Medical expert of the article
New publications
Removal of acute condylomas
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
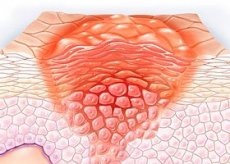
In modern dermatological, proctological and gynecological practice, removal of genital warts is considered the most effective method of getting rid of the visible manifestation of infection with the human papillomavirus of the squamous epithelium of the skin and mucous membranes of the anal and urogenital area.
 [ 1 ]
[ 1 ]
Indications for removal of genital warts
Typical localization of viral condylomatosis in women is the external genitalia, vagina, cervix, opening of the urethra, perineum, external and internal surfaces of the anus; in male patients, pointed genital warts occur on the foreskin and head of the penis, on the scrotum, near the opening of the urethra, in the urethra, around and inside the anus.
Indications for removal of genital warts include factors such as:
- progression of the pathology, in which the size of the condylomas or their number increases:
- the presence of large condylomas that do not respond to local drug treatment with ointments;
- constant trauma to the condylomas, even to the point of bleeding;
- physical discomfort and problems during sex, urination, defecation;
- the threat of complications during the upcoming birth (if localized in the cervix and in the cervical canal) and infection of the newborn;
- the emergence of psychological discomfort due to an external defect.
In addition, as studies of the last decade have shown, with oncogenic types of papillomavirus 16 and 18, condylomas on the cervix can lead to squamous cell cancer.
How are genital warts removed?
Removal of genital warts can be performed:
- surgically (excision),
- hardware ablation (diathermocoagulation, cryogenic destruction, laser coagulation, radio wave excision),
- by contact chemical method.
Classic surgical excision of acuminate condyloma is applicable for single, fairly hard formations (10 mm or more in diameter) that have formed on the penis, in the vagina or around the anus, for extensive formations, and also for relapses of condylomatosis after other treatment methods. Excision is performed under local anesthesia, stitches are applied to the wound at the site of the excised condyloma, and a scar is subsequently formed. Pain after surgery may persist for up to three weeks.
Removal of pointed condylomas with electric current - diathermocoagulation: this is burning of the formation with high temperature created by high-frequency current. The method is painful, so local anesthesia is needed. A scab forms at the site of the burned genital wart, which falls off on its own after 7-8 days. After the scab comes off, a large scar remains. Currently, electrocoagulation is considered an outdated method; according to foreign specialists, the probability of relapse after its use ranges from 30 to 70%.
Nitrogen removal
Cryotherapy or removal of genital warts with nitrogen is the destruction of warts by instantaneous (within 10-20 seconds) freezing of tissue with liquid nitrogen (temperature below -195°C). Necrosis and rejection of the wart occurs. This method is most often used to remove several small warts, especially those located on the penis, vagina, rectum and urethra. Although there is an opinion that this method should not be used in hard-to-reach places.
Local anesthesia is used if warts are present in several places or when the affected area is large.
During the procedure, patients feel a burning sensation, and after its completion - moderate pain. Blisters and hyperemia of the skin may appear, but there are practically no scars. Healing takes an average of two weeks. The probability of relapse of the pathology (after several months) is 20-40%.
Laser removal
Laser therapy (using carbon dioxide or infrared lasers) completely removes the viral neoplasm with an efficiency of up to 90%. But this method is very painful and is performed under local or general anesthesia - depending on the number and size of warts. As a rule, wounds heal for at least a month, scars remain at the site of removal.
Laser removal of genital warts is recommended for the treatment of large genital warts that cannot be treated using other physical ablation methods due to access difficulties. This applies to warts located deep inside the anus or urethra. With this method, the risk of warts recurring is 25-50%.
Radio wave removal
With this method, condylomas are removed using a special radio wave surgical generator Surgitron Dual, which operates without contact with tissues - radio waves. According to reviews from doctors and patients, this procedure is fast, minimally traumatizes the surface of the skin and mucous membranes and does not cause pain.
Radio wave excision - removal of pointed condylomas by radio wave method - refers to bloodless high-precision methods of hardware surgery, since the dissected tissues are simultaneously coagulated, preventing bleeding. After its implementation, there is no need to apply stitches and no scars are formed.
In general, experts consider physical ablation to be more effective for keratinized condylomas, while for soft condylomas in the genital area, contact chemical removal is more suitable.
Removal with Solcoderm
A chemical solution to the problem is the removal of pointed condylomas with Solcoderm. This solution (in 0.2 ml ampoules) is intended for external use only. It contains nitric, acetic and lactic acid, oxalic acid dihydrate and copper nitrate trihydrate.
The action of the concentrated acid compound leads to chemical denaturation of the proteins of the condyloma tissue, its drying out and falling off in the form of a scab. If the drug gets on healthy skin or mucous membrane, a burn and necrosis also occur. Therefore, according to the instructions, Solcoderm should be applied only in a medical institution, and the patient himself is not recommended to do this, although the ampoules are supplied with an applicator and a glass tube for the manipulation.
It should be borne in mind that removing pointed condylomas at home is very problematic in the absence of an overview of the genital formation, and is also very unsafe if there are several of them and they are on the mucous membranes. And doctors warn that attempts to get rid of condylomas on your own can lead to their quantitative growth.
If condylomatosis is multiple, Solcoderm is not applied to all lesions at once, but in stages: to 4-5 condylomas in one procedure, and after 24-25 days – to the next ones. In addition, after contact with water, it is necessary to treat the skin in the area where the preparation was applied with 70% medical alcohol. And in no case should you tear off the resulting scab: it should fall off on its own.
Preparations for chemical removal of genital warts also include Ferezol (phenol with tricresol) and Verrukacid (phenol with metacresol) solutions, which should be applied only to external warts - several times, after the solution already applied has dried.
Complications after removal of genital warts
The most common complications after removal of pointed condylomas are pain, swelling and redness of tissues, discharge (in case of internal localization of condylomas), bloody discharge (in case of damage to blood vessels), erosion, inflammation (in case of infection). In addition, all methods of removal have a significant level of relapse of the disease.
It should also be remembered that the removal of genital warts cannot cure the human papillomavirus, which continues to remain in the skin and mucous membranes in an inactive state, and a person can still spread the infection through contact and sexual intercourse.

