Medical expert of the article
New publications
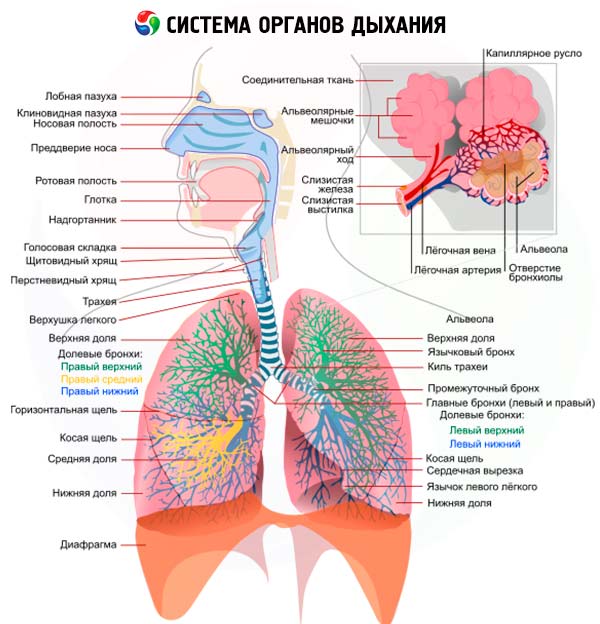
Respiratory study
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Despite the great successes in the development of special methods for studying the condition of the respiratory organs, many methods of physical examination described by R. Laennec are still of primary importance. True, now we try to identify only those symptoms that really have an important diagnostic value, understanding that in some lung diseases (for example, bronchogenic cancer or tuberculosis) the occurrence of these symptoms often indicates a fairly pronounced stage of the disease, and for early diagnosis it is necessary to use more subtle methods.
Another difference of the modern stage of research of the respiratory system is significantly greater attention to the physiology of respiration, the relationship between clinical signs and disorders of external respiration function, and to functional, and not just anatomical, changes.
The current stage of understanding pathological processes occurring in the respiratory organs is impossible without knowledge of those protective mechanisms that prevent the penetration of microorganisms, dust particles, toxic substances, plant pollen, etc. In addition to anatomical barriers (larynx, epiglottis, numerous divisions and narrowing of the bronchial tree), rich vascularization of the mucous membrane of the respiratory tract, cough reflex, a very important role in protecting the respiratory organs is played by mucociliary transport carried out by the ciliated epithelium of the bronchi, as well as the formation of tracheobronchial secretion containing biologically active substances (lysozyme, lactoferrin, a1-antitrypsin) and immunoglobulins of all classes synthesized by plasma cells, but primarily IgA. At the level of terminal bronchi, alveolar ducts and alveoli, the protective function is performed mainly by alveolar macrophages and neutrophilic granulocytes with their pronounced chemotaxis and phagocytosis, as well as lymphocytes that secrete lymphokines that activate macrophages. Broncho-associated lymphoid tissue (BALT), as well as reactions of humoral (immunoglobulins of classes A and G) immunity, are of particular importance in the protective mechanisms of the respiratory organs. An important place in the protection of the lungs is occupied by their full ventilation.
All these mechanisms of respiratory protection can and should now be studied in each individual patient, which allows for a more detailed presentation of the characteristics of the developing disease, and therefore, the choice of more rational treatment.
When examining the respiratory organs (which, as in all other cases, begins with questioning, followed by inspection, palpation, percussion and auscultation ), the main question that needs to be answered is determining the predominant localization of the process: the respiratory tract, the lung parenchyma or the pleura. Often, several parts of the respiratory system are involved at the same time: for example, with inflammation of a lung lobe (lobar, or croupous, pneumonia ), there is almost always inflammation of the pleural sheets ( pleurisy ), with focal pneumonia, the process most often begins with inflammation of the bronchi ( bronchitis ), and then peribronchial inflammation develops. This makes the clinical picture of a number of pulmonary diseases diverse and forces us to evaluate the detected signs from different positions.
Medical history of respiratory diseases
Continuous questioning allows us to identify the features of the development of pulmonary pathology - the anamnesis of the disease. The general principle of "spare no time in getting acquainted with the anamnesis" should be fully used when studying diseases of the respiratory system. The time sequence of the appearance of certain signs of the disease, the features of its initial period, relapses, their frequency and the presence of provoking factors, the nature and effectiveness of the treatment, the occurrence of complications are specified.
Thus, in acute pulmonary diseases, such general symptoms as malaise, chills, fever may be detected several days before pulmonary signs (viral pneumonia) or almost simultaneously with them ( pneumococcal pneumonia ), and acutely occurring severe dyspnea is a very important sign of bronchial asthma, acute respiratory failure, and pneumothorax. It is necessary to evaluate the results obtained using special research methods (sputum and blood tests, radiography, etc.). Of particular importance are indications of the presence of allergic reactions (urticaria, vasomotor rhinitis, Quincke's edema, bronchospasm) in response to the action of such factors as food products, odors, drugs (primarily antibiotics, vitamins); recently, close attention has been paid to the possibility of worsening the course of bronchial asthma when using aspirin and other non-steroidal anti-inflammatory drugs ("aspirin asthma").
An important stage of questioning is an attempt to establish the etiology of the disease (infectious, occupational, medicinal).
A number of serious lung diseases are associated with more or less prolonged contact with various industrial (professional) factors, such as dust containing silicon dioxide, asbestos, talc, iron, aluminum, etc. In addition to the well-known professional dust lung diseases ( pneumoconiosis ), a connection is now increasingly being found between such a lung disease as exogenous allergic alveolitis and numerous environmental factors, such as rotten hay, raw grain, etc. ("farmer's lung", "cheese maker's lung", "poultry farmer's lung", etc.). It is not uncommon for diffuse pulmonary changes to occur in patients receiving medications such as cytostatics, nitrofurans, cordarone and its analogues, as well as long-term radiation therapy for various non-pulmonary diseases.
All the identified features of the course of the disease should ultimately be presented in the form of an appropriate graphic image, an example of which can be the observation of a patient with lobar pneumonia.
Finally, important information can be obtained by studying the family history (family predisposition to bronchopulmonary diseases, such as bronchial asthma, tuberculosis or the presence of a1-antitrypsin deficiency, cystic fibrosis ), as well as bad habits: smoking is a generally recognized risk factor for lung cancer, alcohol abuse contributes to the unfavorable course of pneumonia (suppuration, abscess formation).
Smoking (especially cigarette smoking) plays a special role in the history of lung disease in each individual patient, as it either causes or worsens the disease. Therefore, it is important for the doctor to know (record) both the number of cigarettes smoked per day and the time the patient smokes (the so-called "cigarette pack years"). Chronic bronchitis and pulmonary emphysema, severe forms of chronic obstructive pulmonary disease, are the most common in heavy smokers;bronchogenic cancer, one of the most common malignant tumors in men and increasingly common in women, is directly related to smoking.
Examination of the upper respiratory tract
Direct examination of the respiratory organs often begins with an examination of the chest. However, a preliminary examination of the upper respiratory tract is more correct, due to the important role that various pathological changes in the upper respiratory tract can play in the development of lung diseases. It goes without saying that a detailed examination of the upper respiratory tract is the responsibility of an otolaryngologist. However, a doctor of any specialty (and especially a therapist) must know the main symptoms of the most common diseases of the nose, pharynx, larynx, and be proficient in the simplest methods of examining the upper respiratory tract.
First of all, it is determined how freely the patient can breathe through the nose. To better assess nasal breathing, the patient is asked to close the nasal passages alternately, pressing the left and right wings of the nose successively to the nasal septum. Difficulty in nasal breathing is a common complaint of patients and occurs, for example, with a deviated nasal septum, acute and chronic rhinitis, sinusitis.
They clarify whether the patient has a feeling of dryness in the nose, which may appear in the initial stage of acute rhinitis or be observed constantly in patients with chronic atrophic rhinitis. Patients often complain of the appearance of discharge from the nose. In such cases, their quantity is determined (heavy discharge in acute rhinitis, scanty, with crust formation - in atrophic rhinitis), nature (serous or mucous discharge - in acute catarrhal rhinitis, watery - in vasomotor rhinitis, thick and purulent - in sinusitis, serous - in flu, etc.), and they also note whether the amount of discharge from the right and left nasal passages is the same.
Great attention should be paid to complaints from patients about nosebleeds, which may be associated with local causes (trauma, tumors, ulcerative lesions of the nasal mucosa) or caused by some general diseases (for example, hypertension, hemorrhagic diathesis, leukemia, vitamin deficiency, etc.). If nosebleeds are present, it is determined how often they occur in the patient (episodically or regularly), whether they are scanty or profuse. Scanty nosebleeds most often stop on their own. Profuse nosebleeds (over 200 ml per day) may be accompanied by general symptoms characteristic of all profuse bleeding (general weakness, drop in blood pressure, tachycardia), and require emergency measures to stop it (nasal tamponade). It should be borne in mind that it is not always possible to correctly determine the volume of nosebleeds, since the blood flowing down the back wall of the nasopharynx is often swallowed by patients.
Sometimes patients also complain of a deterioration in the sense of smell ( hyposmia ) or its complete absence. Olfactory disorders can be associated with both difficulty in nasal breathing and damage to the olfactory nerve.
When the paranasal sinuses (frontal, maxillary, etc.) become inflamed, pain may appear in the area of the root of the nose, forehead, cheekbones, sometimes radiating to the temporal region.
A thorough examination of the nasal cavity is performed by an otolaryngologist using rhinoscopy, which involves the use of special nasal mirrors. However, the anterior part of the nasal cavity can be examined quite well without resorting to special techniques. To do this, the patient throws his head back a little, four fingers (II-V) of the right hand are placed on the patient's forehead, and the thumb of the same hand is lightly pressed (from the bottom up) on the tip of the nose. Also pay attention to the presence of pain when palpating and tapping in the area of the root of the nose, its back, and the projection sites of the frontal and maxillary paranasal sinuses. Pain, as well as swelling of soft tissues and hyperemia of the skin in these areas can appear with damage to the nasal bones, inflammatory diseases of the paranasal sinuses.
A full examination of the larynx is possible only with the use of laryngoscopy, which is performed by an otolaryngologist. In cases where the patient is examined by a doctor of another specialty, the patient's complaints are analyzed, indicating a possible disease of the larynx (for example, pain when talking and swallowing, a characteristic barking or, conversely, silent cough), changes in the voice ( hoarseness, aphonia) are identified, breathing disorders are noted (loud, tense, with difficulty inhaling), appearing, for example, with stenosis of the larynx.
When examining the larynx, possible changes in shape are assessed (for example, due to trauma); when palpating the larynx area, the presence of swelling or pain is determined (due to traumatic injuries, chondroperichondritis, etc.).
Additional methods of examination of respiratory organs
To clarify the diagnosis, the degree of activity of the pulmonary process (exacerbation, remission), the functional state of the respiratory system, additional methods of clinical examination are of great importance, such as blood tests (including immunological indicators), urine, but especially sputum analysis, bronchoalveolar lavage fluid, pleural fluid, as well as radiological methods, which in recent years have been supplemented by tomographic and computed tomographic studies, radiocontrast methods (bronchography, angiopulmonography), radionuclide and endoscopic methods (bronchoscopy, thoracoscopy, mediastinoscopy), puncture biopsy of the lungs, mediastinal lymph nodes, special cytological studies. Particular attention is paid to the study of the function of external respiration.
The need to use additional research methods is also related to the fact that in a number of observations, general examination does not reveal changes, especially in the early stages of the disease, which are not clinically manifested (for example, bronchogenic cancer, small tuberculous infiltrate). In these cases, the diagnosis depends on the ability to use additional methods.
Sputum examination
Macroscopic examination of sputum was discussed earlier. Microscopic examination of sputum (stained smears) can reveal a predominance of neutrophils, which is associated with a bacterial infection (pneumonia, bronchiectasis, etc.), which in some patients is subsequently confirmed by the detection of microbial growth during sputum culture, or eosinophils, which is considered characteristic of bronchial asthma and other allergic lung diseases. In bronchial asthma, Curschmann spirals (mucus-containing casts of spasmodically narrowed bronchi) and Charcot-Leyden crystals (assumed to be remnants of eosinophils) can be detected in sputum. The presence of erythrocytes in the smear indicates an admixture of blood as a sign of bronchial or pulmonary hemorrhage. Alveolar macrophages can be detected, which indicates that the material was obtained from the deep sections of the respiratory tract. If they contain hemoglobin derivatives (siderophages, heart defect cells), one can think about the presence of blood stagnation in the pulmonary circulation (decompensated mitral heart defect, other causes of heart failure). General microscopy of sputum can reveal elastic fibers - a sign of destruction of lung tissue (abscess and gangrene of the lungs, tuberculosis), as well as fungal druses. The most important method of studying sputum is the identification of bacteria in smears stained by Gram, which provides valuable information about the cause of the inflammatory process, primarily pneumonia, and allows for a more targeted etiological treatment.
Lavage fluid examination
In recent years, microscopic examination of the fluid obtained by washing (from the English lavage - washing) the walls of the subsegmental bronchi with an isotonic solution - bronchoalveolar lavage fluid (BALF), which is aspirated with the same bronchofibroscope that was used to instill the solution, has become widespread. The normal cellular composition of BALF in non-smokers per 100-300 ml of fluid is represented mainly by alveolar macrophages (up to 90%), band neutrophils (1-2%), lymphocytes (7-12%), and bronchial epithelial cells (1-5%). Important diagnostic conclusions are made based on changes in the cellular composition of BALF, the activity of alveolar macrophages, and a number of other immunological and biochemical indicators. For example, in such a common diffuse lung lesion as sarcoidosis, lymphocytes predominate over neutrophils in the BALF; detection of fungi and pneumocysts allows diagnosing rare variants of bronchopulmonary infection.
Pleural puncture
The examination of fluid obtained by pleural puncture has a certain diagnostic value. Its type (light, transparent, turbid, purulent, bloody, chylous), odor, and relative density of protein content are determined. In the presence of exudate (as opposed to transudate), the relative density and protein content in the obtained fluid are high, respectively, more than 1.015 and 2.5%; currently, instead of the Rivolt test, the ratio of protein content in pleural fluid to protein content in plasma is determined (in the presence of exudate, it is more than 0.5).
X-ray examination methods
Of particular importance in the diagnosis of respiratory diseases are radiological methods, which confirm diagnostic assumptions that arise at previous stages of examination, are reliable during dynamic observation, and in some cases help to clarify the etiology of the disease even before receiving the results of bacteriological and cytological studies. The importance of radiological methods in determining the localization of pulmonary changes and understanding the essence of the process is unconditional. For example, bronchopneumonia and fungal lesions can be determined in any part of the lungs, lobar and segmental changes are primarily characteristic of pneumonia, pulmonary infarction, and endobronchial tumor growth.
Currently, fluoroscopy is used much less frequently, since it involves a higher radiation load, the interpretation of changes is largely subjective, comparative dynamic observation is difficult, although the use of a television screen and video recording of the image allows one to avoid some negative aspects. The advantage of this method is the ability to study the lungs during breathing, in particular the movements of the diaphragm, the state of the sinuses, and the position of the esophagus.
X-ray ( fluorographic ) examination is the most objective, widespread and essentially the main method of additional examination, allowing to obtain accurate data and evaluate them in dynamics. The use of oblique, lateral positions, the position of lordosis (to identify apical localizations), etc. helps to clarify the diagnosis. In this case, the features of the pulmonary parenchyma, vascular and interstitial structure (pulmonary pattern) are analyzed, the roots of the lungs and a number of other parts of the respiratory system are assessed. Changes are specified in more detail during tomography and computed tomography. These methods allow to identify pathology of the bronchi, trachea (in particular, its bifurcations), seals located at different depths. Particularly informative in this regard is computed tomography, which, thanks to the use of a computer, simultaneously in a short time processing data from hundreds of transilluminations of a certain layer of tissue, allows to obtain information about very small and difficult to access for conventional X-ray examination formations.
Radiological methods also include contrast angiopulmonography with the introduction of iodine-containing substances (urotrast, verografin), which helps identify the characteristics of the vessels of the pulmonary circulation, as well as the arteries of the bronchial tree.
Of certain diagnostic value are the data obtained using radionuclide methods: introduction of radioactive isotopes and subsequent assessment of their distribution in the chest organs using special devices (scanners, gamma cameras, etc.). In pulmonology practice, radioactive isotopes of technetium ( 99 Tc), in particular technetium-labeled albumin, gallium ( 67 Ga), xenon ( 133 Xe), indium ( 133 In), phosphorus ( 32 P) are usually used. Radionuclide methods allow to assess perfusion properties (technetium), regional ventilation (xenon), proliferative cellular activity of the interstitium, lymph nodes (gallium). For example, this study reliably reveals perfusion disorders in pulmonary embolism, accumulation of gallium isotope in the mediastinal lymph nodes in active sarcoidosis.
Endoscopic research methods
A special place in the examination of a patient with a lung disease belongs to endoscopic methods, among which bronchoscopy is of primary importance. Using a modern bronchofibroscope, it is possible to visually assess the characteristics of the respiratory tract from the glottis to the subsegmental bronchi, the function of the mucociliary escalator, take the contents of the respiratory tubes at different levels for cytological and bacteriological examination, conduct bronchoalveolar lavage with subsequent study of the obtained wash, make a puncture biopsy of the bronchial mucosa, as well as a transbronchial biopsy of adjacent tissues (lymph node, lung). The bronchoscope is also used for therapeutic purposes, sometimes for washing the bronchi and local administration of antibacterial agents in bronchiectatic disease (bronchial sanitation), but especially for liquefying and suctioning mucus from the lumen of blocked bronchi during an uncontrollable attack of bronchial asthma, especially in the presence of a picture of "silent lung", removal of a foreign body.
 [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ]
[ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ]
Indications for bronchoscopy
Indications |
Notes |
Hemoptysis. |
To establish the source (preferably in the period close to the end of bleeding) and to stop the bleeding. |
Chronic cough with no apparent cause. |
There may be an endobronchial tumor that is not visible on the radiograph. |
Delayed resolution of pneumonia. |
To exclude local bronchial obstruction. |
Atelectasis. |
To establish the cause. |
Lung cancer. |
For biopsy, assessment of operability. |
Lung abscess. |
To exclude bronchial obstruction, obtain material for bacteriological examination and to improve drainage. |
Foreign body. |
To delete. |
Bronchoscopy is mandatory in patients with hemoptysis (especially repeated) or pulmonary hemorrhage; it allows one to determine the source (trachea, bronchi, parenchyma) and cause (bronchiectasis, tumor, tuberculosis) of bleeding.
Among other endoscopic methods, although rarely used, are thoracoscopy (examination of the pleural layers) and mediastinoscopy (examination of the anterior mediastinum), one of the main purposes of which is biopsy of the corresponding areas.
Ultrasound examination (ultrasound)
In pulmonology, ultrasound is not yet very informative; it can be used to identify small areas of exudate and perform pleural puncture.
Intradermal tests
In the diagnosis of some pulmonary diseases, intradermal tests are used, which help to establish the presence of atopy (for example, allergic rhinitis, some types of bronchial asthma), the cause of pulmonary eosinophilia;the tuberculin test (especially in pediatric and adolescent practice), the Kveim test (in the diagnosis of sarcoidosis) are of diagnostic value.
Study of external respiratory function
Evaluation of the functional state of the respiratory organs is the most important stage of the patient examination. The functions of the lungs are very diverse: gas exchange, regulation of the acid-base balance, heat exchange, water exchange, synthesis of biologically active products, but one of the main functions of the respiratory organs is the function of gas exchange, which includes the flow of air into the alveoli (ventilation), gas exchange in the alveoli (diffusion), and oxygen transport by the blood of the pulmonary capillaries (perfusion). Therefore, a special place in the study of the respiratory organs is occupied by the study of the function of the external respiration apparatus. The normal functioning of this system ensures gas exchange between the external and internal environments, and therefore determines the completeness of tissue respiration, which is why it is important to understand the role of all components of the external respiration mechanism. The clinician must establish the functional capacity of this system, i.e., identify the degree of respiratory failure.
The most important method for determining the function of external respiration, primarily the ventilation function, is spirography. The main spirographic indicators (lung volumes) are divided into static and dynamic. The first group includes volumetric parameters. First of all, this is the vital capacity of the lungs (VC), i.e. the volume of air during maximum exhalation produced after maximum inhalation. Of the dynamic indicators, the forced vital capacity of the lungs (FVC) is of particular importance - the volume of air during the most intense and rapid exhalation, which is 80-85% of the VC in the first second of exhalation (FEV1) (Tiffeneau test). The FVC is affected by the state of bronchial patency: the smaller the lumen of the bronchi, the more difficult the exhalation, the smaller the volume of forced exhalation.
Another dynamic indicator is the volumetric speed of forced inhalation and exhalation (normally 5-7 l/s) and during calm breathing (normally 300-500 ml/s) - it is determined by a special device, a pneumotachometer, and reflects the state of bronchial patency: a decrease in the exhalation speed is a sign of bronchial obstruction.
The respiratory rate parameters are represented graphically by plotting the flow-volume curves, on which each point corresponds to a certain percentage of the FVC: the air flow rate (in liters per 1 s) is plotted along the ordinate axis, the forced expiratory volume (in percent or liters) is plotted along the abscissa axis, and the peak and instantaneous volumetric flow rates (MVF) are determined at the moment of forced expiration. In case of bronchial obstruction, the curve is shifted to the left and has a flat terminal part, in case of lung restriction, it is shifted to the right and does not differ in shape from the norm.
The diffusion capacity of the lungs can be determined using carbon monoxide (CO) flowing through the membrane (like O2): when CO is inhaled, the diffusion rate is calculated, which decreases (sometimes significantly) in severe lesions of the alveolar membrane and the interstitium of the lungs.
When assessing respiratory function, determination of the partial pressure of oxygen and carbon dioxide, as well as the pH of arterial blood, are of great clinical importance.
The state of the capillary bed (perfusion or oxygen transport by the blood) is assessed by inhaling pure oxygen: an insufficient increase in PO2 in arterial blood after inhalation indicates poor perfusion capacity of the lungs.
Who to contact?

