Medical expert of the article
New publications
Cervical dysplasia
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Cervical dysplasia is a clear change in the number and morphological structure of cells in individual sectors of the mucous membrane of the cervix uteri. This condition of the epithelium is considered dangerous due to the high risk of developing an oncological process, but with timely diagnosis and treatment, the pathology is reversible. Cervical cancer ranks third among the most common diseases in women. According to statistics collected by the WHO, cervical dysplasia as a precancerous pathology is diagnosed annually in more than 40 million representatives of the fairer sex. In modern gynecological practice, cervical dysplasia as a diagnosis is replaced by the definition - CIN (Cervical intraepithelial neoplasia), or cervical intraepithelial neoplasia.
 [ 1 ]
[ 1 ]
Causes cervical dysplasia
According to the latest WHO data, 90% of cervical dysplasia causes are associated with a viral infection. Most often, it is HPV - human papillomavirus, the DNA of this virus is detected in almost every study, regardless of the severity of cervical dysplasia. However, etiologically, CIN can also be provoked by other factors, including the following diseases, conditions and circumstances:
- Human papillomavirus (HPV)
- HSV-2 (HSV2) - herpes simplex virus, type 2
- Cytomegalovirus (CMV) - cytomegalovirus
- Gardinella, an anaerobic bacterial infection (Gardnerella vaginalis)
- Vaginal candidiasis (Candida spp)
- Urogenital infection - mycoplasmosis (Mycoplasma hominis)
- Chlamydia (Chlamydia trachomatis)
- Long-term use of hormonal contraceptives
- Promiscuous sexual relations, indiscriminate choice of sexual partners
- Beginning sexual activity before reaching adequate sexual maturity (12-14 years)
- History of genetic oncofactor
- Immunodeficiency, including HIV
- Chemotherapy
- Alimentary pathologies associated with malnutrition, deficiency of microelements and essential vitamins
- Frequent births or, on the contrary, abortions
- Unhealthy habits - smoking, alcohol addiction
- Antisocial lifestyle, insufficient level of basic hygiene
It should be noted that cervical dysplasia is most often associated with STDs - sexually transmitted diseases, the leader among them is Human Papillomavirus - papillomavirus. This is the most common cause of precancerous diseases in women, so it is worth considering in more detail.
HPV is divided into the following categories according to the degree of risk of developing cancer:
- Pointed condylomas, warts, non-oncogenic nature
- Low oncogenic risk (oncogenic serotype 14 species)
- High risk of developing cancer
The danger of such etiological factors lies in the asymptomatic progression of the disease. It is almost impossible to notice the onset of developing pathology without regular gynecological examinations. More than 10 years can pass from the onset of infection to the stage of obvious oncological process. Infection threatens many women, but those who fall into the risk category are most susceptible to it. These are ladies leading a free lifestyle in the sexual sense, as well as those who do not use contraception when changing sexual partners. In addition, women who are negligent about any inflammatory processes in the genitourinary sphere are at risk of becoming infected with HPV. A small percentage of infection occurs in cases of traumatic injuries to the cervix during termination of pregnancy.
An interesting version of the causes that contribute to the development of cervical dysplasia was put forward by the American gynecologist Polikar. The "weed theory" explains CIN in this way:
- The epithelial covering of the cervix is a kind of soil
- Viruses and bacteria can enter the “soil”, causing changes in tissue cells
- In order for the “seeds” to begin to grow and provoke pathology, they need certain conditions
- Conditions for pathological growth of "seeds" are heat, humid environment, dirt, light
- The following factors play a role in the conditions for the development of pathology growth:
- immunodeficiency
- vitamin deficiency and micronutrient deficiency
- failure to observe hygiene rules
- bad habits
- genetic factor
The hypothesis of the doctor from the University of California is not yet rejected, but it is not accepted as an axiom, however, clinical observations indicate a certain reliability of the "weed theory". Women who were diagnosed with cervical dysplasia were treated in the doctor's clinic. In 45% of them, after quitting smoking, receiving normal vitamin-rich nutrition and immunomodulators, the results of PAP tests and histological scrapings improved. 25% of patients were completely cured of HPV after a year.
Pathogenesis
Cervical dysplasia is pathogenetically most often associated with infection with HumanPapillomavirus, the human papilloma virus. In the practice of gynecologic oncologists, it is customary to consider two types of viral infection development:
- The first stage – the DNA of the papilloma virus is already in the cell, but does not penetrate its chromosome (episomal state). This type of infection is considered reversible and easily curable in terms of treatment
- The second stage, when the DNA of the papillomavirus is already in the cell genome. This variant of infection can be called the first step towards the development of pathological transformation of cells. At the same time, the birth of a specific estrogen (16α-ONE1) with an aggressive form of development, which has a carcinogenic effect, is induced. These are ideal conditions for the formation of a tumor process.
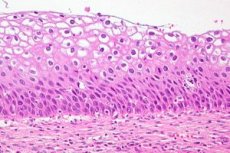
In general, the pathogenesis of cervical dysplasia is associated with the transformation of the cellular structure of the tissue. The epithelial tissue of the cervix has certain properties:
- Structure (4 layers)
- Standards of cell nuclei size
- Cellular contact mode
Also, epithelial tissue may have different structures depending on its location. The endocervix is located inside the uterus, it is glandular tissue (single-row cylindrical epithelium). The outer layer of the epithelium (vaginal) is a flat epithelium with many layers (SPE). The layers of the multilayered epithelium are divided into the following types:
- Initial, germinal (basal low-differentiated cells)
- The layer that is capable of actively dividing and multiplying is the parabasal layer.
- An intermediate, spiny layer of differentiated cells with clearly expressed cytoplasm. This is the protective layer of the epithelium.
- The layer that can peel off is superficial. This layer is subject to keratinization.
Pathogenetically, cervical dysplasia is most often associated with a disruption in the structure of the basal and parabasal layers (hyperplasia). The changes affect the following processes:
- The division of nuclei, their sizes and contours are disrupted
- The cells are poorly differentiated.
- The normal stratification of the epithelium is disrupted
The pathology can develop over the years until the integrity of the basement membrane is compromised, which in turn leads to cervical cancer (invasive form).
Currently, thanks to regular screening programs (gynecological examinations), most women have the opportunity to stop the development of atypical cells at early stages. Mild and moderate cervical dysplasia is successfully treated and is not a life-threatening disease. Severe dysplasia is most often associated with the refusal of patients from the risk group to comply with the rules of preventive examination and adequate therapy.
Symptoms cervical dysplasia
Symptoms of CIN are characterized by their "secrecy". Cervical dysplasia is dangerous because it occurs without obvious, noticeable clinical manifestations. It is almost impossible to see the clinical picture in time without examination, especially in the early stages of the disease. The pathology develops absolutely asymptomatically in 10-15% of women, the rest of the category of patients has the opportunity to stop the process thanks to regular examinations by the attending gynecologist.
It should be noted that CIN rarely occurs as an independent disease; it is usually accompanied by bacterial and viral infections:
- HPV
- Colpitis
- Chlamydia
- Herpes infection
- Cervicitis
- Leukoplakia
- Adnexitis
- Candidiasis
Symptoms of cervical dysplasia may not be the true causes of the CIN process itself; signs are usually caused by concomitant diseases and may be as follows:
- Itching in the vagina
- Burning sensation
- Discharge that is not typical for a healthy state, including blood
- Pain during intercourse
- Pulling pain in the lower abdomen
- Visible condylomas, papillomas
Cervical dysplasia is not an oncological disease, but due to the latent clinical picture it is considered quite dangerous, prone to progression, and in severe form can lead to cervical cancer. Therefore, the main way to promptly detect asymptomatic changes in the epithelial cover of the cervix is considered to be examination and diagnosis.

First signs
Latent course of CIN is a characteristic clinical picture for all types of cervical dysplasia.
The first signs that may manifest the disease are most likely associated with the presence of signs of associated pathologies or initially provoking factors.
Most often, cervical dysplasia is etiologically caused by HPV infection.
According to statistics, every ninth inhabitant of the planet is a carrier of one of the 100 varieties of human papillomavirus. Many types of HPV go away on their own due to the activity of the immune system, some of them are prone to recurrence and can manifest themselves as follows:
- Warts in the genital area (they are detected during a gynecological examination)
- Pointed condylomas are visible growths with jagged edges in the vagina and anal area. Internal condylomas are only visible during an examination in the doctor's office.
- Occasional light bleeding after intercourse, especially in the middle of the monthly cycle
- Discharge that is unusual in color, odor, consistency
- Irregular monthly cycle
The first signs may be absent, everything depends on the type of HPV, the protective properties of the immune system. This is a serious threat, since cervical dysplasia can proceed as a hidden process for many years. The erased clinic of CIN as a risk factor can only be prevented with the help of examinations, screening. Doctors recommend that all women after 18 years visit a gynecologist and undergo diagnostics - both clinical and instrumental, laboratory.
 [ 15 ]
[ 15 ]
Discharge in cervical dysplasia
Discharges that could indicate cervical dysplasia are most often detected during examination on a gynecological chair or when taking material for cytology. A certain amount of mucous fluid may be released from the cervical canal. Its properties and characteristics are determined not by CIN itself, but rather by concomitant, associated infections, most often bacterial or viral. Also, discharges with cervical dysplasia can be associated with erosive processes. A little more detail about the specific signs of discharge:
- Abundant, white and thick discharge takes the form of flakes and has a characteristic odor. These are signs of colpitis, which may accompany cervical dysplasia
- Scanty discharge mixed with blood or pus may be a sign of erosive processes, especially if they appear after sexual intercourse.
- Discharge accompanied by itching, pain, burning are a sign of a viral or bacterial infection, most often associated with STDs (sexually transmitted diseases)
- Discharge, the amount of which increases in the 2nd half of the cycle, with acute itching, burning - a symptom of genital herpes. It in turn is a factor that provokes cervical dysplasia
- Bloody discharge, heavy or scanty, is a dangerous sign. CIN in the third stage is characterized not so much by pain as by the properties of the fluid secreted from the vagina.
In order to determine the cause of the discharge, in any case, one examination is not enough, bacteriological culture, cytology and other laboratory tests are required. If you go through all the stages of diagnostics in time, the process can be stopped at the initial stage and prevent the development of pathological transformations in the cells of the cervical epithelium.
Pain in cervical dysplasia
Pain in cervical intraepithelial neoplasia is a threatening symptom that may mean that cervical dysplasia has already progressed to stage III. CIN of the first two stages is considered a background disease and does not relate to oncological processes. As a rule, dysplasia occurs without noticeable clinical signs, there may be minor symptoms (discharge, itching) characteristic of concomitant diseases.
In what cases can pain occur with cervical dysplasia?
- All inflammatory processes associated with the pelvic organs - PID:
- Acute endometritis - pain is accompanied by fever and chills
- Oophoritis, unilateral or bilateral, is often of infectious origin (mycosis, candida, everything related to STDs). Inflammation in the ovaries causes pain in the lower abdomen, often with discharge.
- Endometritis in the acute phase - pain in the lower abdomen
- Myometritis - pain, bloating, fever
- Salpingitis manifests itself with painful symptoms at the end of the menstrual cycle
- Adnexitis in the subacute or acute course of the process is accompanied by severe pain
PID - inflammations associated with the pelvic organs are etiologically caused by infections, viruses, and bacterial lesions. It is this "base" that is considered favorable for the development of cervical dysplasia as a consequence of an advanced disease.
- Cervical dysplasia, progressing to stage III, when two thirds of the epithelial layers are subject to changes. The pain symptom lasts for quite a long time, is of a pulling nature, often with discharge (blood, odor, atypical consistency). Pain can appear even without a stress factor, at rest, and is rarely cutting or acute. In such cases, a preliminary diagnosis is made - cervical cancer, requiring specification (localization of the process, degree of damage)
Most often, pain in CIN is a clinical manifestation of factors that provoke dysplasia. These include, first of all, viral infections (HPV) and almost the entire range of sexually transmitted diseases (STDs).
Where does it hurt?
Stages
Modern practitioners use a new classification developed by WHO. Cervical dysplasia is defined as CIN of three degrees depending on the severity of the process:
- The changes in the cellular structure are minor. This is low-grade dysplasia or CIN I. The diagnosis needs to be clarified with laboratory tests and screening examination.
- The cellular structure of the epithelium is subject to pronounced transformation. This is cervical dysplasia of moderate severity or CIN II.
- The typical picture for CIN III is visible pathological changes in two-thirds of the epithelial layers. The morphology and functions of the cells are clearly impaired, this stage is diagnosed as severe (severe CIN). This may not yet be cancer, but the diagnosis is defined as the border between carcinoma in situ and an advanced form of oncology.
Cervical dysplasia should not be confused with another nosology - erosion. According to the ICD 10 classification, erosion is a defect of the epithelial cover, recorded in class XIV under code N 86. The terminological definition of "cervical dysplasia" was adopted back in 1953, then at the First Congress of Exfoliative Cytology in 1965 this term was approved. Ten years later, in 1975, another international forum was held (II Congress on Pathological Changes in the Cervical Cervical Diseases).
It was decided to call cervical dysplasia Cervical Intraepithelial Neoplasia (CIN). or CIN. Cervical intraepithelial neoplasia as a diagnosis was divided into 3 degrees:
- 1st degree – mild.
- 2nd degree – moderate.
- Grade 3 – severe, carcinoma in situ (initial, preinvasive stage) added.
In the generally accepted classification ICD 10, the diagnosis of cervical dysplasia is recorded as follows:
1. Class XIV, code N87
- N87.0 – mild cervical dysplasia, CIN grade I.
- N87.1 – moderate cervical dysplasia, cervical intraepithelial neoplasia (CIN) grade II.
- N87.2 - overt cervical dysplasia NOS (CIN not elsewhere specified), not elsewhere classified. This code excludes CIN grade III.
- N87.9 – CIN - unspecified cervical dysplasia.
Carcinoma in situ is designated by the code D06 or as cervical intraepithelial neoplasia (CIN) grade III.
Complications and consequences
The consequences of CIN are directly related to the diagnosed stage of the disease. In general, most women take care of their health and regularly visit a doctor for preventive examinations. This significantly affects the risk of malignancy of dysplasia. According to statistics, 95% of the fair sex under the supervision of a gynecologist successfully cope with such an ailment as cervical dysplasia.
Diagnostics cervical dysplasia
Dysplasia is a characteristic transformation of the cellular tissue of the cervical epithelium. Accordingly, diagnostics are aimed at determining changes in the structure of endocervical cells.
Diagnosis of CIN (cervical dysplasia) is based on 7 signs that determine the morphology of the cellular structure:
- How much does the size of the cell nucleus increase?
- Changes in the shape of the nucleus.
- How the density of the nucleus' color increases.
- Kernel polymorphism.
- Characteristics of mitoses.
- Presence of atypical mitoses.
- Absence or determination of maturation.
Differential diagnosis
Cervical dysplasia requires careful examination and differential diagnosis is mandatory.
Differential diagnostics are necessary because the epithelial layer of the cervix has a layered structure. In addition, the cervix itself consists of a small layer of muscle tissue, it also contains connective tissue, blood and lymph vessels, and even nerve endings. Such a complex structure of the cervix requires clarification if the doctor doubts the diagnosis, especially in dysplastic processes.
Cervical dysplasia, what can it be confused with?
Differential diagnosis should exclude the following diseases:
- Cervical erosion during pregnancy, caused by a change in hormonal leadership and some shift in certain cellular layers. For the process of bearing a fetus, such changes are considered normal.
- Erosive processes, defects of epithelial tissue - true erosion. Trauma to the mucous membrane can be caused by anything - tampons, alkaline agents, drug therapy, intrauterine contraception, instrumental procedures without proper training and qualifications of the doctor. It happens that erosion occurs as an inevitable consequence of a planned surgical intervention. Lymphocytes, plasma cells, and other cellular elements may appear under a microscope, indicating the beginning of cell transformation. However, in combination with other examination criteria, all this can rather exclude dysplasia and confirm erosive damage.
- Cervicitis of infectious etiology. This is an inflammatory process in the epithelial covering of the cervix, which is quite common. The fact is that the epithelium is, in principle, very sensitive and susceptible to the influence of multiple factors. An infectious agent can provoke inflammation in the first two layers of tissue. Chlamydia, as a rule, affects cylindrical cells, gonococci as well. Other infections can give rise to a pseudotumor process or ulceration. Differential diagnostics should clarify and separate nosologies, preferably determining the type of pathogen of infectious inflammation.
- Diseases (STDs) transmitted through unprotected sexual intercourse. Trichomoniasis gives a picture almost in all respects similar to cervical dysplasia.
- Venereal diseases (syphilis), Treponemapallidum gives a picture of epithelial damage similar to dysplastic changes.
- Herpetic infections. The disease requires specification of the type and kind of herpes.
- Hyperplasia (polyp-like growth).
- Cervical polyps – type and kind (fibrous, inflammatory, pseudosarcomatous, vascular and others).
- Leukoplakia.
- Residual fragments of the Wolffian duct.
- Cervical atrophy due to low estrogen levels.
- Squamous cell papilloma as a benign neoplasm.
- Hyperkeratosis.
- Endometriosis.
- Protozoal infections (amebiasis).
- Cervical dysplasia is in most cases caused by HPV (papillomavirus), but it also requires specification of the type and kind.
Differential examination is a classic set of procedures in gynecology:
- Collection of the patient's anamnesis and complaints.
- Examination, including with the help of medical mirrors.
- Cytology.
- Colposcopy as indicated.
- Collection of material for histology – biopsy.
- Additionally, transvaginal ultrasound, PCR analysis, general and detailed blood and urine tests are possible.
Who to contact?
Treatment cervical dysplasia
Treatment of cervical dysplasia begins after a woman has passed all stages of diagnostics. The factors that provoke dysplastic pathologies are diverse, so an accurate assessment of the pathogen - a virus, infection is not only important, but can sometimes save the patient's life. Cervical cancer in women remains on the list of the most common oncological diseases. To detect it in time, to stop it at an early stage - this is the main task of treating cervical dysplasia.
Treatment involves solving a very specific problem - eliminating the cause that caused pathological changes in epithelial cells. Most often, the transformation of cellular tissue is provoked by viruses, the first place among them is occupied by the human papilloma virus. In addition, age-related hormonal changes, chronic inflammatory diseases, coccal infections and many other causes do not so easily "give up" their positions. A woman who has been diagnosed with cervical dysplasia should be prepared for a fairly long period of treatment, which will really make her healthy.
Let's consider what methods are used in the treatment of endocervical dysplasia:
- Conservative (taking medications according to the course and regimen determined by the doctor).
- Surgical (local surgical intervention, full-fledged operation, depending on the stage of development of the pathology).
- Additional treatment methods (physiotherapy, herbal medicine).
- Alternative methods of treating cervical dysplasia, which are not confirmed either clinically or statistically. Therefore, they will be discussed below only as an overview description.
In general, the therapy can be described as follows:
- Elimination of the cause of the disease and mandatory removal of the dysplasia sector:
- Cauterization of the area (laser therapy).
- Cryodestruction.
- Electrocoagulation method.
- Long-term drug therapy (immunomodulators, vitamin therapy).
- Surgical treatment (conization) or removal of the damaged area using a radiosurgical knife.
Tactical and strategic planning of treatment of cervical dysplasia directly depends on the severity of the pathology.
- The first degree of severity is drug therapy that activates and supports the immune system. Dysplasia is often neutralized after treatment, this is especially true after the elimination of the pathogen - HPV.
Treatment plan:
- Continuous observation of the patient for one to two years after diagnosis has been clarified.
- Regular screening of the epithelial condition (cytology).
- Immunomodulators, intake of important microelements – selenium, folic acid, B vitamins, vitamins E, A, C.
- Parallel treatment of concomitant pathologies of the genitourinary system.
- Treatment of areas of the cervix damaged by dysplasia using chemical coagulating agents (vagotyl).
- Recommendations for healthy eating and lifestyle.
- Selection of adaptive contraceptive methods that exclude hormonal drugs.
- Observation by an endocrinologist.
- Second degree of severity:
- Methods of cauterization.
- Cryotherapy methods (cryodestruction).
- Laser treatment.
- Radio wave therapy treatment.
- Conization (excision of the affected area of epithelial tissue).
Surgical treatment for cervical dysplasia is performed on the second day after the end of the menstrual cycle in order to prevent pathological proliferation of the endometrium. Also, small wounds after surgery heal more easily on these days.
- The third degree of severity is a serious diagnosis. Treatment is determined jointly with an oncologist.
A brief overview of treatment methods with their advantages and some disadvantages:
- Cauterization.
- The advantage is availability, both in terms of technology and cost.
- The disadvantage is that there is no technological possibility to control the quality of cauterization and the depth of penetration of the electric loop.
- Cryomethod (destruction using ultra-low temperatures):
- There is no deep scarring after the procedure; the method is suitable for young, nulliparous women.
- The disadvantage is complications, temporary but uncomfortable, in the form of heavy discharge after the procedure. It should also be taken into account that after cryofreezing the patient must abstain from sexual intercourse for 1.5-2 months.
- Laser treatment:
- The specific “evaporation” of the affected area of the epithelium leaves virtually no traces, no scars, the procedure is very precise.
- Nearby areas of the cervix may be affected by the laser and may be burned.
- Radio wave therapy:
- The method is considered to be low-traumatic, precise, and painless. No rehabilitation or regime restrictions are needed after radio wave treatment. Relapses are virtually non-existent.
- The disadvantage can be considered the high commercial cost of the procedure.
- Conization:
- No specific criterion of conical excision of tissue can be considered an advantage or disadvantage. In all cases of using a scalpel, wounds will remain, the method is traumatic, but in modern practice, gynecologists perform conization with a laser. Laser excision is much more effective, does not cause prolonged bleeding. Conization as a treatment for cervical dysplasia is prescribed only if necessary and it is impossible to use a more gentle method.
In general, treatment of cervical dysplasia is divided into several stages:
- General – drugs for normalizing the state of epithelial tissue (orthomolecular therapy) – essential vitamins (beta-carotene, B vitamins, ascorbic acid, folic acid, oligomeric proatocyanidins, PUFA – polyunsaturated fatty acids, selenium, enzyme therapy. This category also includes a special diet.
- Drug treatment - immunomodulators and cytokines to neutralize viruses and infectious agents.
- Local therapy – chemical cauterization (coagulation).
- Treatment with surgery.
- Phytotherapy
Medicines
Cervical dysplasia is successfully treated in most cases, provided that diagnostic measures are carried out in time. Medicines can be prescribed as an auxiliary stage of therapy; the basic treatment of CIN is considered to be methods of removing epithelial tissue, the area and layer where the pathological process develops. However, conservative treatment with medications is also included in the complex of therapeutic measures. First of all, medications are needed to neutralize the activity of the most common causative agent of dysplastic changes - HPV. In addition, an important criterion for choosing drugs can be the woman's age and her desire to maintain fertility.
Medicines used in the treatment of CIN are aimed at achieving the following objectives:
- Anti-inflammatory medications (etiotropic therapy). The treatment regimen is selected depending on the etiology and stage of the disease.
- Medicines from the category of hormonal drugs for restoring normal functioning of the endocrine system.
- Immunomodulators.
- Medicines and agents that help normalize the vaginal microbiocenosis (microflora).
Thus, the medications that can be prescribed at the stage of conservative treatment are all types of immunomodulators, a carefully selected complex of vitamins and microelements. Gynecologists assign the leading role to folic acid, a group of vitamins - A, E, C, selenium.
More details about what medications can be prescribed for cervical dysplasia:
Drugs that stimulate the immune system |
Interferon-alpha 2 Isoprinosine Prodigiosan |
Activates the production of immune cells capable of resisting viral infections. Protect cells from penetration of bacteria and viruses Strengthens all protective functions of the body as a whole |
Vitamin preparations, microelements |
Folic acid Retinol (vitamin A) Vitamins C, E Selenium |
Folic acid is prescribed as a means of counteracting the destruction of epithelial tissue cells. Vitamin A helps epithelial cells to undergo the division process normally. Vitamin E acts as a powerful antioxidant. Vitamin C is considered a classic remedy for strengthening the body's defenses. Selenium also acts as an antioxidant and helps endocervical tissue cells regenerate and recover after conization, cauterization and other therapeutic procedures. |
Similar treatment regimens for cervical dysplasia are used in almost all countries that consider themselves developed. Gynecologists try to avoid serious surgical interventions for as long as possible when diagnosing CIN, however, medications are not always able to effectively affect the pathological process of cell degeneration. Therefore, in 65-70% of cases, it is necessary to remove a section of cervical tissue, and then prescribe a maintenance course of medication.
It should be noted that the doctor can also conduct antibacterial, antiviral therapy, as a rule, this happens when cervical dysplasia has already progressed to more severe stages. In general, medications as a separate treatment strategy for CIN are not used.
Surgical treatment of cervical dysplasia
Surgical treatment of cervical dysplasia is the most commonly used method. The choice of therapy for CIN depends on many factors - the patient's age, the stage of dysplasia, concomitant pathologies, the size of the damaged epithelium. A wait-and-see treatment strategy is appropriate only when cervical dysplasia is diagnosed as moderate, i.e. stage I severity.
Modern surgical treatment includes several basic techniques:
- Excision and its variants: loop electrocoagulation, radioexcision, diathermoelectric method of tissue removal, electroconization.
- Destruction of an atypical area of epithelium using cold exposure – cryoconization, cryodestruction.
- Laser vaporization (also laser conization or cauterization).
- Excision of the zone of atypical transformation of epithelial cells – knife conization.
- Removal of the cervix - amputation.
Under what conditions is it advisable to perform surgical treatment of cervical dysplasia?
- The best period for removing a pathologically altered area of epithelium is considered to be the follicular phase of the monthly cycle (phase I). At this time, after the procedure, tissue regeneration improves due to the increased content of estrogens.
- If the surgery is performed urgently, it is necessary to determine the level of human chorionic gonadotropin (hCG) to exclude possible pregnancy. This is especially important when the surgery is scheduled for the second phase of the menstrual cycle.
- Surgical intervention is inevitable when cervical dysplasia is diagnosed at stage III. In this way, the risk of malignancy – the development of oncopathology – can be minimized.
- In case of detection of HPV (papillomavirus), the most effective methods are laser removal of transformed cells or diathermocoagulation.
More about surgical treatment methods for CIN:
- Destruction. As a rule, gynecologists use a cold method - cryodestruction using a cryogen (liquid nitrogen). This technology was first tested in 1971 and since then its effectiveness has been confirmed clinically and statistically by almost all doctors in the world. The cryomethod is used on the 7th-10th day of the monthly cycle, does not require specific preparation. However, there are some contraindications to its use:
- infectious diseases in the acute stage.
- obvious areas of scar tissue in the cervix.
- acute inflammatory process in the vagina.
- cervical dysplasia progressing to stage III.
- chronic endometriosis.
- tumor process in the ovaries.
- unclear boundaries of the pathologically altered area of the cervix.
- pregnancy.
- start of menstruation.
After cryodestruction, many patients note bloody, rather abundant discharge, which is considered an acceptable norm for a certain postoperative period. The effectiveness of the technique is close to 95%, depending on the preliminary diagnostics and individual characteristics of the patient. Relapse is possible in cases of incorrectly determined stage of cervical dysplasia.
- Diathermocoagulation is one of the most common methods of surgical treatment of cervical dysplasia. In essence, this is a method of cauterization using two types of electrodes - large and small (in the form of a loop). The current is supplied pointwise and at low voltage, which allows for a fairly targeted procedure. The nuance of the technique is that there is no way to regulate the depth of cauterization, but with comprehensive detailed diagnostics, this task can be overcome. Complications - scars, tissue necrosis, possible development of endometriosis. According to statistics, about 12% of patients may fall into the category of those who suffer from such consequences.
- Laser vaporization and laser conization. Vaporization has been known to gynecologists since the 80s of the last century, the method was very popular, but still remains quite expensive. Radiation, CO 2 method is a targeted destruction of atypical cells. The technology is effective, almost bloodless, but, like other surgical methods, it has its side effects:
- Burning of nearby tissue areas is possible.
- the inability to perform histology after surgery.
- the need for complete immobilization of the patient (immobility with the help of general anesthesia).
- risk of pain after the procedure.
- Gynecologists use the radio wave method as an alternative to other methods. The technology has not yet received official approval from the world medical community, since there is not enough clinical and statistical data. Just like ultrasound treatment, RVT (radio wave therapy) has been little studied in terms of complications and effectiveness.
- Conization of the cervix with a scalpel (knife conization). Despite the emergence of more modern techniques, conization with a scalpel remains one of the most common methods of treating CIN. Gynecologists excise a section of atypical cells using the cold knife method, while simultaneously taking tissue for biopsy. Complications and disadvantages of the technology - possible bleeding, risk of trauma to surrounding tissues, long-term regeneration.
- Removal of the cervix or its part (amputation) is carried out strictly according to indications, when cervical dysplasia is diagnosed as pronounced (stage III). The operation is performed in a hospital setting, general anesthesia is indicated. Such a radical method is necessary to minimize the risk of developing cervical cancer.
Sex with cervical dysplasia
Cervical dysplasia is not a contraindication for intimate relationships. Sex with cervical dysplasia is possible, but there are certain conditions and rules.
Abstinence is indicated after surgery (surgical treatment of cervical dysplasia):
- Laser cauterization (or radio wave method).
- All types of conization (cryodestruction, using a laser or electrical loop).
- Removal of part or all of the cervix (amputation).
Why should you limit sexual contact?
- 1-2 months after cauterization, the epithelial tissue is restored, regeneration takes time. During this period, the woman needs special conditions - a special diet, daily routine, and the use of vaginal tampons is also prohibited. The period of abstinence is determined by the method, the patient's condition and the stage of cervical dysplasia.
- Excision of a section of the cervix is a rather serious procedure. After it, it is necessary to exclude intimate relations for at least 4-5 weeks. Conization is considered a more serious surgical intervention compared to vaporization or cauterization, so abstinence from sex can last up to two months.
- Removal (amputation) of the cervix requires at least 2 months of abstinence from sexual intercourse. The period of abstinence is determined individually, but one should remember about the serious health consequences in case of violation of the abstinence regime.
The reasons why sex is excluded after surgery are quite understandable:
- The wound surface is very vulnerable, including to infections. In addition, sexual intercourse significantly slows down the process of tissue regeneration.
- Intimate life during the time when bleeding is possible after surgery is questionable as such.
- Sexual contact after surgery can further traumatize the cervical epithelium and provoke a relapse of dysplasia.
- There is a risk of re-infection with infectious agents if the partner did not undergo treatment together with the woman.
- Sex in the postoperative period can cause damage to the healing area, which can lead to bleeding.
- For a woman, intimate relations after removal of the damaged area of the cervix are very painful and cause discomfort.
If cervical dysplasia is treated conservatively, sex with a partner is not prohibited, but you will have to consult with your gynecologist. It is not recommended to enter into relationships with unfamiliar partners, of course, frequent changes are excluded. Also, a woman needs to be extremely attentive to her own health, especially if atypical discharge or pain occurs after sexual intercourse. This may be the first sign of an accelerating pathological process.
Sunburn in cervical dysplasia
Tanning and gynecological disease are incompatible. Cervical dysplasia is considered a pre-oncological disease. Not being a death sentence, however, such a diagnosis suggests preventive and protective measures
One of the factors that provoke cancer, including cervical cancer, can be excessive sunbathing. Dysplasia in the initial stage can be successfully treated, but its development can be provoked by sun rays, solarium. This is due to the fact that viruses, bacteria, infectious agents, which are often the cause of CIN, respond well to heat, it is an almost ideal environment for them. In addition, many hours on the beach will not so much give the skin a beautiful shade, as it will reduce the protective functions of the body, not to mention sunstroke or heat stroke. Weakening of the immune system is a sure way to start the development of infections and related pathologies. UV rays are useful only at a certain time, in a normal dose and only for absolutely healthy people. Their excess has a negative effect on the cellular structure, and cervical dysplasia is just an atypical division of epithelial cells. In addition, ultraviolet radiation can penetrate deep enough into the layers of the skin and activate “dormant” oncological processes, causing genetic failure.
Sunbathing with cervical dysplasia can only take place if the attending physician has given permission for it and has specifically prescribed a sunbathing regimen. This rule also applies to visiting a solarium. Even with CIN at a mild, initial stage, you should not experiment and risk your own health. Remember that, according to statistics, cervical cancer ranks third among all the most common oncopathologies in women. The sun will wait, you can sunbathe when the disease is left behind. This time usually comes 12-16 months after successful treatment and regular examination by a doctor.
More information of the treatment
Prevention
Cervical dysplasia is a serious diagnosis, the condition of the epithelial tissue is threateningly tending to oncopathology. Therefore, prevention should be comprehensive and regular. Cervical cancer as one of the risks of developing CIN starts with precancerous gynecological diseases. One of the most effective methods of prevention in this area is considered to be systematic screening. Back in 2004, the international community of gynecologists approved a resolution on a total screening examination of all women, starting from the age of 20-25. Examinations are recommended to be carried out at least once every 2 years until reaching the climacteric period (50-55 years). Then preventive screening is prescribed every 3-5 years, although patients can undergo it more often at their own request.
The program for prevention of cervical dysplasia makes it possible to identify areas of pathologically altered epithelium at early stages and take timely measures to stop them. It is worth noting that screening is not a 100% way to prevent the development of HPV (papillomavirus), it can only be stopped by vaccination.
Vaccines are effective against all oncogenic infectious and viral agents, and are recommended for women of reproductive age. Such measures, together with regular cytology, significantly reduce the number of cases of cervical cancer and save thousands of lives in general.
Thus, prevention of cervical dysplasia, or rather, its transformation into stage III, consists of the following actions:
- Timely visit to the gynecologist, at least once a year.
- Comprehensive treatment of any infectious or viral pathogen.
- Healthy diet and lifestyle in general. Giving up harmful habits - smoking, alcohol abuse, promiscuous sexual relations.
- Observance of basic rules of personal hygiene.
- Use of cotton underwear, refusal of fashionable experiments with synthetic thongs and other “delights” that often lead to inflammatory processes.
- Contraception as a barrier to infections, especially STDs (sexually transmitted diseases).
- Vaccination against papillomavirus.
- Regular screening of the uterus, cervix and pelvic organs (PAP test, cytology, biopsy if indicated).
Recommendations for the prevention of the development of dysplastic pathologies for women of different age categories:
- The first preventive examination should take place no later than the age of 20-21 years (or in the first year after the debut of sexual relations).
- If the Pap test is negative, a preventive visit to the gynecologist should be made at least once every 2 years.
- If a woman over 30 years of age has normal Pap tests, she still needs to see a doctor at least once every 3 years.
- Ladies over 65-70 years old can stop visiting a gynecologist and examinations if cytology is normal. Preventive screening should be continued in case of frequent positive Pap tests up to 50-55 years old.
In many developed countries, there are educational programs for the population, which carry out explanatory work on the threat of cancer and its prevention. However, neither programs nor orders at the government level can replace common sense and the desire to preserve one's own health. Therefore, the prevention of cervical cancer and dysplastic changes should be a conscious and voluntary matter, every reasonable woman should understand the importance of preventive examinations and undergo them regularly to avoid serious consequences.
Forecast
Cervical dysplasia is not cancer yet, such a diagnosis only indicates the risk of malignancy of the pathological process. According to statistics, about 25-30% of patients who refused complex treatment and regular examinations end up in an oncoclinic. There are other figures, more optimistic. 70-75% (sometimes more) with the help of diagnostics, a carefully selected course of treatment, including radical methods, are completely cured and then undergo only preventive examinations. It is obvious that the overwhelming majority of women are still more attentive to their own health and successfully overcome the disease.
To make the information more convincing, we will formulate the prognosis for cervical dysplasia in the following way:
- Every third patient diagnosed with CIN did not experience symptoms of the disease. Dysplasia was detected by chance during a routine examination by a doctor.
- Modern medicine is able to successfully combat cervical cancer, provided that the pathology of the epithelial lining of the cervix is detected in a timely manner.
- Surgical treatment for the diagnosis of cervical dysplasia is indicated in 80-85% of cases.
- Relapses of dysplastic processes are possible in 10-15% of cases even after successful treatment. They are usually detected during preventive examinations 1.5-2 years after surgery.
- The recurrence of the development of pathology can be explained by inaccurate excision of the area with atypical cells or in the case of persistence of the papillomavirus.
- During pregnancy, stage I dysplasia can be neutralized through powerful restructuring of the woman’s hormonal, immune and other systems.
- Cervical dysplasia does not interfere with natural childbirth and is not a strict indication for cesarean section.
- With CIN in the moderate stage, the prognosis is more than favorable. Only 1% of patients continue treatment due to the transformation of the pathology into stages II and III.
- 10-15% of women with stage II cervical dysplasia continue complex therapy due to the development of the process to stage III (this occurs within 2-3 years).
- The transition of dysplasia to stage III and to cervical cancer is observed in 25-30% of women who have not received treatment, and in 10-12% of patients who have undergone a full course of therapeutic measures.
- More than 75-80% of women who are diagnosed with CIN early recover completely within 3-5 years.
Cervical dysplasia as an asymptomatic process, developing rather slowly, remains a difficult but surmountable task for gynecologists. This problem is solved especially successfully provided that the woman understands the seriousness of the disease and consciously undergoes timely preventive examinations, including the entire necessary set of diagnostic tests. CIN is not oncology, but still the first alarm signal about a threat. The risk is easier to prevent and neutralize at the very beginning of development.

