Medical expert of the article
New publications
HPV type 58 in women, men and children
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
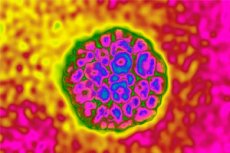
Today, there are more and more problems with which people turn to cosmetologists, dermatologists, but they are unable to help them. This is due to the fact that the cause is not cosmetic. It must be sought much deeper, in the features of anatomy, physiology, as well as in the composition of biological fluids. In many ways, the condition is determined by the bacterial and viral load, the state of immunity. Today, one of the common causes of skin neoplasms on the skin, mucous membranes, is HPV type 58. The abbreviation stands for human papillomavirus, related to type 58. But this virus causes not only neoplasms. Let's consider its features in more detail.
The most dangerous HPV?
The reason for the higher prevalence of HPV 58 in East Asia is still not fully understood. The establishment of a tumor cell clone from HPV-infected epithelium is a multi-step process involving multiple factors, in which host genetics is likely to be a major determinant. [ 1 ]
There are many HPV genotypes. The most dangerous of them are types 16, 18, and 33. The main danger is carcinogenicity, that is, the ability to cause cancer. As for type 58, it is also dangerous, since under certain circumstances it can cause malignant degeneration of cells, but it is much less common than other genotypes.
The danger is that the mucous membranes of the genitals and the reproductive system are affected, the infection can progress quickly, going beyond the mucous membranes. Damage to internal organs or the entire body can be observed - the chest, abdomen, and even the neck and face.
The third significant risk is that they can cause infertility in both men and women. They often lead to gynecological and urological diseases, in women they cause the inability to become pregnant, carry a child to term, lead to abortions, miscarriages, stillbirths, premature births. There is a risk of infection of the child during passage through the birth canal during childbirth.
They manifest themselves in a similar way. There may be a long incubation period, so they are often difficult to diagnose. From the moment of infection to the moment the first signs of the disease appear, more than one month may pass. During this period, a number of pathological changes occur in the body, many of which are irreversible. They are also all transmitted sexually.
In the cutaneous form, growths and papillomas may appear on the skin. They may be flat or raised. They are distinguished by the ability to grow and multiply quite quickly. They can be either single or multiple. With persistence or high virus content in the blood, symptoms similar to a cold are noted. Thus, a person's body temperature may rise. Runny nose, cough, tonsils, lymph nodes often appear, and tonsils, lymph nodes become inflamed.
Structure HPV type 58
Papillomaviruses have a small double-stranded DNA genome of approximately 8 kb. [ 2 ] To date, more than 120 HPV types have been well characterized, of which approximately 40 types can infect the genital tract. [ 3 ] About 15 types of these genital (mucosal) HPVs are classified as "high-risk" because of their oncogenic or possible oncogenic properties, either demonstrated by in vitro biochemical studies or inferred from epidemiological observations. [ 4 ] Two early proteins, E6 and E7, are the major oncoproteins encoded by high-risk HPVs. [ 5 ], [ 6 ] The E6 protein associates with the tumor suppressor protein p53 in association with the E6-associated protein (E6-AP). Overexpression of E6 results in p53 degradation, antiapoptosis, chromosome destabilization, increased integration of foreign DNA, and telomerase activation. E7 binds to retinoblastoma protein (Rb) and Rb-associated pocket proteins, resulting in inactivation of Rb-associated pocket proteins, activation of cyclins, inhibition of cyclin-dependent kinase inhibitors, and increased integration of foreign DNA and mutagenesis.
The HPV genome is packaged into a major capsid late protein L1 and a minor capsid protein L2. [ 7 ], [ 8 ] Five L1 proteins form a pentamer, and 72 pentamers make up the viral capsid. The L1 and L2 proteins self-assemble into virus-like particles (VLPs), which induce high levels of neutralizing antibodies and are highly protective. [ 9 ], [ 10 ] L1-VLPs are components used in the development of specific prophylactic vaccines. Targeting L1 vaccine prevents infection by only certain HPV subtypes due to the lack of cross-protective epitopes in different HPV subtypes. HPV L2 protein also induces neutralizing antibodies, the N-terminus of the L2 protein contains cross-protective epitopes and represents a target for neutralizing antibodies. Therefore, targeting L2 may be an attractive approach for a vaccine candidate.
High-risk HPV genotypes 58
HPV 58 is a virus cloned in 1990 that is phylogenetically related to HPV 16 and classified in the genus Alfapapillomavirus, species groups α-9, consisting almost entirely of carcinogenic types having as their major type the species HPV 16, also encompassing several other species that are related to HR-HPV 16, including HPV 58. [ 11 ] HPV58 is strongly associated with CIN of varying degrees and has been isolated from specimens of condylomata, premalignant lesions, and invasive cancer. [ 12 ]
Recently, two independent studies have come to the same conclusion and have provided a basis for future research. [ 13 ], [ 14 ] The results of the studies are to classify HPV 58 variants into four lineages designated as A (sub-lineages A1 and A2), B (sub-lineages B1 and B2), C and D (sub-lineages D1 and D2). Based on 401 isolates collected from 15 countries/cities across four continents, lineage A was found to be the most common in all regions. Lineage C was found to be more common in Africa than anywhere else, while lineage D was more common in Africa than in Asia. It is noteworthy that sub-lineage A1, representing the prototype obtained from a Japanese cancer patient, was rare worldwide except in Asia. Whether the higher contribution of HPV58 to invasive cancer in East Asia is due to the higher oncogenicity of the A1 sub-lineage is worth further investigation. The study also identified sequence signatures representing these lineages, allowing large-scale molecular epidemiological studies on HPV58.
Life cycle HPV type 58
There are five phases in the HPV life cycle, which include
- infection,
- proliferation,
- genomic phase,
- viral synthesis and
- selection. [ 15 ]
In the first stage of infection, the basal cells are infected with HPV. The second stage is genome maintenance. During this stage, the early viral proteins (E1 and E2) are expressed. The virus maintains its genomic material with a low copy number (10–200 copies per cell). This is followed by the proliferative phase and the early proteins E6 and E7 are expressed. These proteins stimulate cell cycle progression and regulate regulation in the parabasal layer. Genomic amplification follows in the suprabasal layer and the early proteins (E1, E2, E4, and E5) are expressed. Viral synthesis then occurs and the late proteins (L1 and L2) are expressed. In the epithelial layer, these structural proteins enhance viral packaging. In the stratified epithelium, the virus is released as dead cells die and the virus is free to infect other cells. This infectious cell cycle is thought to occur over a period of two to three weeks. The incubation period can vary from 1 to 20 months.[ 16 ]
Another possibility in the HPV life cycle is latency. After the initial infection, the immune system can cause a regression of the viral life cycle, and the virus can remain in a latent stage in the basal epithelium.
How is HPV type 58 transmitted?
Papilloma viruses are highly contagious, they are easily transmitted from person to person. The threat of infection with them exists almost everywhere, but not everyone is susceptible to them. Even if a person is a carrier of this virus, this does not mean that the disease will manifest itself immediately. It can manifest itself many years after infection, it can manifest itself after the body has weakened, for example, after a serious illness, after surgeries, against the background of decreased immunity and hormonal imbalances, dysbacteriosis. Sometimes the disease can make itself known after antibiotic therapy, chemotherapy, during pregnancy, menopause, or in adolescence against the background of increased stress on the body and hormonal changes. Therefore, each of us should know how HPV type 58 is transmitted in order to be able to protect ourselves from infection.
The main route of penetration of the virus into the body is sexual intercourse, that is, the infection enters directly during sexual intercourse, if it is unprotected. [ 17 ], Any microtraumas and damages affecting the skin or mucous membranes are the gateway for infection, the probability of its penetration into the body increases sharply. Even if these are very microscopic injuries that cannot be seen with the naked eye, they are enough for the infection to freely penetrate into the body. In the absence of sexual contact, infection can also occur (if there was contact of damaged tissues with blood or any other infected surface). [ 18 ], [ 19 ]
Blood transfusions and transplants can also be the cause. Doctors and medical staff who come into contact with infected biological material often become infected.
There is also a high probability of infection of the child during childbirth, when passing through the birth canal of the mother, if she is infected with the virus. And this must be taken into account if a woman is planning a child. In most cases, if a woman is diagnosed with HPV type 58, this is the basis for a cesarean section, which will prevent infection of the child.
In case of physical contact or contact with the belongings of an infected patient, the risk exists only if there is damage to the skin and mucous membranes, including microscopic ones. This has been demonstrated in school-age children who acquire HPV from sharing school supplies. [ 20 ]
When the virus enters the body, it is initially inactive, and only then, after some time, it is activated (that is, there is initially an incubation period). During this period, the symptoms of the disease do not appear, but the person is already a carrier of the virus, and can infect other people at this time. The disease develops when unfavorable conditions of the external and internal environment occur. Most often, this is a decrease in immunity and hormonal imbalance. Also, after taking certain medications, after serious illnesses, the virus may be activated.
Therefore, if you are a carrier of a viral infection, its activation may occur under the influence of a number of factors, including after recently suffered viral, colds, after exacerbation of gastritis, hepatitis, other chronic pathologies of internal organs. Bad habits, polluted environment, concomitant venereal and other diseases, sudden change in climatic conditions, poor nutrition, lack of vitamins or minerals.
There is a genetic predisposition to decreased immunity, hormonal imbalances, and metabolic disorders. In this regard, the risk group primarily includes young people who do not have a regular sexual partner and do not use protection. This includes people who lead an immoral lifestyle with frequent changes of sexual partners, with promiscuous and non-traditional sexual relationships, take drugs, and abuse alcohol. Smoking can also be considered a risk factor, since it causes intoxication of the body and contributes to immune system tension.
Epidemiology
Human papillomavirus (HPV) is the most common sexually transmitted infection in the United States. The prevalence of human papillomavirus (HPV) among adults aged 18–69 years is 7.3%; high-risk HPV is 4.0%. [ 21 ]
HPV-58, which is associated with a high risk of cervical dysplasia and cervical cancer, is rare worldwide, usually in East Asia.[ 22 ] Overall, HPV-58 is the third most common oncogenic type in Asia, but causes only 3.3% of all global cervical cancer cases.[ 23 ],[ 24 ] In Korea, HPV-58 is the second most common type diagnosed in women with abnormal cytology specimens (10.8% of all abnormal cytology specimens).
Symptoms
The main symptom is the development of condylomas or papillomas on the body, which are pointed or flat growths on the external genitalia, on the skin, in the oral cavity, and in the anal area.
In most cases, condylomas are papillary growths that rise above the surface of the body, are pink, and sometimes flesh-colored. They usually consist of a large number of papules. Some of them are scattered over the body, others are grouped into separate groups. Sometimes these groups of papules grow together, forming a separate ridge.
Papillomas are often flat growths on the surface of the skin or mucous membranes. They may not always be noticeable on the body, but are discovered when they reach a fairly large size. They also often blend in with the skin in color and do not rise above it. They are discovered in most cases completely by accident, during a preventive examination or during the diagnosis of other diseases. As a rule, they do not cause significant discomfort to a person. The manifestations do not affect either the mental or physical condition of the body. They do not cause pain, do not entail itching or irritation, so a person rarely pays attention to them and rarely consults a doctor for this reason. Flat papillomas are considered safer than hanging ones, since they are not noticeable, do not separate from the surface of the body, and therefore are less likely to be subject to mechanical damage and pressure.
HPV 58 in women
For women, HPV 58 is much more dangerous than for men. This is primarily due to the high risk of developing infection of the fetus, since the virus is almost always transmitted through the birth canal, with microdamage to the child. With a high degree of viral load and a sharply reduced immunity, milk can also become infected in the woman's body, as a result of which the infection can be transmitted to the child. It can also cause miscarriage, premature birth, miscarriage, spontaneous abortion. Often causes gynecological diseases and pathologies, leads to infertility.
Papillomas located around the internal genital organs, on the cervix, also pose a risk. Firstly, they can be damaged during sexual intercourse (on the labia, in the vagina). Numerous injuries lead to degeneration and mutation, as a result of which neoplasms can become malignant. There is also a high risk of infection, development of inflammatory and purulent-septic processes with further progression and development of infectious diseases of the internal organs, genitourinary tract.
When neoplasms are localized on the cervix, they can cause the inability to conceive a child, lead to serious and incurable infertility. In 80% of cases, it is condylomas and papillomas on the cervix that cause cancer. [ 25 ] In addition, during childbirth, they can be damaged, ruptured, cause bleeding, ruptures. They can also lead to uterine bleeding, miscarriages, spontaneous abortions and premature births.
No less dangerous are flat condylomas located on the internal organs of a woman. During a gynecological examination, they are quite difficult to diagnose, since they are very inconspicuous, often small in size, flesh-colored (merge with the mucous membranes). To detect them, laboratory tests are most often used, which can accurately indicate the presence or absence of infection, as well as indicate its quantitative indicators.
Often HPV type 58, even the one that occurs in a latent form, triggers cervical dysplasia, inflammatory and dysplastic processes in the endometrium. It often causes the development of cervical, epithelial neoplasia, carcinoma. It should also be taken into account that the virus is not detected in the blood immediately, but after some time (from 1 to 6 months). During this time, signs of the disease may not yet develop, however, the virus will already cause significant damage to the body. Pathologies can already develop at the cellular, tissue levels.
HPV 58 in men
Often, papillomas and condylomas spread to neighboring areas and organs. They can affect the entire perineum, groin area. There are even cases when warts grow upward and first affect the lower abdomen, then the stomach, chest. With deep spread, there are often cases in which genital warts spread to internal organs, damage to the urethra, digestive tract, reproductive organs is noted. And such warts, of course, cause both physical and psychological discomfort. With mechanical damage, irritation may be observed, pain appears. Psychological discomfort is associated primarily with appearance, lack of aesthetics and beauty. The higher the warts spread, and the more noticeable they are, the worse the psychological state of a person.
Do not think that this virus is not dangerous. The greatest danger of this virus is associated with the fact that it is carcinogenic, that is, it has the ability to cause malignant neoplasms. With a high content of HPV type 58 in the body of men, papillomas and condylomas can develop into a malignant neoplasm. Thus, they are considered a precancerous condition. It is important to understand that not every person who has HPV type 58 detected in the blood is diagnosed with cancer, since the development of cancer requires a combination of many factors, including internal, external factors, genetic predisposition, and reduced immunity. However, most patients suffering from various forms of cancer have a fairly high content of the papilloma virus in their blood.
HPV 58 in a newborn
The possibility of maternal transmission was proposed by Hayek in 1956. [ 26 ]
Possible mechanisms of vertical transmission are not well understood. HPV DNA has been isolated from the vas deferens, seminal fluid, and spermatozoa.[ 27 ] Prenatal transmission of HPV has also been proposed. This is supported by the presence of HPV foci in the infant at the time of birth.[ 28 ] HPV has been detected in amniotic fluid that was obtained by amniocentesis before rupture of membranes,[ 29 ] and from amniotic fluid in primary cesarean sections in which artificial rupture of membranes was performed immediately before delivery.[ 30 ] These examples suggest mechanisms of ascending infection rather than transplacental HPV infection, as HPV infection does not result in viremia.
Most neonatal HPV infections are vertically transmitted at birth. It is also possible that the newborn is indirectly exposed to HPV on contaminated surfaces in the birthing room. HPV DNA can also be transmitted postnatally by caregivers during bathing or swaddling.
In very young children (less than four years old), visible manifestations of HPV infection may include condyloma acuminatum.[ 31 ] Cervical and anal infections in young children result from sexual abuse. Oral lesions include verrucae vulgaris, papillomas, condylomata, and focal epithelial hyperplasia.[ 32 ] However, the majority of these lesions (75%) are due to HPV types 6 and 11. Childhood recurrent respiratory papillomatosis (JORRP) is a rare, more serious condition that can occur.[ 33 ] JORRP is estimated to occur in 4.3 per 100,000 live births and is caused by infection with HPV types 6 or 11; it is most common in first-born, vaginally delivered infants of women under 20 years of age.[ 34 ]
A newborn has all the factors predisposing to the development of HPV 58: decreased immunity, increased reactivity and sensitization, weakness, decreased endurance and resistance of the body, disruption of the biochemical cycle, normal structural and functional state of the body, as well as unformed microflora, sometimes - hormonal imbalance. Under such conditions, papillomas, condylomas, growths (dysplasia) develop. This is especially dangerous for children with low body weight, premature babies, with jaundice and functional disorders of the liver. There is always a potential risk of progression of these conditions and their transition to malignant tumors - sarcomas, cancers, leukemia. The infection is transmitted during childbirth from an infected mother.
Among researchers there are indications that the development of warts, papillomas and condylomas may indicate the presence of a parasitic infection in the body, and progresses with prolonged and systematic intoxication of the body with by-products of parasite metabolism. As a rule, it indicates parasitic intoxication.
Diagnostics
To diagnose HPV type 58, women need to see a gynecologist, men - a urologist. These doctors will conduct an examination, prescribe the appropriate tests, instrumental methods. Also, if necessary, additional consultations with other specialists can be prescribed. In order to identify an infection that is latent, it will be necessary to take a test for latent infections, a number of other tests. This will require a smear of urethral discharge (gynecological discharge). The doctor collects the biological material and then sends it to the laboratory, where further research is carried out.
HPV 58 test
In the laboratory, a double study is usually performed from this material (analysis for HPV 58): a standard microbiological study and a cytological study. The first study allows diagnosing a bacterial infection, determining dysbacteriosis, and the condition of the mucous membranes. Cytological research allows detecting altered and mutated cells, and allows predicting the likelihood of cancer development or diagnosing it at early stages of development.
Sometimes, material is taken directly from the condyloma or papilloma (biopsy). This need arises when a malignant neoplasm is suspected. The biopsy (piece of tissue) is sent to the laboratory for further histological examination. The nature of tissue growth determines whether it is a malignant or benign neoplasm.
The use of the Pap test for cervical cancer screening has significantly reduced the incidence of cervical cancer and its associated mortality in recent years. [ 35 ] However, the Pap test has low sensitivity (<70%) for the detection of high-grade squamous intraepithelial lesions (HSIL), which raises several concerns regarding the need for additional methods to improve detection. [ 36 ] Therefore, it is recommended to perform human papillomavirus (HPV) DNA testing in combination with the Pap test to improve the detection of precancerous cervical lesions. [ 37 ]
Monolayer cytology techniques: New methods for collecting and processing Pap smear specimens have recently been developed to help reduce false negatives. In these methods, the specimen is collected in a preservative solution rather than being spread directly onto a microscope slide by hand. Cellular structure is better preserved because the cells are immediately fixed. Additionally, a cervical brush is used to collect the specimen, which provides nearly twice as many epithelial cells as other collection devices.[ 38 ]
Histopathology: Patients with abnormal Pap smear results who do not have gross cervical lesions are typically evaluated by colposcopy and colposcopic biopsy. After application of 3% acetic acid solution, the cervix is examined using bright filtered light at 10-15x magnification.[ 39 ]
Detection of HPV DNA by type-specific PCR. Type-specific PCR assays are based on sequence variations present in the E6 and E7 genes of HPV subtypes. Fourteen type-specific PCR assays for high-risk HPV (HPV-16, -18, -31, -33, -35, -39, -45, -51, -52, -56, -58, -59, -66, and -68) target approximately 100 bp within the E7 ORF. [ 40 ]
Common PCR primer. Most PCR studies to date have used consensus primers to amplify a broad range of HPV types in a single PCR amplification. These primers target conserved regions of the HPV genome, such as the L1 capsid gene. Primers MY09 plus MY11 target a 450 bp fragment within the HPV L1 ORF.[ 41 ]
The Hybrid Capture Assay (Digene, Beltsville, MD) is the only kit currently approved by the FDA for the detection of HPV DNA in cervical specimens. The Hybrid Capture Assay has been used in many studies, and the second-generation version of the Hybrid Capture Assay is now widely used in clinical diagnostic laboratories. It is an antibody capture/solution hybridization/signal amplification assay that uses chemiluminescence detection to qualitatively detect the presence of HPV. In this assay, DNA in patient specimens is first denatured and mixed with a pool of RNA probe in a buffered solution in a test tube.[ 42 ]
HPV 58 positive
The most informative method that allows you to directly judge the presence or absence of HPV type 58 in the body is PCR. This is a method that determines the genotype of the virus in the blood, or detects its fragments. It is also possible to determine the quantitative indicators of this virus in the body. In the latent form of the pathology, PCR is often the only method that allows you to diagnose the infection in the body.
Even if the DNA of the virus is very small in the blood, with the help of special viruses, it doubles and even triples in the sample being tested, as a result of which it becomes visible and can be visualized during examination. If you have received a test positive for HPV type 58, this means that the virus persists in the blood, or an active viral infection is occurring. In the absence of the virus in the blood, the test will be negative. For further treatment, it is necessary to determine the quantitative indicators of the virus in the blood.
If we talk about quantitative indicators, the norm is considered to be a complete absence of viruses in the blood. But this is an ideal case, and it is extremely rare at present. Therefore, there are certain conditional norms of HPV 33 in the body, they differ in different countries. Basically, it depends on climatic conditions.
Treatment
Most HPV-induced changes in cervical cells are transient, and 90% spontaneously regress within 12–36 months as the immune system clears the virus.[ 43 ],[ 44 ]
Treatment is directed at macroscopic (eg, genital warts) or pathological precancerous lesions caused by HPV. Subclinical genital HPV infection usually resolves spontaneously; therefore, specific antiviral therapy is not recommended to eradicate HPV infection. Precancerous lesions are detected during cervical cancer screening. HPV-associated precancerous lesions should be treated based on existing guidelines.
The treatment proceeds in two directions. On the one hand, this is actually antiviral therapy, aimed at eliminating the virus, reducing its activity and numbers.
For the treatment of HPV type 58, various antiviral drugs are used: anaferon, arbidol, groprinosin, isoprinosine. For the treatment of genital forms, both in women and men, suppositories are used, for example, kipferon, genferon, viferon. Panavir gel and oxolinic ointment are also used.
In addition to surgical and cytodestructive procedures, several antiviral and immunomodulatory agents may be prescribed.
Cidofovir is an acyclic nucleoside phosphonate derivative that has a broad spectrum of activity against DNA viruses and is used to treat CMV infections.[ 45 ] In vitro antiproliferative activity has been shown to be selective for rapidly proliferating HPV-infected cells. 1% cidofovir gel was used topically without adverse effects every other day for 1 month to treat 15 women with severe CIN.[ 46 ] Complete or partial responses were observed in 80% of patients, as assessed by histology and HPV DNA detection by PCR.
Podophyllin, a cytotoxic agent that arrests mitosis at metaphase (also used to treat genital warts), in combination with vidarabine, a DNA polymerase inhibitor, inhibited HPV gene expression and cell growth in cervical cancer cell lines.[ 47 ] Expression of HPV-16 E6 and E7 gene products in normal cervical keratinocytes in vitro in the presence of podophyllin or vidarabine sensitized these cells to apoptosis. Combination topical therapy with podophyllin and vidarabine ointments in 28 patients with mild to moderate CIN resulted in lesion regression and successful eradication of HPV-16 or HPV-18 DNA in 81% of patients.
IFN and intravaginal 5-fluorouracil have shown variable responses in clinical and in vitro studies. IFN-α is approved for the treatment of genital warts. The effects of IFN-α, IFN-β, and IFN-γ have been studied in several human carcinoma cell lines harboring HPV-16 or HPV-18. A response was seen in some cell lines but not others. In HPV-18 HeLa cells, all IFNs suppressed HPV E6 and E7 gene transcript levels. In HPV-18 C-411 cells, IFNs had no effect. In HPV-16 CaSki and HPK1A cells, only IFN-γ was effective. It is likely that, because IFN-responsive elements appear to be suppressed by at least some oncogenic HPV types, the usefulness of IFN therapy in cervical disease will be limited. [ 48 ]
On the other hand, this is a therapy aimed at preventing malignant neoplasms. To reduce the carcinogenicity of the virus, it is necessary to increase immunity. With a high level of immunity, the body itself will fight the infection and will not allow malignant degeneration of tissues. If necessary, immunomodulators and immunostimulants are used. It is necessary to remember that excessive stimulation of the immune system can also be dangerous due to the fact that autoimmune aggression can develop, in which the body attacks its own tissues and cells, destroying them.
Answering the question of whether it is possible to cure HPV type 58, it is worth noting that most often drug treatment is effective only in the early stages of the pathology. It is important to understand that it is impossible to achieve complete disappearance of all DNA fragments from the body. Once ill, DNA remains in a person's blood forever. But if a person has undergone treatment, DNA in this case no longer provokes the disease, and even more so, does not become a factor predisposing to the development of cancer. Also, treatment will not allow new condylomas or papillomas to develop.
Often there is a need to remove these neoplasms. Today, laser removal methods are widely used. Warts are evaporated and burned with a laser. This is considered the safest method, which does not cause complications. Risks and the likelihood of side effects are also significantly reduced. The recovery period is sharply reduced. The advantage of this procedure is that it can be used even to treat infections of internal organs, to remove condillomas and papillomas on the genitals.
Of course, to perform such an operation, you need to contact a surgeon or specialized dermatological clinics, where the operation will be performed. In no case should you remove it yourself, because if you do something wrong, a malignant degeneration of the wart may occur, which will lead to the development of cancer.
Typically, noninvasive intraepithelial lesions identified only by microscopy are treated with superficial ablative procedures such as cryotherapy or laser therapy. These are outpatient office procedures and fertility is preserved. Cryotherapy freezes the abnormal tissue and the surrounding 5 mm using a supercooled probe. Tissue ablation with a carbon dioxide laser beam is as effective as cryotherapy but is more expensive. Loop electrosurgical procedures are currently considered the preferred treatment for noninvasive squamous cell lesions. In these procedures, an electrically charged wire is used to ablate the transformation zone and the distal endocervical canal. It is less expensive than laser therapy and preserves the excised tissue for histologic examination of marginal status. After treatment of noninvasive intraepithelial neoplasia lesions with any method, the recurrence rate is as high as 31% with a median time to recurrence of 11.9 months.[ 49 ]
What to do if HPV type 58 is detected?
Treatment is mainly medicinal. Tablets, suppositories, various ointments, gels, creams are prescribed. Vitamin and mineral complexes are also useful. Most often, antiviral and immunostimulating drugs are used. Sometimes there is a need for surgical operations, for example, if the condylomas rise significantly above the surface of the body, if they have been damaged, or there is a risk of their compression, mechanical damage. If there is a risk of developing a cancerous tumor or malignant degeneration of a condyloma, papilloma, surgery may also be required.
In the postoperative period, antibiotics, anti-inflammatory drugs, ointments, and creams are used. In addition to treatment, you need to reconsider your lifestyle and include health-improving activities in your daily routine. You can try folk recipes, herbal remedies, and homeopathic remedies. Otherwise, if you do not know what to do if you have HPV type 58, you need to see a doctor and strictly follow his recommendations.
Prevention HPV type 58
Prevention is based on maintaining normal immunity, proper nutrition, and observing hygiene rules. It is important to lead a moral lifestyle: having a permanent partner, using protection when in contact with temporary partners, abstaining from non-traditional relationships, multiple partners, and preventive treatment if the sexual partner has an infection. You should periodically consult an immunologist, gynecologist (urologist), and get tested for viruses and latent infections. You should periodically take courses of vitamins and, if necessary, immunostimulants. It is important to monitor the body for parasitic infections, since they can also trigger the development of a viral infection and its activation. You should periodically take antiparasitic drugs.
The most important preventive measure is to get treatment in a timely manner when a viral infection is detected. Maintaining a high level of immunity is especially important, since the development of the disease is possible only with reduced immunity and disturbed microflora.
The efficacy of these vaccines is largely type-dependent, although some cross-type protection has been observed, particularly with the bivalent vaccine (Cervarix ®, GlaxoSmithKline Biologicals). [ 50 ] Therefore, differences in the distribution of non-vaccine types (non-HPV16/18) may impact the development of next-generation vaccines. Prevention of >90% of HPV infections requires targeting at least 5 additional high-risk HPV subtypes HPV-31, HPV-33, HPV-45, HPV-52, and HPV-58. [ 51 ]
Based on the results, HPV vaccination protects more than 70% of patients from high-grade lesions and cancer. However, the relatively high prevalence of HPV 58 found in studies conducted in different regions of Brazil, [ 52 ], [ 53 ] as well as in other countries [ 54 ] highlights the importance of future vaccines to include other HPV genotypes, in particular HPV 58, to increase the potential for preventing cervical cancer and other HPV-related diseases closer to 100%. [ 55 ]
Forecast
Often, it is HPV type 58 that causes genital warts. Their localization is mainly in areas such as the labia, vulva, vaginal walls, uterus. The cervix, oral cavity, anus and areas around it. With a high viral load and a sharp decrease in immunity, warts can also form in the pubic and perineal areas.
According to statistics, approximately 70% of the world's population is infected with the papilloma virus. Therefore, HPV type 58 is one of the most common viruses. About 60% of carriers of this virus remain carriers, and only 40% suffer from various forms of this infection. In approximately 8-10% of people, condylomas and papillomas develop into cancerous neoplasms. If the virus is detected in a timely manner, it can be prevented from being activated and kept in an inactive form, in which it will simply persist in the body, but will not cause disease. With an active form of the virus, by choosing the right treatment, it can be transferred to a state of persistence. The main thing is not to self-medicate, otherwise the prognosis may be unpredictable.

