Medical expert of the article
New publications
HPV type 18: structure, pathogenesis, prognosis
Last reviewed: 03.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The appearance of warts and papillomas on the body is associated with the penetration of the papillomatous virus into the body. However, not everyone knows that relatively harmless neoplasms on the skin are not the only manifestation of this far from safe virus. After all, what is united under the name of the human papillomavirus (HPV) is a large variety of infection types that cause various diseases, including cancer, with their characteristic symptoms. HPV types 18 and 16 are considered especially dangerous. And we can only wish our readers never to get to know them closely.
Structure HPV type 18
When scientists, after a long search for the truth, finally managed to identify such a life form as viruses, they were not surprised that these microparticles remained unnoticed for so long. Their small size (up to 500 nm) allowed them to pass through various filters. And even seeding in a favorable environment did not give results, since it was discovered that viruses cannot reproduce outside a living cell.
Viruses are a non-cellular form of living matter. Although it is very difficult to judge how much this matter is alive. Having microscopic dimensions and the ability to penetrate a living cell, viruses are active only inside the human body or other living organisms, including bacteria (bacteria have their own viruses that cause diseases and death of microorganisms, they are called bacteriophages and are used for medicinal purposes). In the environment around us, viruses are inactive and do not show signs of life.
The papillomavirus mainly affects mammals, which are more suitable than other living creatures for the introduction and life of viral particles called virions. The skin and especially the delicate mucous membrane of a person turned out to be easily permeable for HPV virions, which is why there is a high percentage of virus carriers among people. Moreover, these are people of different ages, because even a newborn baby can get a papillomavirus infection during movement through the mother's genital tract, if there were pointed condylomas on the mucous membrane of her uterus or vagina.
HPV 18 is one of 18 types of papillomavirus with a high risk of developing cancer. Its virions are round in shape and very tiny in size (no more than 30 nanometers). In their size, they are close to large protein molecules.
Usually living cells, including bacterial ones, have 2 types of nucleic acids (DNA and RNA) in their structure, which carry genetic information about hereditary properties. Viruses contain only one type of NC. Papillomavirus belongs to the class of DNA-containing viruses.
The HPV genome is represented as a ring DNA molecule consisting of 2 chains, surrounded by a protein shell (capsid). This is the simplest particle, which does not have its own energy exchange and is not capable of protein synthesis. The only thing it can do is penetrate the body of a living being by accidentally getting on the skin and attach itself to the host cell, feeding on its energy and gradually destroying it.
The human papillomavirus genome encodes two types of proteins:
- early (they are characterized by regulatory and reproductive functions; in HPV 18, these same proteins have a carcinogenic effect and provoke malignant degeneration of host cells),
- late (these are the proteins that form the virion membrane).
The human body is a complex structure that provides protection against various pathological processes. Thus, the growth and reproduction of cells are controlled by certain genes. Early proteins E6 and E7 of the HPV 18 virion destroy genes that prevent the development of the tumor process in a living organism.
Virions do not penetrate deep. They parasitize in the inner layers of the skin and mucous membrane, affecting young and mature keratinocytes of the epidermis. Until the viral particle penetrates the cell, it is not able to reproduce, its behavior is identical to that observed while the virion is outside the living organism. But, penetrating into a living cell, which becomes a source of nutrition and energy for the virion, it discards its protein shell and integrates into the cell genome, changing its properties. That is, the information encoded in the virion NC becomes the cell's own genetic information. And this information in highly oncogenic HPV types has a destructive nature, stimulating constant cell division, which the immune system is no longer able to control.
In a cell infected with a virus, new DNA and capsids are synthesized and combined into new fully formed virions with the same properties. The new virions capture other cells, changing their genetic information like their ancestors.
Life cycle HPV type 18
The life cycle of the papillomavirus is tied to the stages of development of the main cells of the epidermis - keratinocytes. It is easiest for the virion to penetrate into a young cell during its active division. Such cells are located near the basement membrane, located below the epidermis (under its upper layers). But as they mature, young keratinocytes infected with the virus rise higher, where new virions are formed.
The incubation period of HPV 18, which causes anogenital warts, can last from 1 to 4 months or more. This means that a person infected with the virus will not suspect that they are carrying the virus for several weeks or months before the first symptoms of the disease appear. But even the appearance of warts will not indicate cancer. It will take several more years for a benign tumor caused by the virus to transform into a malignant one.
It is very difficult to predict how soon this will happen, because everything depends on the human immune system and its ability to suppress cell growth. In some patients, malignancy of cells can be detected as early as 5 years after infection, while others will need 25-30 years, and in others, the body will be able to cope with the virus and remove it during this time, as happens with low-oncogenic viruses (usually, within a year, almost all such virions die naturally).
Pathogenesis
Today, more than a hundred types of papillomavirus infection are known. About 80 of them cause various diseases in humans. But not all of them are equally dangerous, so in virology there is a division of HPV types into high- and low-oncogenic. Before HPV type 16, everything was more or less peaceful, because from types 1 to 15, the viruses only caused warts on the body. True, types 6, 11 and 13 are also responsible for the appearance of genital warts on the mucous membrane of the internal genital organs in women, but they do not pose a particular danger.
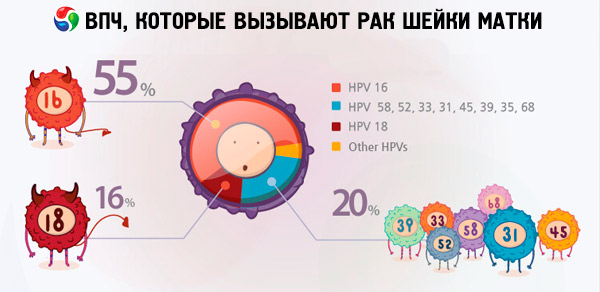
But starting with HPV type 16, problematic viruses with a high risk of developing oncological pathologies begin. All subsequent viruses pose a threat of oncology. In addition to type 16, 18, 31, 33, 39, 45 and some others are considered highly oncogenic (18 types in total).
As we can see, this list also includes the type 18 human papillomavirus that interests us. Moreover, it is the high-oncogenic risk HPV 18, along with HPV 16, that most often appears in gynecological charts as a causative agent of cervical cancer.
HPV 18 and Cancer
There are about 40 types of papillomavirus infection that affect the urogenital organs, causing the appearance of pointed and flat condylomas on the mucous membrane. But depending on the type of pathogen, such neoplasms may be a simple cosmetic defect or a cancerous tumor.
Pointed condylomas are convex growths on the skin in the form of papillae, which can be almost indistinguishable in color from the skin or be somewhat brighter than it. When affected by the virus, both single condylomas and multiple ones consisting of several closely located growths can be seen on the mucous membranes. Such neoplasms can be found in the anal area and perineum, as well as on the mucous membrane of the internal genital organs in women.
These growths are highly contagious. With such "papillae" the risk of transmitting the virus approaches one hundred percent. How is HPV transmitted? The human papilloma virus is considered one of the most common urogenital infections. Infection usually occurs during sexual intercourse, but contact transmission is also possible when touching the affected area.
The presence of pointed condylomas does not mean that a person can get cancer. These are neoplasms of medium oncogenicity, which do not often lead to oncology. But the appearance of flat condylomas, which are located flush with the surrounding surface of the mucous membrane, already represents a real risk of a deadly disease.
Flat condylomas are a rarer phenomenon, which are mainly found in women in the vagina and cervix. Doctors blame the appearance of such neoplasms on highly oncogenic types of the virus, including HPV 18.
The appearance of condylomas on the genitals of women and men does not yet indicate cancer. And even a predisposition to oncology is revealed in the laboratory, when the type of virus is determined. For example, the detection of HPV type 6, 43 or 11 will not cause the doctor any particular concerns about the patient's health, although he will suggest removing the growths on the mucous membrane just in case. Another matter if the analysis shows the presence of HPV type 18.
What is so dangerous about HPV 18? We have already said that this type of human papillomavirus is classified as highly oncogenic. Moreover, it is a fairly common infection that can hide in the body for a long time, destroying healthy cells, changing their genetic information and pushing them to uncontrolled reproduction.
According to various data, from 70 to 90% of the planet's inhabitants are carriers of various types of papillomavirus infection. Among women diagnosed with uterine cancer, 2/3 were carriers of viruses of types 18 and 16, which indicates that these types of HPV are the most dangerous.
It is HPV types 18 and 16 that often cause the development of cancerous tumors against the background of diseases that do not cause such complications in people without the virus. For example, erosion or dysplasia of the cervix can unexpectedly develop into cervical cancer precisely due to HPV types 16 and 18. Women who have not been diagnosed with highly oncogenic types of papillomavirus can live with these pathologies for many years without any particular risk to life.
But what kind of parasites are these that not only live at the expense of humans, but also gradually kill them? Let's try to look at the papilloma virus from a biological point of view.
 [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ]
[ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ]
Complications and consequences
The human papilloma virus is one of the most common urogenital infections. But until the disease has external symptoms, it is impossible to detect it without special studies. It is impossible to say that this is bad, because until there are no manifestations, it is too early to draw conclusions about the possible consequences. There is a possibility that the disease may not manifest itself at all, which means that its treatment will be pointless, because even papillomas that appear on the body and mucous membranes can disappear without a trace after a while.
Read also:
Diagnostics
When symptoms have already appeared and the patient consults a doctor about them or in connection with another problem, a gynecologist or urologist will definitely pay attention to the appearance of growths in such unusual places as the genitals and anus during a physical examination. If such neoplasms appear in the mouth (larynx and vocal cords), their occurrence may also interest a therapist or ENT specialist.
When examining women, suspicion of the papilloma virus may fall when cervical erosion is detected (especially if it has not been treated for a long time), hyperplastic processes at the entrance to the cervical canal, cystic formations that are actively increasing in size. In men, a urologist or andrologist will pay attention to the appearance of spots and plaques in the area of the head and body of the patient's penis.
A physical examination of the affected area allows one to suspect (with sufficient accuracy) a papillomavirus infection. But at the same time, the doctor cannot determine by eye which strain of the virus caused the appearance of specific external symptoms. Usually, with HPV type 18 or 16, flat condylomas appear on the mucous membrane, but in most cases, several strains of the virus are detected in one patient at once, which means that pointed condylomas (single or multiple) and anogenital warts can also appear on the mucous membrane.
In such conditions, it is very difficult to determine what types of the virus a particular patient has. But this must be done, because in addition to safe low-oncogenic strains, types with medium or high oncogenicity can also be detected, which can turn a harmless neoplasm into a cancerous tumor.
HPV diagnostics are not limited to external examination only. To detect the virus in the body and determine its type, the following is practiced:
- Study of the tissues of the mucous membrane of the internal genital organs using a special microscope (colposcopy). This method allows you to carefully examine the lesions and identify not only pointed condylomas (they are usually visible to the naked eye), but also flat ones. Using colposcopy, doctors can carefully study tissues with dysplastic processes and their reaction to special reagents (Schiller test): Lugol's solution or vinegar (3% aqueous solution). If there are malignant cells, the affected area acquires a whitish tint.
- Smear microscopy (cytological examination of biomaterial taken from the surface of the vaginal mucosa, cervical canal or urethra). Cytology in the case of papillomavirus infection does not play a decisive role in diagnosing the disease. However, it allows one to identify modified cells (koilocytes and dyskeratocytes) and judge the degree of development of the malignant process based on their number.
- Histological examination is also tissue microscopy, but the biomaterial is no longer mucus, but a small piece of the affected epidermis and deeper tissues taken during a gynecological or urological examination (biopsy). Such an analysis is carried out if cytology shows a questionable or positive result. This is the most accurate method for detecting oncological diseases.
- Blood test for antibodies. This test is indicative even when there are no external manifestations of a viral infection yet, but the virus has already entered the human body and can circulate hematogenously (through the blood). The test allows you to identify the human papillomavirus, but it cannot determine the degree of infection (quantitative indicators of virions) and the type of virus directly with 100% accuracy.
- PAP test. This test is relevant not only for women with suspected cervical cancer, but also for detecting HPV 18 in men. Like dysplasia foci, neoplasms on the penis are lubricated with a 3% solution of acetic acid. A positive test for HPV 18 will show the correct vascular network in the area of application of the reagent.
- HPV Digene test or hybrid capture method. An innovative technique that allows differentiating highly oncogenic strains of the papilloma virus from low oncogenic ones. Two tests are performed. One (395) identifies low oncogenic HPV types, and the other (394) identifies high oncogenic HPV types, including HPV 18 and 16.
Usually this study is carried out in combination with a cytological analysis of the smear.
- PCR analysis (polymerase chain reaction, PCR test) is not a new, many times proven method of detecting highly oncogenic types of human papillomavirus: HPV 18, 16, 31, 33, 56, etc., allowing to detect dangerous diseases already at early stages. As a biomaterial a smear from a mucous membrane is used, less often blood or urine.
Today, PCR testing is the most popular and accurate analysis that allows you to isolate the DNA of the virus. It determines not only the type and kind of the virus, but also its quantity.
The structure of the PCR test distinguishes between:
- PCR HPV 16 and 18 qualitative (determination of highly oncogenic strains of the virus)
- HPV PCR with genotyping (determination of the virus genotype, which is necessary for effective treatment, taking into account the resistance of the identified strain to drugs),
- HPV 18 quantitative PCR (determination of the degree of infection or the number of virions) and some other research options, including combined ones.
A qualitative type of research allows to determine only the presence of a certain strain of the virus in the body. The decoding of the results for HPV 18 or another type of virus will contain one of the words: "positive" or "negative". For example, HPV 16 18 positive (+), if fragments of the DNA of the virus were detected in the biomaterial, or HPV 16 18 negative (-), if none were detected.
To find out how serious the situation is when identifying highly oncogenic strains of the virus, it is necessary to conduct an additional quantitative analysis. Here, everything will depend on the person's immunity (both general and local). The weaker the immune system, the greater the number of virions in the biomaterial will be detected.
The analyzer during PCR testing allows to detect more than 0.3 copies of HPV DNA per ml, which is considered the norm for HPV 18, since a smaller number of copies no longer has clinical significance and is not capable of causing serious pathology.
The detection of a minimal amount of papilloma virus DNA in itself indicates good immunity. But it is also possible that the infection could have occurred quite recently (in this case, the PCR result will be declared doubtful), so after a while, on the recommendation of a doctor, it is worth taking a repeat test.
When it comes to cervical cancer, the most common types of papillomavirus infection that appear in research results are 16 and 18. What is the difference between HPV 16 and HPV 18, since both types of the virus are considered highly oncogenic and are blamed for the development of cervical cancer? It must be said that the degree of oncogenicity of these strains of the virus is not the same. According to some Internet sources, HPV 16 is considered the most dangerous, accounting for 50% of cases of cancer detection, while HPV 18 is the culprit of this dangerous disease in only 10% of cases.
However, foreign scientists, having conducted a number of studies, came to the conclusion that the culprit of the development of invasive adenocarcinomas (and it is this type of cervical cancer that doctors detect in most patients) in most cases is still HPV-18, and in those cases where both strains of the virus are detected, the 18th type contributes to the rapid progression of the disease. In the case of non-invasive types of glandular cancer, affecting not only the reproductive system, but also other organs, the leading role belongs to HPV-16.
The appearance of early dysplastic processes in the uterus during studies in some cases was observed even before the introduction of the HPV 16 genome into the cell, and this indicates that the integration of this type of virus into the cells of a living organism is not a necessary condition for the development of the disease. The pathological process begins even before its first signs appear.
But the development of severe grade 3 cervical dysplasia, often developing into invasive adenocarcinoma, in most cases implied the integration of HPV 18 and other types of papillomavirus infection, causing pathological processes in the uterus (highly oncogenic HPV 31, 33, 52b, 58 and low-oncogenic HPV 6 and 11), into the cell. This is necessary to transfer its genetic information to it, the information that will subsequently change its properties and turn it into a cancerous tumor.
But even the introduction of a highly oncogenic virus into a cell does not always cause cancer. Only 1 in 100 women with dysplasia is subsequently diagnosed with cervical cancer. Everything depends on the duration of the virus's presence in the body and its ability to express the carcinogenic genes E6 and E7 (their introduction into the host cell genome and the transfer of information causing mutations), activation of the mechanisms of transformation of the female sex hormone estradiol into 16α OH sterone, the presence or absence of multiple mutational damage to the chromosomes of a living cell. Thus, oncological diseases against the background of papillomavirus infection develop only with the simultaneous interaction of several factors that create fertile ground for the initiation of the process of malignant degeneration of cells.
Prevention HPV type 18
Palillomavirus infection is a problem that is close to many people. And this is supported by relevant Internet resources, where those who have been diagnosed with highly oncogenic types of the virus share their troubles and ask for advice on what to do next, how to fight this small parasite that can cause a terrible disease.
Those people who have carriers of the virus in their family or among close friends are no less concerned. Their posts convey concern for the lives of their loved ones, but at the same time they are concerned about their health, realizing that the virus is quite contagious. And although the main route of transmission of the virus is considered to be sexual (especially in the presence of external manifestations), which means that the danger is mainly for sexual partners, people understand that HPV virions can also be found in the blood or other physiological fluids and secretions of the patient. This is what scares many, forcing them to limit communication with the virus carrier.
In fact, the risk of transmission of infection by contact is minimal. There is no precise evidence that the contact-household route is relevant in this case, so doctors do not take it into account at all. When kissing, the virus can be transmitted only if one of the partners has papillomavirus neoplasms in the throat, but even there it usually ends up as a result of oral sex. That is, everything again comes down to sexual contact: oral, vaginal and rectal, which can settle the virus in the rectum.
And again, the presence of the virus in the body is not an indicator that a person will subsequently become a client of an oncology clinic. It is worth remembering the fact that among women with HPV 16 or 18, only 1% get cervical cancer, so you should not be too upset about contracting the virus and put an end to your life in advance. Depression and unnecessary worries can only worsen the situation.
It is much more logical to regularly visit a gynecologist or dermatovenerologist, undergo the course of treatment prescribed by them and in the future be more selective in choosing a sexual partner.
What preventive measures can be recommended to those who have not been diagnosed with papillomavirus infection, so that it is not detected in the future:
- Once a year, or better yet, every six months, you need to undergo an examination by a gynecologist (women) or urologist/andrologist (men), even if there are no symptoms of the disease. Such an examination is especially important for those who have had cases of cancer in their family, which indicates a predisposition to them.
- We recommend being more careful when choosing a sexual partner. Let it be one, but a reliable partner who will not run to the side, than many dubious ones. It is necessary to remember that a person may not even suspect his illness, but already be a source of danger, being a virus carrier. For example, women cannot visualize the condition of the mucous membrane of the internal genital organs, which means that even the appearance of internal condylomas can remain unnoticed for a long time. And a man, even in the absence of external manifestations, should understand that for a partner with weakened immunity, he is still a risk factor for infection, because even 1 virion is capable of subsequently reproducing a huge number of clones.
- If one of the sexual partners has HPV 18 or 16, but during the exacerbation of the infection, he should limit sexual contacts until the signs of the disease disappear. In the future, it is recommended to use such a reliable means of protection against various infections as a condom. The question remains whether a condom can completely delay the spread of infection, but the risk of infection is much lower, which is also important.
- Intimate hygiene before and after sexual intercourse is also considered a preventive measure against infection. And this applies not only to viruses, but also to no less dangerous infections that cause sexually transmitted diseases.
- Strong immunity is the main condition for the health of the body, because our immune system, if it works properly, can protect us from various misfortunes. And even if highly oncogenic types of papillomavirus manage to penetrate deep into the body's tissues, the immune system will not allow them to multiply and provoke pathological processes. Any infection can be active in the body only against the background of reduced immunity. This means that we must first of all take care of the health of the immune system.
Proper nutrition, a healthy and active lifestyle, giving up bad habits, hardening procedures, timely treatment of any diseases to prevent them from becoming chronic, which severely affects the immune system - this is the key to strong immunity and prevention of viral diseases of any etiology.
- Since stress is considered a strong factor that weakens the body's defenses, one must learn to react correctly to stressful situations. If a person cannot cope with his feelings and emotions on his own, it is never a shame to seek help from a specialist - a psychologist, which has long been practiced in foreign countries, but still has not become fashionable in our homeland.
- Vaccination is one of the most reliable ways to prevent many infections. Nowadays, many vaccines have been invented for various diseases, and papillomavirus infection is no exception. And if earlier the vaccine acted mainly against HPV types 6 and 11, today there are already several vaccines that can prevent infection with highly oncogenic HPV types 16 and 18.
Let's talk in more detail about vaccination, which should be understood not as a therapeutic measure, but as a preventive measure against viral infection. In foreign countries, this practice has already been put on a wide footing. For example, in Finland, the HPV vaccination is considered mandatory for all girls who turn 10 years old.
In our country, vaccination is voluntary. Doctors can only offer such a preventive measure, and the person himself decides whether he can afford to buy the vaccine, the cost of which is from 750 hryvnia and above.
Today, doctors offer our compatriots mainly 2 types of vaccines that can prevent infection with the main types of papillomavirus, which cause the appearance of neoplasms on the mucous membrane of the genitals (6, 11, 16 and 18). These are the vaccines "Gardasil" and its cheaper analogue "Cervarix".
The preventive course consists of 3 injections. The interval between the first and second vaccinations is 1 month. The third injection is given six months after the first. The procedure lasts about an hour, during which doctors give the injection and observe the patient's reaction. Vaccination of children under 18 years of age is carried out only in the presence of their parents. After the full vaccination course, the patient remains protected for 3-6 years, regardless of age.
Vaccine manufacturers recommend starting vaccination at the age of 9-10 years, as stated in the instructions for the drugs. But doctors believe that such a measure will be relevant for all girls, young women and women aged 9 to 26 years, as well as for boys aged 9 to 15-17 years. If desired, men who care about their health can also seek vaccination at a young age (the Gardasil vaccine). The effectiveness of both vaccines is about 99%.
It should be said that if the infection is already present in the body, vaccination will not be of any use, since it does not affect the course of the disease. Treatment of a viral infection should be carried out with other drugs intended for this purpose. And vaccination is an effective preventive measure.
But this measure has its downsides. Teenagers who have been vaccinated begin to feel invulnerable, neglect basic contraceptive measures (we are talking about condoms), do not think much about the health of their sexual partner, "collect" sexual partners, etc., believing that they are not in danger. Over time, such behavior can become a habit, but the vaccine has a limited duration of action, and doctors usually give a 99% guarantee for 3 years. Further, such indiscriminate sexual behavior can lead to infection with the papillomavirus.
Forecast
The prognosis of diseases caused by papillomavirus infection depends on many factors, the main ones being hereditary predisposition and hormonal background. This is especially relevant for women who have impaired synthesis of the female hormone estrogen and its metabolism. The earlier the infection is detected, the easier it is to prevent the unpleasant and dangerous consequences of its reproduction.
But even if the patient has already developed external symptoms of the disease, this is not a reason to panic. Firstly, in the absence of HIV infection, the disease retreats even from taking immunomodulators, especially if the formed condylomas and anogenital warts are treated beforehand. The worst prognosis is for people with immunodeficiency, because their body is simply not able to fight the infection, so any infectious diseases in such patients proceed with complications.
Secondly, the appearance of condylomas or the development of dysplastic processes in the uterus itself does not indicate oncology. Usually, at least 5 years pass before a benign neoplasm turns into a malignant one. During this time, you can successfully undergo more than one course of treatment, which can prevent such dangerous consequences.
It is another matter if a woman does not see a doctor for 5-10 years after contracting the papillomavirus infection, and the disease progresses. But there is one point here, the danger of cervical cancer is often overestimated. If the disease is detected at the first stage, the survival rate in this case is 90-92%, which is significantly higher than many other cancers. However, at the third stage, the probability of successful treatment is already reduced threefold.
It should be said that women (not to mention men) have time to prevent possible complications of HPV 18. The process does not develop rapidly, which means there is always a chance to stop it before the onset of sad consequences. And although it is very problematic to remove the virus from the body, there is always a way to minimize its negative impact.
A bit of history
Until the end of the 19th century, humanity was at a loss. People were sick and dying, but doctors could not understand what was causing more and more new diseases that could not be treated with the drugs that existed at that time. Some people died from the flu, while strange pointed growths appeared on the bodies of others. And doctors could not answer what caused these pathologies, because laboratory studies of that time could not identify the pathogen.
And such an elusive pathogen turned out to be viruses. This word was used to describe microscopic particles, the size of which turned out to be a hundred times smaller than the size of a bacterial cell. They were discovered by the Russian scientist Dmitry Iosifovich Ivanovsky in 1892, although the name of the new form of life was given somewhat later.
Since then, developments in science began to actively appear, which in the 20th century was already called virology. It was during this century that many viruses were discovered, which turned out to be the causative agents of yellow fever, smallpox, poliomyelitis, acute respiratory viral infections and influenza, HIV infection, cancer, etc.
It should be said that humanity learned about papillomavirus infection far from the 19th century. Mentions of condylomas and warts can be found in the works of ancient Greek doctors (first century BC). It was also noted there that the disease is transmitted sexually. But the causative agent of condylomas itself could not be found for another two decades.
It was only in the middle of the 20th century that it became known that the cause of wart-like growths on the skin and mucous membranes was a virus, when these microscopic particles were isolated from warts, and later from papillomas that formed on the mucous membrane of the genitals. But the papilloma virus was first isolated in 1933 thanks to the American virologist Richard Shope.
Further development of virology as a science has shown that there is not one, but several types of HPV. They are called HPV 6, HPV 18, HPV 35, HPV 69, etc. Some types, having entered the human body, take root, but do not manifest themselves in any way. Almost all of us have them, but we do not suspect that we are carriers of the virus. Other types can be called not just parasites, but enemies of man, since they are capable of causing the most dangerous diseases.

