Medical expert of the article
New publications
Human papillomavirus: structure, life cycle, how it is transmitted, prevention
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
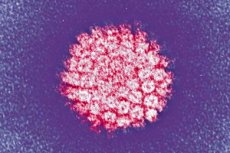
One of the most common infections is the human papilloma virus. Let's look at its main types, the risk of oncogenicity, symptoms, diagnostic and treatment methods.
HPV is a highly specific infection in relation to the human body from the Papovaviridea family, i.e. papoviruses of subgroup A. Every sixth person on the planet is its carrier. The small thermostable pathogen survives well in the external environment and is resistant to heat treatment. It has a high ability to infect multilayered epithelium: skin, mucous membranes, cylindrical epithelium of the lungs, prostate and cervical canal.
Today, medicine knows more than 120 serotypes of the virus, 35 of which affect the skin and mucous membranes. Some serotypes are oncogenic, that is, they are capable of causing cancerous degeneration of affected tissues.
- Low oncogenicity – 6, 11, 42, 43, 44, 73.
- High oncogenicity – 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68.
Once in the human body, the virus spreads through the bloodstream, penetrates the cell's DNA and disrupts its normal functioning. The infected cell begins to actively divide and grow, causing characteristic growths to appear on the affected area.
According to medical statistics, HPV infection is most common when transmitted during sexual intercourse. In the last 7-10 years alone, the number of infected people has increased more than 10 times. The disease requires comprehensive diagnostics and treatment.
Structure human papillomavirus
HPV has small virions without a membrane shell, with a diameter of no more than 30 nm. That is, its size is 5 times smaller than the flu virus and HIV, which have a membrane shell. The genetic material of the papillomavirus is DNA, which has about 8,000 base pairs and many protein compounds. The genome is a double-stranded molecule packed with histomes, that is, cellular proteins that participate in the compaction of DNA in the nucleus.
The virus genes encode several types of proteins, each of which performs specific functions in its life cycle. Early proteins (E), which are responsible for regulatory functions and the proliferation of infected cells, and late proteins (L), which perform structural functions, are distinguished.
The following types of proteins are responsible for the structure of the virus:
- E1-E8 – participate in DNA replication, are synthesized immediately after infection. Manifested by granularity of the skin, in which they accumulate.
- L1-L2 – form the structure of the virus. They are responsible for the formation of the outer shell (capsid), which penetrates the stratum corneum of the epidermis.
Of particular danger are protein structures involved in oncogenesis:
- E6 – disables the tumor suppressor p53 of healthy cells, causing excessive proliferation of cellular structures. E6 leads to a sharp decrease in p53 and degenerative processes.
- E7 – binds Rb, that is, an oncosuppressor responsible for slowing down the enzymatic reactions of uncontrolled cell division.
E6 and E7 lead to uncontrolled cell growth, causing tumor formations. At the same time, the E2 protein stops this pathological process, but this ability is lost immediately after the genome infects a human cell.
Due to its complex structure, HPV is difficult to cultivate in the laboratory. This is because virus particles are formed only in living organisms or complex organotypic cultures that are similar to human cells.
Life cycle human papillomavirus
The infectious process and life cycle of the human papilloma virus are based on the self-reproduction of infectious virions. In the normal course of the pathological process, there is a close relationship between the replication cycle of viral DNA and the life cycle of an infected cell of the human body. The papillomavirus disrupts the replication of cellular DNA, laying down a program for the reproduction of its own infected cells with increased infectious activity.
In the process of inhibiting replication, there is a high probability of altering the infection cycle and transforming it into a malignant tumor. If the life cycle is disrupted or interrupted, then the production of infectious virions becomes impossible.
In an infected cell, HPV exists in two forms:
- Episomal – located outside the chromosomes of the infected cell, has a low risk of oncogenicity.
- Integrated – viral DNA is incorporated into the cell chromosome. This form is malignant.
Depending on the intracellular form of infection, the following variants of the infectious process are possible:
- Latent (hidden) course – HPV in episomal form, but does not cause pathological changes and has no clinical manifestations.
- Papillomas are an infection in an episomal form. The number of cells in the basal layer increases, which leads to the appearance of skin growths of various localizations.
- Dysplasia – virions are in episomal and integrated form.
- Carcinoma – the virus is in an integrated form. Atypical cells appear, indicating the development of malignant processes in the body.
The incubation period from infection to the appearance of the first symptoms can range from ½ month to several years. In this case, several genotypes can develop in the body at the same time. In some cases, self-healing occurs within 6-12 months after infection, i.e., a violation of viral DNA replication.
How is the human papillomavirus transmitted?
HPV is transmitted from a sick person to a healthy one. Infection occurs through close household contact, during sexual intercourse or during the birth process from mother to child.
There are the following ways of infection penetration into the body:
- Contact with infected skin or mucous membranes.
- Use of personal items of an infected person.
- Wearing the patient's shoes or clothes.
- Visiting saunas, swimming pools and other public places with high humidity.
According to medical statistics, the most common way of transmitting HPV is unprotected sexual intercourse. Infection occurs regardless of the type of contact (vaginal, oral, anal). The virus enters the body through microdamage to the mucous membranes and epidermis. If growths occur in the oral cavity, this may indicate infection during a kiss or oral sex. Men infect women more often. Infection is possible only in the presence of papillomas and warts on the genitals.
When infected from mother to child, papillomatosis is transmitted intrapartum or when the child passes through the birth canal. The infant may develop anogenital wart-like growths and condylomas on the inner surface of the larynx and pharynx, complicating the breathing process. Infection can also occur during lactation. Household transmission routes of the virus are extremely rare. This is due to the fact that the infection does not exist in the environment for long.
Since the human papilloma virus is not highly contagious, infection occurs under the influence of certain factors:
- Decreased immune system defenses.
- Violation of the barrier functions of the epidermis or mucous membranes.
- Disruption of the intestinal or vaginal microflora.
- STD (papillomatosis is a secondary infection).
- Exacerbation of chronic diseases.
- Frequent stress or harmful working conditions.
- Failure to comply with personal hygiene rules.
- Use of drugs that suppress the immune system.
During a person's life, he or she can be infected with several genotypes of infection at the same time. The action of the above factors leads to the activation of the infection. The infected cells begin to actively multiply, causing skin growths of various shapes and localizations.
 [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ]
[ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ]
Immunity
Today, papillomatosis is one of the most common diseases. People with a strong immune system can be carriers of the virus for a long period of time without even knowing it.
It is the immune system that acts as a factor in protecting the body from pathogenic microorganisms. A timely immune response leads to the destruction of the pathogen, which does not have time to infect the basal cells of the epithelium.
There are a number of factors that undermine the immune system and contribute to infection and activation of the virus:
- Frequent respiratory viral infections and infectious and inflammatory lesions of the body.
- Intense physical activity.
- Psycho-emotional stress and strain.
- Hypothermia.
- Abuse of alcohol, smoking and other bad habits.
Reduced immunity ensures active growth of papillomatous neoplasms. In order to prevent this, it is recommended to take immunomodulators and vitamins, which promote a speedy recovery and elimination of the virus from the body.
Prevention human papillomavirus
It is much easier and more important to prevent any disease than to treat it. Prevention of the human papilloma virus is based on a healthy lifestyle and strengthening the immune system. It is the immune system that plays a decisive role in the emergence of HPV infection. When the body's defenses are weakened, it weakens, creating a favorable background for infectious lesions.
Prevention of papillomatosis and other diseases comes down to these simple rules:
- Healthy lifestyle.
- Absence of bad habits.
- Proper balanced nutrition.
- Protected sex and a regular partner.
- Absence of stress and other emotional shocks.
- Timely treatment of any diseases.
- Vaccination.
- Regular preventive examinations with a doctor.
The above recommendations relate to the first level of prevention. There are special vaccines to prevent infection with HPV with a high carcinogenic risk. They contain viral proteins-antigens, under the influence of which the body produces specific antibodies that help destroy the infection when it occurs.
There are also secondary preventive measures, which include: visual and cytological screening to detect the virus and track the dynamics of its development. If the results of these tests are positive, the patient is prescribed a comprehensive set of diagnostic tests. As a rule, these are PCR, biopsy, colposcopy and a number of other methods.
Tertiary prevention is carried out in case of infection with high oncogenic risk HPV. The patient must take a smear test for cytology every six months for three years after infection. If the results are negative, the test is taken once a year for the rest of the patient's life.
Vaccination against human papillomavirus
One of the methods of preventing papillomatosis is vaccination. Vaccination against the papilloma virus is used to prevent infection with HPV with a high carcinogenic risk - these are types 16 and 18. Vaccination is advisable to be carried out before the first sexual contacts, that is, in adolescence from 16 to 23 years old.
It should be taken into account that if the virus is already present in the body, the effect of the injection is zero. But many scientists believe that the introduction of the vaccine to already infected patients alleviates the course of the virus and speeds up the recovery process.
Vaccination involves inoculation with one of the following drugs:
- Cervarix
An adsorbed recombinant vaccine for the prevention of diseases caused by the human papilloma virus. It contains a mixture of virus-like particles of strains 16 and 18. The effectiveness of the drug is based on its adjuvant system. Provides cross-protection of the body from any manifestations of HPV that can be detected cytologically.
When undergoing a full vaccination according to a special schedule, the drug promotes the formation of specific antibodies to the virus in the body. Immunoglobulins are detected in 100% of patients who have undergone a vaccination course.
- Indications for use: prevention of cervical cancer in female patients aged 10-25 years, prevention of acute and chronic infections associated with Human papillomavirus, as well as cellular pathologies, including the development of flat atypical cells of unknown etiology, cervical intraepithelial neoplasia and precancerous conditions in patients aged 10-25 years.
- Method of administration: the vaccine is administered in the deltoid muscle area. Intravenous and intradermal administration are contraindicated. Before vaccination, the preparation should be organoleptically tested and shaken thoroughly to obtain an opaque white suspension. The medicine is administered in three stages with a single dose of 0.5 ml. For primary vaccination, the schedule is 0-1-6 months.
- Side effects: pain at the injection site, increased fatigue, dizziness, gastrointestinal and musculoskeletal disorders, skin allergic reactions. There is also a risk of anaphylactic reactions.
- Contraindications: hypersensitivity to vaccine components, acute hyperthermia, relapses of chronic diseases. Vaccination should be carried out with special caution in case of thrombocytopenia and disorders of the blood coagulation system. The vaccine is not suitable for the treatment of existing lesions caused by HPV types 16 and 18. Cervarix injections are not carried out during pregnancy and lactation. No cases of overdose have been recorded.
The vaccine is available in a single-dose syringe. The drug should be stored in the refrigerator for three years from the date of manufacture.
- Gardasil and Gardasil 9
The drug Gardasil is an antigen set of papillomaviruses of types 6, 11, 16 and 18. It helps activate the immune system to form antiviral antibodies and provide immunological protection of the body. Gardasil®9 is a 9-valent recombinant vaccine against the human papillomavirus. It is active against the following strains of infection: 6, 11, 16, 18, 31, 33, 45, 52, 58. Both vaccinations provide cross-protection against genotypes that are not in the drug: 31, 33, 35, 39, 45, 51, 52, 56, 58 and 59.
- Indications for use: prevention of infection with Human papillomavirus, prevention of cancerous and precancerous conditions of the cervix, vulva, anus, penis. Recommended for vaccination of patients from 9 to 45 years old.
- Directions for use: shake the bottle with the solution and check for foreign inclusions. Draw the solution into a syringe and inject intramuscularly into the delta of the shoulder or the anterolateral thigh. After the procedure, the patient must be under medical supervision for 30 minutes. Injections are administered according to specially developed schemes. Standard scheme 0-2-6 month, accelerated 0-1-4 month.
- Side effects: itching, swelling and pain at the injection site, headaches, fever, fainting, anaphylaxis, inflammatory processes in the pelvic organs, thromboembolism, urticaria, gastroenteritis, etc. In case of overdose, the severity of the above reactions increases.
- Contraindications: intolerance to active components, blood clotting disorders, pregnancy and lactation, treatment with anticoagulants.
Gardasil and Gardasil 9 are available as a suspension in vials with a dosage of 0.5 ml each.
The above vaccines are certified and have passed all necessary checks. Vaccination is carried out in outpatient conditions in compliance with the rules of asepsis and antisepsis.
 [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ]
[ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ]
Using a condom to prevent HPV
The main route of HPV transmission is unprotected sex with an infected person. Clinical studies have shown that using a condom to prevent papillomavirus is highly effective. With this method of contraception, infection occurs in approximately 30% of cases. The risk of infection during sex without using a condom is 90%. HPV transmission through a condom more often occurs after anal sex, not vaginal sex.
It should also be taken into account that pathogenic microorganisms are present in all biological fluids of the human body: saliva, mucus, etc. Therefore, if one of the partners has growths characteristic of the disease on the mucous membrane of the oral cavity, then infection is possible not only during oral sex, but also during kissing.
As for sex during the treatment of papillomatosis, intimate relations are possible after destructive methods of sanitation of papillomas, condylomas or warts and after a course of antiviral treatment to suppress the activity of the infection. In this case, sex should only be with the use of barrier contraception to prevent repeated relapses or infection of the partner.
Forecast
Human papillomavirus is one of the most common diseases with a latent course. The prognosis of this pathology when infected with strains with low and medium oncogenicity is favorable. If there was an infection with HPV of the third group (high carcinogenicity), the outcome of the disease depends on its early diagnosis and treatment.

