Medical expert of the article
New publications
Papillomatosis
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
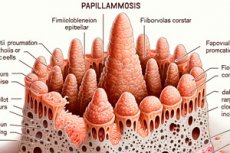
Various skin lesions are caused by dermatologic viral diseases, including papillomatosis. Its characteristic feature is exophytic, i.e. Benign epithelial formations protruding outward: flat or papilla-shaped (Latin rarilla - nipple, papilla + Greek oma - tumor).
Causes of the papillomatosis
Although such skin lesions were described by Hippocrates, their viral origin - thanks to electron microscopy - was finally confirmed by the middle of the 20th century. To date, there are more than two hundred fully sequenced genotypes of HPV (HPV) in the Papillomaviridae family, a species-specific epitheliotropic (Human papilloma virus), at least one third of which types cause papillomavirus infection of the genitals. [1]
Virologists have identified five genera of HPV, and the major ones are alpha, beta and gamma papillomaviruses, with 60-70% similarity between them. Each polygonal viral capsid has a circular double-stranded DNA containing their genome, which is released and replicates in infected epithelial cells of the skin and mucous membranes.
What is the danger of papillomatosis? It is contagious, i.e. Infectious: about 40 types of HPV are transmitted by direct sexual contact or skin-to-skin contact; it is also possible to be infected in the household through objects contaminated with the virus.
But even this is not the main thing. DNA of some types of papillomavirus can integrate into cell chromosomes, which leads to malignant transformation of cells and the development of cancer of various localizations. The group of high oncogenic risk includes the following types of human papillomavirus: 16, 18, 31, 33, 33, 35, 45, 51, 52, 56, 58, 59, 68. In some European countries, the prevalence of high-risk HPV infection among women exceeds 15% and among men is 12%. These HPV types account for up to 35-45% of vaginal and oropharyngeal cancers. And the bulk of cervical, penile and anogenital cancers are associated with hPV type 16 and hPV type 18. [2]
The involvement of papillomaviruses in the development of cervical cancer, the second most common cancer in women, was established by the German virologist H. Hausen (1936-2023), who received the Nobel Prize for it. [3]
HPV types 5, 8, 26, 30, 39, 53, 66, 67, 70, 73, 82 belong to the category of HPV with so-called probable carcinogenicity. And viruses of types 6, 11, 42, 43, 44, 54, 55 do not usually cause malignization of papillomatous epithelial neoplasms.
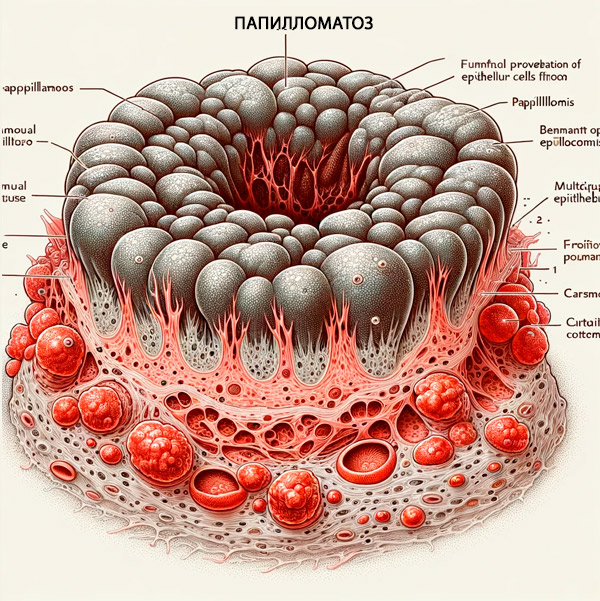
Pathogenesis
Viruses of this family Papillomaviridae infect predominantly proliferating (dividing) cells of mucous membranes and keratinized epithelium whose extracellular matrix has type VII collagen fibrils, especially numerous in multilayered squamous skin cells - keratinocytes. The high collagen content increases signaling of the papillomavirus-activated intraepidermal macrophage enzyme phosphoinositide-3-kinase (PI3K). This enzyme provides cell cycle regulation and promotes cell proliferation and reduces cell apoptosis. In addition, PI3K activation helps the papillomavirus to avoid recognition of the infection by immunocompetent cells (thereby disrupting natural cell-mediated immunity).
Upon entering the target cells through the plasma membrane, HPV releases its genome, where it remains in the form of extrachromosomal nuclear DNA, the autonomous episome (or plasmid), i.e. It does not penetrate the chromosomes of the cell nuclei. Within the affected cells, each viral DNA molecule is doubled by bidirectional theta replication, and the genomes are retained and transmitted to daughter cells.
The mechanism of papillomatosis development is closely related to both the phase of its productive cycle and the terminal differentiation of epidermal cells. The virus replication intensifies as the epithelial cells mature, which explains its adherence to the cells of the superficial layers of the skin, which have significant regenerative potential.
Expression of viral genes (transfer of its amino acid codes) leads to the production of viral proteins by ribosomes of epithelial cells, virus multiplication (assembly of new capsids) and spread of infection. By infecting the epithelium of mucous membranes and keratinized epithelium, the virus triggers proliferation of their cells with the formation of epithelial neoplasia, and, in fact, this is focal epithelial hyperplasia. This is the pathogenesis of benign papillomatosis.
But when the DNA of HPV types of high oncogenic risk integrates with cellular DNA (embedded in the human genome), malignant transformation of the affected cells occurs. In this case, special viral proteins (called oncoproteins, which not all HPV types have) block anti-tumor proteins (p53 and pRb) and disrupt the cell cycle, leading to uncontrolled mitosis and multiplication of atypical (genetically altered) epithelial cells.
Forms
Depending on the localization of the lesion, types of papillomatosis are distinguished.
First of all, it is caused by HPV type 1, hPV type 2, as well as papillomavirus genotypes 4, 7, 22, 27, 29 skin papillomatosis or skin papilloma - formation of verrucae vulgaris, i.e. Common (vulgar) warts. They may also be called viral warts. [4]
Infection of epithelial cells with HPV genotypes 3, 5, 10, 28 or 49 results in flat warts on the face, hands and body.
Papillomatosis of the neck often has the appearance of having a stalk hanging warts.
In two-thirds of cases of papillomatosis in children in the form of papilloma or focal epithelial hyperplasia is the result of HPV 6 and HPV 11 lesions. Read more in the publication - warts in children
When HPV types 5, 8, 9, 10, 12, 15, 19, 36 infect the skin on the hands, forearms, shins, and other parts of the body, a rare condition such as wart-like or verruciform epidermodysplasia Lewandowsky-Lutz. May develop. [5]
A carcinoid papillomatosis of the skin, known as carcinoid papillomatosis of the skin Gottron (or Gottron-Eisenlohr), is a verrucous (warty) carcinoma, a variant of squamous cell carcinoma of the skin and mucous membranes that rarely metastasizes. [6]
Genital papillomatosis
HPVs of different genotypes affecting the genital tract and anogenital region cause benign hyperproliferative masses - acute condylomas, which can be defined as papillomas, viral warts or genital warts. [7]
Papillomatosis of the vulva, vagina, and cervical papillomatosis are caused by different HPV genotypes, and form acute condylomas in women.
Read more:
The formation of small papillomas (papillary mucosal protrusions) in the vaginal vestibule (vestibulum vaginae) in women is diagnosed as vestibular papillomatosis.
In men, penile papillomatosis affecting the shaft, glans, frenulum (frenulum), and urethra is caused by many genotypes of the virus, but most commonly by HPV types 6 and 11. Although it is not uncommon to be affected by HPV with different degrees of risk of malignant transformation (types 31, 35, 51, 56).
Alteration of the epithelium leads to the formation of acute condylomas in men. This is usually multiple papillomatosis - with the presence of several genital warts. It is possible their growth into a giant condyloma Buschke-Levenstein, with inadequate treatment of which destructive processes spread to the skeleton and pelvic organs, leading to death. And in more than half of cases giant condyloma malignant.
Uterine and breast papillomatosis
There is practically no available information about uterine papillomatosis, but gynecologists say that if the virus is present in the cervix, it is possible for it to spread into the uterine cavity - into the endometrium. According to some studies, HPV is detected in endometriosis in 24% of cases, and in malignant uterine neoplasms - in almost 70%.
Papilloma of the mammary gland is localized in its milk ducts (ductus lactiferi) - in the form of a benign formation of epithelial cells with fibrovascular nuclei growing into the duct lumen. Mammologists diagnose it as intraductal or intraductal papillomatosis of the breast, which accounts for 5% of benign neoplasia of this localization. [8]
Central intraductal papilloma (usually as a solitary retroareolar mass) is located in the large milk ducts; peripheral (usually multiple) affects the terminal ducts within the breast lobes and is often discovered incidentally.
Papillomatosis of the oral cavity
Virus-induced papillomatosis of the mouth is characterized by the appearance of the formation of
Squamous cell papillomas, i.e. Warts, which can be located on the root and back of the tongue and are diagnosed as tongue papillomatosis. The same overgrowths of HPV types 6, 7, 11, 16 or 32 characterize papillomatosis of the palate. [9]
Oral acute condylomas, which are associated with HPV genotypes 6, 11, 16 and 18, are most commonly found in young and adult patients and - because they are often found simultaneously on the genitals - are considered a form of sexually transmitted HPV. It is characterized by the presence of several lesions of this type on the soft palate, the frenulum of the tongue and the mucosa of the lips.
HPV types 13 and 32 can cause an asymptomatic benign neoplastic condition of the oral cavity characterized by multiple white to pinkish papules that spontaneously regress over time without treatment.
Gingival papillomatosis in the form of squamous cell papilloma of the gingiva is a benign, asymptomatic, exophytic formation on the mucosa; it can affect several areas of the oral cavity. Pathological formation can also occur on the epithelium forming the wall of the gingival pocket: its epitheliocytes multiply rapidly, the tissue is characterized by friability and numerous intercellular spaces, which facilitates the penetration of the virus through the basal membrane. As clinical practice shows, the gingiva is the most frequent site of HPV infection with the threat of squamous cell carcinoma of oropharynx (with HPV type 16). [10]
The papilloma virus infects the tissues of the oropharyngeal region - tonsillar crypts (recesses of the mucous membrane of the palatine tonsils), as well as the lingual tonsil, causing papillomatosis of the tonsils.
Respiratory papillomatosis
Laryngeal papillomatosis, also defined as laryngeal papillomatosis, [11] recurrent respiratory papillomatosis, or vocal cleft papillomatosis, is most commonly caused by HPV type 6 and type 6 and HPV type 11 (although genotype 16, 18, 31, and 33 viruses may be associated). It is a rare disease in which papillomas form along the respiratory tract (oropharynx, larynx, and pharynx), pulmonary tract (trachea, bronchi, and lungs), and upper digestive tract (esophagus). Depending on the age of onset, there are two variants of the disease: juvenile papillomatosis, which occurs in childhood, and adult papillomatosis of the larynx.
Recurrent or recurrent papillomatosis of the larynopharynx and larynx in children is a rare and serious condition: papillomas can lead to airway narrowing with voice changes or airway obstruction. Most patients with this condition will require repeated surgical procedures to maintain airway patency.
HPV genotypes 6 and 11 cause the formation of pulmonary squamous cell papillomas (with a fibrovascular nucleus covered with epithelium) of a benign nature - pulmonary papillomatosis. Specialists note that it occurs mainly in children who are infected from an infected mother during vaginal delivery.
Malignant transformation in lesions of papillomavirus types 16, 18 and 31 is rarely observed.
Papillomatosis of other localizations
Papillomatosis of the bladder - inverted urothelial papilloma (associated with HPV types 6 and 11) or Ringer's tumor - is a rare non-invasive tumor of the urothelium lining the bladder, the prevalence of which is less than 1% among neoplasms of this localization. The papilloma is called inverted because hyperplastic epithelial cells sprout downward into the underlying supporting tissue. [12]
Squamous cell papilloma of the esophagus in the form of a single wart-like mass - esophageal papillomatosis - develops in its middle or distal part when affected by HPV type 58. It is an extremely rare epithelial neoplasm in this area. [13]
When the epithelial cells of the skin in the area of the external opening of the rectum (anus) are damaged by HPV 6, 11, 21, 42, 44, etc. With the appearance of anogenital warts, anus papillomatosis is diagnosed. [14]
Eyelid papillomatosis is papilloma of the conjunctiva, that is, the inner mucous membrane of the eyelids. It can also be papillomatosis of the nasal passages.
More information in the article - symptoms and diseases caused by the human papillomavirus
Diagnostics of the papillomatosis
Diagnosis (which begins with examination of patients and collection of anamnesis) is carried out by specialists - dermatologists and dermatovenerologists, gynecologists, ENT doctors - depending on the site of papillomatosis.
To be sure of the presence of the virus (and to determine its genotype) laboratory tests are mandatory, read more:
- Human papillomavirus tests
- Papillomavirus infection: detection of human papillomavirus (PCR genotyping)
A skin biopsy with histologic examination of the biopsy, analysis of cervical smear by Papanicolaou (PAP-test), cervical cytology, etc. Is performed.
Instrumental diagnostics in dermatology includes dermatoscopy and ultrasound examination of the skin; in gynecology - colposcopy, ultrasound of the pelvic organs and uterus, mammography; in otolaryngology - laryngoscopy, etc.
Differential diagnosis
Differential diagnosis should exclude: Molluscum contagiosum, verrucous nevus (warty convex mole), seborrheic keratosis (seborrheic and senile wart, keratoma), verrucous form of Darier-White disease, lenticular hyperkeratosisPhlegel's disease, verrucous porokeratosis, papillary hydradenoma of the skin (benign formation of sweat glands), superficial limited lymphangioma, basalioma, genital wide condylomas (similar to warts) in the secondary phase of syphilis, hirsutoid papillomas - pearly papules of the penis.
It should be borne in mind that the term "papillomatosis" appears in the names of nosological forms, etiologically unrelated to HPV, that is, it is not viral papillomatosis, but the designation of a small dense elevation of the skin by transliteration of the Latin word rapilla (nipple). In dermatology, nodules on the skin of dense consistency are called papules: from Latin papula - bulge.
So papillomatosis in psoriasis refers to an epidermal syndrome with an increase in the length and width of the papillae of the papillary or papillary layer of the skin (papillaris iacuit pellis), which is immediately below the epidermis and is composed of loose connective tissue.
There is such a disease of unknown etiology as lymphostatic papillomatosis - with the appearance of numerous papules on the back of the feet, toes and shins, which give the epidermis a warty appearance; there is also a general thickening of the skin (pachydermia). These skin changes are considered to be a consequence of long-term lymphostasis - impaired lymphatic outflow in the lower extremities. Experts call the pathology elephantiasis nostras verrucosa - warty elephantiasis of the legs, which is a rare form of chronic lymphedema with cutaneous hypertrophy.
But plum reticular or plum reticular papillomatosis - Gugero-Carto syndrome (disease) or plum reticular erythrokeratoderma Gugero-Carto - is caused by a violation of keratinization (keratinization) of the skin. Among the versions of the causes of its development are: infection by fungi of the genus Malassezia; infection of the skin by bacteria of the genus Dietzia - Gram-positive aerobic actinomycetes Dietzia papillomatosis; exposure to UV radiation, etc.
Who to contact?
Treatment of the papillomatosis
A detailed description of papillomatosis treatment methods, drugs used in drug therapy (names, forms of release and methods of their use) is given in the following publications:
- Human papillomavirus treatment
- Ointments for papillomas
- Ointment for condylomas
- HPV - human papillomavirus suppositories
- Overview of effective treatments for acute condylomas
- Wart treatment
- Ointments for warts
Doctors can prescribe courses of various physiotherapy procedures, for example, ozone therapy is used for papillomatosis of the larynx, oral cavity, vagina of the uterus (in insufflations) or for papillomatosis on exposed skin (in the form of applications).
Used and folk remedies for human papillomavirus. For example, it is recommended to apply on papillomas and condylomas celandine or garlic juice, paste of baking soda, etc. You can also use aloe extract for papillomatosis, because the biologically active substances contained in aloe vera have antioxidant, anti-inflammatory and healing effects.
Surgical treatment is performed to radically get rid of papillomas, condylomas and warts. In addition to excisional surgery (using traditional instruments), removal of acute condylomas is performed by electrocoagulation, radio wave surgery, destruction by laser or liquid nitrogen.
There is a papillomatosis vaccine, Cervarix, to protect against HPV genotypes 16 and 18. The Gardasil-4 vaccine protects against HPV types 16, 18, 6, and 11, and Gardasil-9 can protect against papillomavirus types 6, 11, 16, 18, 31, 33, 45, 52, and 58. For girls and women, human papillomavirus vaccination can be given from age 9 to 45, and for boys and men from age 9 to 26.

