Medical expert of the article
New publications
Tests for human papillomavirus: how to pass, deciphering
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The human papillomavirus is a serious threat. Diagnostics are necessary to determine the strain of infection and the risk of its oncogenicity. Such information allows us to create the most appropriate and effective treatment plan.
High-quality diagnostics are carried out by several specialists simultaneously. The main indications for examination of the body are:
- Active sexual life and frequent change of sexual partners.
- Itching, burning in the genital area, atypical discharge.
- The appearance of new growths on the skin and mucous membranes in the form of papillomas, warts and condylomas.
Diagnosis of papillomavirus consists of a complex of laboratory and instrumental methods:
- Visual examination and anamnesis collection – the doctor examines the affected areas and asks about when the rash or other signs of HPV first appeared. Assesses the type and shape of the neoplasms. If there are anogenital growths, an examination of the cervix and urethroscopy are performed.
- Cytology of smears and scrapings – is performed to establish morphological changes at the cellular level associated with HPV. The accuracy of this method depends on the technique of collecting the material and the qualifications of the laboratory technicians.
- Colposcopy is an examination of the mucous membrane to detect subclinical forms of infection. The diagnosis is confirmed by the presence of the following factors: leukoplakia, mosaic, puncturation, zone of abnormal transformations.
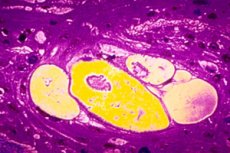
- A biopsy is the removal of a small amount of affected tissue for microscopic examination. It is usually performed when there is a suspicion of cervical involvement.
- Histological examination – the material obtained as a result of the biopsy is sent for laboratory study to identify precancerous conditions and other cellular abnormalities.
- PCR – is performed to identify individual HPV types. Blood, urine, mucus and other tissue fluids are used for diagnostics.
- Digene test is one of the most reliable diagnostic methods. It has high sensitivity to Human papillomavirus. It allows to determine the genotype and its belonging to the high-oncogenic or low-oncogenic group.
Today, there are many methods that allow you to detect HPV infection and determine the degree of its aggressiveness.
Screening for human papillomavirus
A mandatory test for patients with a predisposition to malignant processes in the body is screening. Human papillomavirus is also a reason to undergo this laboratory test.
The first screening is recommended for women at the age of 30. The analysis is necessary to detect not only the papillomavirus, but also to prevent erosive lesions of the cervix associated with HPV.
Most often, patients are prescribed the following types of screening:
- Cytological PAP test – a cervical scraping placed in a liquid medium is used for the study. It helps to identify oncological HPV strains at an early stage of development.
- Extended – identifies genotypes with high oncogenicity and their concentration in the body.
- Polymerase chain reaction has high diagnostic value, since it allows to identify all types of Human papillomavirus.
HPV screening is performed both during diagnosis of the disease and during therapy and to evaluate the results of treatment.
Human papillomavirus test
If papillomavirus is suspected, all patients are prescribed a set of diagnostic procedures. HPV analysis is the determination of the type of virus in a laboratory setting. Various biological fluids and tissues are used for the study.
Most often, a smear from the genitals is taken for analysis. Taking material from this area is necessary even in the absence of visual symptoms of papillomatosis. The resulting biopsy is examined under a microscope for epithelial cells altered by the virus. Based on the diagnostic results, the type of infection and the risk of its oncogenicity are determined.
It is mandatory to take a test for papillomatous infection when planning a pregnancy, to determine the causes of infertility and pathologies of gestation. In this case, the test is prescribed for both partners at once. This is due to the fact that the virus is transmitted during intimate contact. Based on the results of the study, the doctor can prescribe additional diagnostic methods and draw up a treatment plan.
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ]
Quantitative analysis for human papillomavirus
To detect the papillomavirus, determine its type and degree of activity, a quantitative analysis is carried out. There are several methods for determining HPV, let's consider them:
- Polymerase chain reaction – PCR is the standard for HPV diagnostics. The analysis is based on increasing the number of copies of viral DNA in a biopsy. This method allows for the detection of even single types of the virus with high accuracy.
- Digene test – the peculiarity of this method is the reliable detection of genotypes with increased oncogenicity. Various biological fluids and materials are used for analysis.
- Determination of the presence of viral antibodies - the analysis reveals specific proteins of the immune system. Each viral agent that enters the body promotes the production of unique immunoglobulins. If antibodies to Human papillomavirus are detected in the blood serum, this indicates infection of the body.
To conduct a quantitative analysis, capillary blood (from a finger), scrapings from the skin and mucous membranes, and tissue biopsies are used. 12 hours before taking the tests, you should stop taking antifungal, antiviral, antimicrobial and other medications, including contraceptives. On the day of diagnosis, you need to take a shower and thoroughly wash your intimate areas if scrapings are taken from them. Also, 2-3 days before the procedure, you should refrain from sexual intercourse.
The attending physician interprets the results obtained. The doctor takes into account not only the data of the diagnostics performed, but also the clinical manifestations of the disease. Otherwise, the results may be misinterpreted.
Human papillomavirus DNA, PCR
One of the most common and reliable methods for detecting human papillomavirus DNA is PCR. Various biological materials are used to conduct the polymerase chain reaction: blood, urine, smears from the mucous membrane, amniotic fluid. The analysis allows you to establish the presence of infection even if it is latent in the body.
The principle of this diagnostic method is based on the isolation of human and viral DNA. Any deoxyribonucleic acid consists of four nucleotides:
- A – adenine.
- T – thymidine.
- G – guanine.
- C – cytosine.
According to the rules of genetics, they have a certain order of combination: A+T, G+C. All living organisms have their own DNA, which can be isolated. PCR recognizes fragments of pathogenic DNA, thereby isolating the pathogen.
Advantages of PCR:
- Universality – in addition to Human papillomavirus, many other pathogens of infectious diseases can be detected during the study.
- High sensitivity – in addition to determining the presence of the virus, the method determines its type and other characteristics.
- Effectiveness – reliably identifies the required infection.
- Speed – test results can be obtained within 24 hours of taking the test.
Preparation for analysis:
- You should stop taking birth control pills one week before the scheduled test, as they may interfere with the results.
- The study is not performed during menstruation and for 3 days after it.
- You should avoid sexual intercourse two days before the test.
- The diagnostics are performed on an empty stomach, the last meal should be 12 hours before the analysis. But you can drink water.
- On the day of taking the HPV PCR test, it is not recommended to perform hygiene procedures or go to the toilet to pee two hours before collecting the material.
The results obtained should be interpreted by a doctor. An indicator of up to 3 Lg is an insignificant concentration of the pathogen, 3-5 Lg is a clinically significant concentration, and more than 5 Lg is high. Normally, all quantitative titers should be negative. But negative results do not always indicate the absence of the disease. This is often observed with insignificant concentrations of the virus in the body and when it is suppressed by the immune system.
Despite all the advantages, PCR has a number of disadvantages. The analysis should be taken only in a modern laboratory to avoid false results. Particular attention should be paid to the collection of material. Only a doctor should decipher the results, since positive results may occur after recent treatment of an infection.
Scraping for human papillomavirus
To detect genital HPV infection in men, a scraping is performed, that is, a Digene test. The material is collected from the urethral canal using a special brush; in some cases, tissue is taken from the head of the penis. Before taking the test, you must take a shower and wash yourself thoroughly. Violation of personal hygiene negatively affects the results of the test.
In women, a scraping is taken from the cervix if dysplasia, erosion, and other pathological processes caused by HPV are suspected. To collect the material, the doctor removes vaginal discharge and inserts a small brush into the organ, rotating it around the axis in the cervical canal. After all manipulations, the brush is placed in a test tube with a medium and sent to the laboratory.
The obtained materials are sent for differential diagnostics using the PCR method; cytological screening is not performed. The results are ready 2-3 days after the analysis. The obtained data represent complete information about the type of virus, its carcinogenicity and a number of other factors in the course of the disease. If the results are incorrect, the study is performed again. Repeated screening is necessary during treatment and after therapy to determine its effectiveness.
Smear for human papillomavirus
If warts or condylomas are found in the genital area during a gynecological examination, the doctor takes a smear for HPV. The doctor runs a special brush over the affected tissues. The smear is taken from the cervical canal in women and from the urethra in men. The collected biopsy is sent to the laboratory for examination.
The following types of smears are used when Human papillomavirus is suspected:
- PCR – detects the infection’s DNA. To perform this analysis, a scraping is taken from the urethra in men, from the vagina and cervical canal in women. Semen or urine can also be used.
- Digene testing is a study of the collected material at the molecular level. Testing is a differentiation of two groups of papilloma infections at the same time - with high and low oncogenicity.
The above studies classify the results into 5 types:
- Absence of atypical cells.
- The presence of altered cells due to the inflammatory process.
- Minimum number of cells with an atypical structure.
- Malignant cells.
- A large number of oncogenic cells.
There is also a classification according to the Bethesda system. It consists of indicators of low and high degrees of changes. In this case, the smear decoding is presented by the following data:
- NILM – normal epithelium.
- ASCUS – altered cells due to dysplasia, inflammation, sexually transmitted infection or HPV.
- ASC-H – abnormalities in the structure of squamous epithelium were detected. This result indicates early stages of oncology or severe dysplasia.
- LSIL – a small number of altered cells are present in the smear. Indicates dysplasia or papillomavirus.
- HSIL – significant changes in the epithelium. Severe dysplasia and pronounced oncology. If this result is ignored, then 7% of patients develop a malignant disease in 3-5 years.
- AGC is atypical glandular epithelium. It occurs in uterine cancer or dysplasia.
- AIS – early stages of oncology.
- High-grade SIL – squamous cell carcinoma.
The speed of obtaining smear results depends on the chosen research method. As a rule, the decoding is ready in 2-3 days.
 [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ]
[ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ]
Antibodies to human papillomavirus
To detect antibodies to HPV, an enzyme immunoassay of blood is indicated. The principle of this study is to determine the presence of immunoglobulins to the infectious agent. Diagnostics using the ELISA method indicates the body's immune response to the virus. Depending on the antibodies detected, the following stages of the disease are distinguished:
- IgM – acute.
- IgG – chronic or recovery period.
- IgA – relapse of chronic infection.
The results of the antibody test are ready 1-3 days after it is taken. When deciphering the results, it should be taken into account that Human papillomavirus can be an indirect trace, therefore, PCR and other tests are carried out to clarify the presence of infection. In addition, ELISA does not establish the genotype or risk of carcinogenicity of the virus.
 [ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ]
[ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ]

