Medical expert of the article
New publications
HPV 16 oncogenic type: how it manifests, treatment with drugs and folk remedies
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
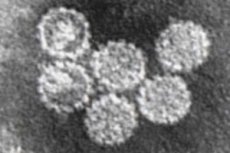
All one hundred and fifty strains of the human papillomavirus (HPV) have a digital designation. If most of them cause the growth of warts on different parts of the body and belong to the HPV serotypes of low risk of malignancy, then HPV type 16 (and more than a dozen strains) is considered carcinogenic and is defined as a high-risk serotype.
Structure HPV type 16
The icosahedral nucleocapsid of the papilloma virus contains fragments of double-stranded DNA, for the replication of which it needs foreign proteins. HPV gains access to them by penetrating human cells through endocytosis of the cellular receptor, and forms its shell from proteins of cellular membranes. At the same time, the virus type 16 is characterized by integration into the cell genome, and penetration into its nucleus is a necessary condition for replication. But if a person's immunity is strong enough, the virus remains in the cell in the so-called episomal form.
Replication of HPV 16 occurs in the epidermis, more precisely, in the basal cells of the stratified squamous epithelium of the stratum corneum of the skin and the cells of the squamous non-keratinizing epithelium of the mucous membranes, in which the process of cellular mitosis and migration constantly occurs. Obviously, a favorable factor for this virus is also the looser intercellular matrix of the epithelium of the genitals, perineum and perianal area, as well as local increased humidity.
In addition, the cells of the superficial epithelium of the indicated areas are often subject to microtrauma (abrasions), and many specialists are sure that HPV 16 damage and its activation occurs only when the epithelial barrier is damaged. Moreover, being an opportunistic infection, HPV takes advantage of the fact that cellular immunity can be significantly weakened by bacteria often present in the anogenital area, in particular when chlamydia or ureaplasma and HPV 16 are combined, as well as other viral infections, such as herpes viruses.
HPV-induced pathogenesis of malignancy consists of the interaction of primary viral oncoproteins E6 and E7 with the nuclei of anti-oncogene cells (tumor suppressor proteins p53 and pRb), which causes these cells to degrade and stop performing their protective function. Then the neoplastic process begins: the cell cycle changes, control over cell growth is lost, the rate of their proliferation increases, and mutations occur in cell structures. Ultimately, this leads to the development of dysplasia or tumor.
Pathogenesis
HPV is an epitheliotropic DNA virus of direct action, that is, when penetrating into an epithelial or mucous membrane cell, the virion integrates into the human cell genome and combines with it, forming a special latent form. In this form, it can remain in cells for a very long time without causing any symptoms (for more details, see below – in the Pathogenesis section).
HPV infection is very common, but in 80-90% of people the immune system is able to cope with it on its own, and a person may not even suspect that he was infected with this virus.
But sometimes the virus reveals its presence openly. More than 30 strains affect the mucous membranes of the urogenital tract and the epidermis of the anogenital area. Thus, low-risk serotypes (HPV 6, 11, 42, 43 and 44) can cause genital warts, often affecting the perianal area; they can also provoke the development of respiratory papillomatosis. And the highest-risk serotypes – HPV 16, 18, 31, 45 – are associated with cervical lesions with a high probability of developing into cervical cancer.
Therefore, how HPV 16 is transmitted is clear: it is sexually transmitted, that is, sexually (including all types of sexual contacts). Moreover, latent HPV, even without external signs, is also transmitted to a sexual partner. And unprotected sex increases the likelihood of infection by 75%. As a rule, two thirds of people who have sexual contact with a partner infected with the papillomavirus may develop genital warts within two to three months.
How is HPV 16 transmitted?
Although sexual intercourse is not the only way HPV can be spread: all its serotypes are extremely contagious and can be transmitted by contact with infected mucous membranes or skin. Presumably, the infection can spread from one part of the body to another: gynecologists believe that the virus can first affect the cervix and then spread to the vagina and vulva.
A natural question arises: is HPV 16 transmitted through saliva? Viruses associated with benign and malignant lesions of the skin and mucous membranes cause papillomas of the oral cavity, and in at least 90% of cases, HPV type 16 is involved in the development of oropharyngeal cancer - squamous cell carcinoma of the throat. So virologists believe that saliva can play a certain role in the transmission of infection. Although specialists from the American Cancer Society claim that this virus is not spread through any biological fluids.
The main risk factors for HPV 16 infection include weakened immunity, early onset of sexual activity, multiple sexual partners, decreased pH (acidification) of the body, and the presence of inflammatory diseases of the genital area. Smoking and long-term use of oral contraceptives also reduce resistance to papillomaviruses.
 [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ]
[ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ]
Incubation period
The incubation period after infection with dermatotropic HPV serotypes – with manifestation as papilloma or genital warts – varies from several weeks to a year. However, most warts appear after two to three months.
With oncogenic papilloma viruses, everything is much more complicated. The incubation period for HPV 16 - for signs of malignant transformation of cervical cells to begin to appear - is quite long. Studies have shown that the average incubation period from the initially detected HPV 16 to the diagnosed low-differentiated dysplasia (intraepithelial neoplasia) of the cervix is 5 years, and to cervical carcinoma in situ - 12-15 years.
It is believed that this virus can remain in a latent or persistent state even longer, which increases the likelihood of infecting sexual partners throughout their lives. And how long people live with HPV 16 depends on whether it manifests itself, provoking the development of cancer, or not. But the very presence of this virus - with asymptomatic or subclinical existence in the body - does not affect life expectancy in any way.
It is important to keep in mind the widespread latent carriage of HPV 16, which can only be detected by partial genotyping using polymerase chain reaction - when the patient takes an STD test. In such cases, according to several foreign studies, the positive result of asymptomatic presence of the virus can be 27-44%.
Epidemiology
By some estimates, 50 to 80% of men and women of sexually active age will become infected with HPV sooner or later…
According to the latest WHO data, two thirds of all cases of precancerous pathological conditions and cervical cancer are caused by HPV types 16 and 18. And experts from the American Cancer Society say that this type of virus is detected in 90% of patients with this diagnosis.
The CDC statistics provide the following official figures: in the United States, 6.2 million new infections with all types of HPV occur annually; currently, 79 million Americans are infected with the papillomavirus, of which 20 million are infected with the HPV 16 virus, and these are people of reproductive age. Up to 20% of patients with genital warts and condylomas have other sexually transmitted diseases.
The prevalence of HPV 16 in women (about 18%) is twice as high as in men (8%).
According to the Journal of Virology, about 12,000 Americans aged 15 to 24 become infected with HPV every day. Of these, approximately 0.1% are HPV type 16.
Also, this virus (in combination with HPV 31) in 23-25% of cases is a trigger for a subset of squamous cell carcinomas of the mouth and pharynx.
 [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ], [ 26 ]
[ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ], [ 26 ]
Symptoms
If the papillomavirus does not manifest itself in most people, then there are no symptoms of HPV 16. When a persistent infection is activated, its first signs most often look like benign epithelial neoplasia - papillomas and condylomas. Pointed condylomas of different sizes and shapes in women can appear on the external genitalia, in the vagina, on the cervix, in the perineum, outside and inside the anus.
Diseases caused by HPV 16
Gynecologists draw the attention of their patients to the fact that any discharge with HPV 16 in women appears only in cases of its activation and development of diseases (see below), and the nature of the discharge depends on many additional factors. And a latent infection never leads to the appearance of pathological vaginal discharge.
Localization of pointed condylomas in men: on the foreskin and head of the penis, on the scrotum, in the urethra, around and inside the anus. Condylomas can also appear on the mucous membrane of the oral cavity, nasopharynx or larynx.
The consequences and complications of HPV 16 in clinical practice are defined as diseases caused by HPV 16. And this corresponds to the pathogenetic principles of medicine. In addition, sexual life with HPV 16 in both women and men is often difficult and can cease due to serious health problems.
Thus, HPV 16 in women can lead to the development of such pathologies as:
- cervical erosion;
- endocervicitis;
- cervical dysplasia;
- cervical cancer;
- vulvar cancer;
- vaginal cancer;
- anal cancer (most often found in HIV-infected people);
- leukoplakia of the oral cavity (including proliferative warty leukoplakia);
- squamous cell carcinoma of the throat (oropharyngeal cancer).
HPV 16 in men can provoke the development of:
- urogenital and anal papillomas;
- condyloma of the rectum;
- squamous cell carcinoma of the penis;
- warty (verrucous) carcinoma of the penis;
- penile skin cancer - Bowen's disease;
- erythroplasia of Queyrat;
- squamous cell anal cancer (among patients with this oncological disease, the largest number are people with immunodeficiency syndrome and homosexuals).
Also, one of the most common HPV 16 lesions in men are tumors that occur at the root of the tongue, on the back wall of the larynx and on the pharyngeal tonsils.
HPV 16 in children appears as a result of transmission from the mother during childbirth, but the development of associated genital diseases is rare. However, the absence of any signs does not exclude asymptomatic latent infection, since the virus can hide for decades.
Most often, the defeat of this type of HPV of the mucous membranes of newborns manifests itself as papillomas in the trachea, bronchi and lungs - respiratory papillomatosis. These papillomas can also grow on the vocal cords, causing laryngeal papillomatosis.
 [ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ]
[ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ]
HPV 16 and pregnancy
HPV infection does not reduce fertility and does not directly affect the ability to conceive, and gynecologists give an affirmative answer to the question of whether it is possible to get pregnant with HPV 16.
True, when a viral infection causes changes in the cervix, they should be treated. This applies to both planned normal conception and IVF for HPV type 16. Doctors recommend postponing pregnancy until treatment is complete.
It is also necessary to take into account the fact that – against the background of physiologically conditioned immunosuppression and increased blood flow and number of vessels in the genital area – genital warts during pregnancy (especially between 12 and 14 weeks) can grow faster and cause irritation or other symptoms (swelling, pain, burning, bleeding, problems with urination).
The risk of transmitting HPV to a child is extremely low, and simply because of the presence of the virus in a pregnant woman, a cesarean section is not recommended. Therefore, the answer to the question - is it possible to give birth with HPV 16 - is also affirmative.
Diagnostics
Detection of papillomavirus in the body, that is, diagnosis of HPV 16, is possible only by microbiological molecular methods.
HPV tests include a qualitative test performed by examining a vaginal or cervical smear (taken by a gynecologist) using the polymerase chain reaction - HPV PCR; at the same time, a quantitative analysis for HPV 16 is done - PCR/HPV VCR.
The norms of HPV type 16 are relative, since the viral load of HPV 16 is determined by the numerical expression of the number of live virions (more precisely, copies of HPV DNA or markers of their genomes - Lg), per 10 5 (100 thousand) cells of biological material. The higher their number, the higher the activity of the infection and the viral load:
- viral concentration (i.e. the probability of oncology with the development of the diagnosed pathology) is very high – 5 Lg and higher;
- the number of viruses has clinical significance (in the diagnosis of an etiologically related disease) – range from 3 to 5 Lg;
- low viral concentration – below 3 Lg;
The PCR genotyping method identifies the specific type of papillomavirus, i.e. its DNA is determined in comparison with reference (standard) samples. The test may be designated PCR HPV 16/DNA HPV 16. The biological material for this analysis is a scraping from the mucous membrane of the cervix or its canal. Its significance is that the oncogenic virus can be determined before the PAP test (Papanicolaou smear) can detect any abnormal cells of the cervix.
Treatment
The first and main question is whether HPV type 16 can be treated? The second and also important question is what to do with HPV 16?
There is no radical therapy for the papillomavirus, since there is nothing yet to rid the body of its presence, and only diseases in the development of which this type of HPV is involved can be treated.
In 2012, European guidelines for the treatment of anogenital warts (condylomata acuminata) were published, and it was emphasized that only surgical treatment (surgical removal of papillomas and condylomas) gives a positive result in almost all patients.
In addition to surgical resection of neoplasia, hardware methods are used: radio wave excision, diathermocoagulation, laser ablation, cryodestruction. Read more in the material - Removal of genital warts
And cauterization of erosion with HPV 16 is carried out in the same way as in the absence of this infection, see - Cauterization of cervical erosion
Algorithms and existing schemes for treating HPV 16 include drug therapy. Below are the main drugs that are most often used in clinical practice today.
To reduce the oncogenic load and activate cellular immunity (T-lymphocytes, macrophages, dendritic cells, etc.), immunomodulators are prescribed for HPV 16 - drugs containing interferon or its analogues.
The drug Alloferon or Allokin alpha stimulates the synthesis of endogenous leukocyte α-, β- and γ-interferons. It is administered subcutaneously - 1 mg every two days. In total, such injections for HPV 16 are given no more than nine times (most often, they are limited to six injections), but if necessary, after a break, the course of treatment can be repeated. This drug is not used for children, pregnant and lactating women, as well as in the presence of autoimmune diseases.
The immunomodulatory drug Isoprinosine (other trade names are Pranobex, Groprinosin, Inosine, Novirin) is prescribed two tablets (0.5 g each) three times a day for two to four weeks. The drug can cause side effects such as decreased appetite, headaches and joint pain, nausea, abdominal pain, and intestinal disorders. Its contraindications include chronic renal failure, bladder stones, pregnancy and breastfeeding.
Cycloferon (Neovir) induces the production of interferons due to the action of acridoneacetic acid. It is available in the form of tablets, injection solution and liniment. Tablets are used one or two times a day (before meals) for three weeks. A course of injections (intravenously or intramuscularly) is prescribed for severe lesions, usually one injection per day. The drug is not used for liver cirrhosis and pregnancy. The liniment is used locally: by instillation into the urethra or vagina.
The means that enhance immunity also include Polyoxidonium (Azoximer bromide) - lyophilisate for the preparation of a solution (for intramuscular and intravenous administration), vaginal suppositories -
Adults (except pregnant women) are given injections for HPV 16 twice a week or every other day (one injection in a single dose of 6 mg). For children, the dose of Polyoxidonium is determined at the rate of 0.1 mg per kilogram of weight; administered once a day, the course of treatment is 7-10 injections. Vaginal suppositories are used in the evening (before bedtime - one suppository per day for ten days).
But the drug Amiksin is used to prevent influenza and reduce the symptoms of acute respiratory viral infections, but is not prescribed for DNA viruses.
Panavir suppositories, gel and injection solution contain potato sprout extract: the product is declared as an antiviral and at the same time immunomodulatory (not registered in the International Pharmacopoeia).
The dietary supplement Promisan with green tea extract, which, according to the description, is recommended for the prevention of cancer, as well as Indinol (Indole-3-carbinol), which contains indole derivatives obtained from broccoli, are not considered drugs.
Externally - for small superficial anogenital condylomas - use Podophyllotoxin solution (Podofilox, Condyline), as well as Keravort cream (Imiquimod) - once a day every other day (at night), for a month; if repeated courses of treatment are necessary, a break should be taken. Both drugs are contraindicated for children and pregnant women.
A very common remedy for local use is vaginal and rectal suppositories for HPV 16:
Genferon (with α2-interferon) – one suppository intravaginally (for men – rectally);
Viferon (with interferon, vitamins C and E);
Vitaferon (with interferon and vitamin C), etc. More information in the article - Suppositories for HPV
But vaginal capsules (not suppositories) Polygynax are intended for the treatment of candidiasis and bacterial infections of the vagina; they are useless against viruses.
Folk treatment of HPV 16
What does folk treatment for HPV 16 recommend? Garlic and iodine cauterization of condylomas; lubrication with propolis tincture with the addition of fresh onion juice; applications with a concentrated solution of baking soda or tincture of green walnut peel on kerosene.
It is claimed that externally applied hydrogen peroxide against HPV 16 or 10% aqueous ammonia solution (ammonia) can help.
You can also try herbal treatment, for example, lubricating warts with celandine (fresh juice) 5-6 times a day. And since researchers have identified the immunoregulatory activity and ability to increase interferon synthesis of one of the licorice species - Glycyrrhiza uralensis, they recommend taking an aqueous extract of the root of this plant. In addition, licorice contains glycyrrhizic acid, which stops the growth of pathogenic bacteria and viruses.
Prevention HPV type 16
Prevention is better than cure. Therefore, sex education should be correct, and sexual contacts should be orderly and protected…
Fortunately, there is a vaccine against HPV 16 and 18: Gardasil (manufactured by Merck) and Cervarix (GlaxoSmithKline). These antiviral vaccines are effective in blocking HPV penetration into the cervical epithelium by generating HPV-specific neutralizing antibodies. But, alas, they cannot destroy the virus that has already penetrated. See also – Vaccination against human papillomavirus (HPV)
Doctors recommend vaccinating girls aged 9-13 and young women up to 26 years. By the end of 2012, HPV vaccination had been introduced in 45 countries. And in 2013, Australia began vaccinating teenage boys.
But it is important to realize that the vaccine will not prevent all cases of cervical cancer. So adult women should definitely undergo gynecological screening examinations.
Forecast
Having HPV type 16 does not mean you have cancer: Up to 90% of people infected with high- or low-risk HPV clear the infection within about two years.
In 30% of cases in women, genital warts spontaneously regress within four to six months. It is not entirely clear whether this immune-mediated regression eliminates the infection or simply suppresses it for a long time. But in any case, the virus stops manifesting itself.
However, each newly acquired infection can persist as an incurable lifelong disease, leading to a significant increase in the long-term risk of cancer for patients and their sexual partners. Many of these HPV 16-related cancers may not become apparent until decades later.
The question arises: how to live a normal life with HPV 16? Doctors advise to monitor your health and maintain immunity.

