Medical expert of the article
New publications
Lung percussion
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Percussion is a tapping on areas of the body surface that reveals the physical characteristics of the underlying organs, tissues, and various formations: hollow (air), liquid (compacted), and combined. In this regard, the chest, where organs with different physical properties are located, is an important object for research. As already noted, percussion became widespread after the famous J. Corvisart translated into French at the beginning of the 19th century a treatise by the Viennese physician L. Auenbrugger (1722-1809), in which the latter described a method similar to tapping wine barrels, used by his father, a winemaker, to determine the level of wine in them. Percussion occupies a special place in the examination of the respiratory organs.
Different densities of air, low-air and airless tissue correspond to different shades of percussion sound, which reflects the state of the respiratory organs adjacent to the chest wall. The volume, pitch and duration of the sound obtained during chest percussion ultimately depend on the density and elasticity of the percussed area. Air and dense elements (muscles, bones, parenchyma of internal organs, blood) have the greatest influence on the quality of sound. The more the density and elasticity of the environment through which the vibrations pass differ, the more heterogeneous the percussion sound will be, the more it will differ from the ringing, so-called tympanic sound, reminiscent of the sound obtained when striking a drum (tympanum - drum), and arising from percussion of air-containing hollow formations (tapping the intestinal area). The less air content in the percussion area and the more dense elements, the quieter, shorter, duller the sound will be (dullness of percussion sound, absolutely dull - “hepatic”, “femoral” sound).
Types and rules of lung percussion
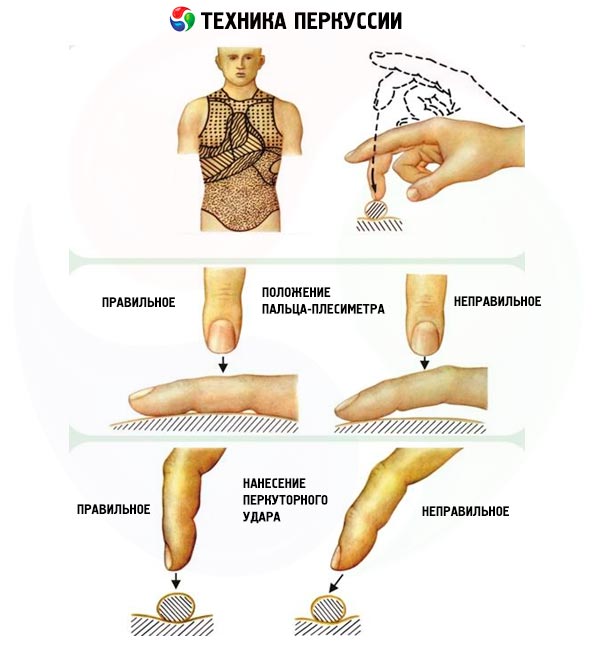
Different shades of percussion sound can be obtained using various techniques: tapping with a special hammer (most doctors use a finger as such a hammer) directly on the body of the person being examined (direct percussion) and tapping on the body of the person being examined through an additional conductor (pleximeter), which is used as various plates or, more often, a finger of the other hand, tightly applied to the surface of the body (indirect percussion). The overwhelming majority of doctors use indirect percussion "finger on finger".
When percussing, it should be remembered that the blow should be directed strictly perpendicular to the surface of the pleximeter, be light, short (fast), similar to the elastic blow of a tennis ball, which is achieved by moving only the hand at the wrist joint with the forearm in a motionless position.
Percussion is performed in order to identify changes in the physical properties (the ratio of air and dense elements) of an organ or its part (comparative percussion) or to determine the boundaries of the organ and the zone of altered physical properties (topographic percussion).
Comparative percussion
During comparative percussion of the chest, which is carried out along the intercostal spaces and is loud, the character of the sound obtained over symmetrical areas of the lungs is determined first, naturally excluding in such a comparison the anterior-lower part of the left half of the chest - the projection site of the heart area, deprived of air. Some asymmetry of sound data is detected during percussion of the area of both apices of the lungs (supraclavicular and subclavian spaces): due to the more developed muscles of the right half of the chest and the greater narrowness of the right upper lobe bronchus, the percussion sound over the right apex is usually more dull. It should be noted that percussion of the apices of the lungs used to be of particular importance due to the high prevalence of pulmonary tuberculosis (this localization is typical for the infiltrative form of tuberculosis). Comparative percussion allows us to reveal a special percussion sound over the lungs - clear pulmonary. This is the result of the transformations that the tympanic tone undergoes (due to air vibrations inside the elastic alveoli) when passing through the heterogeneous interstitial tissue of the lungs, the chest wall. But more important is the detection of changes in this sound over individual areas of the chest: dull (from dullness to absolute dullness) or tympanic.

The dullness (shortening) of the percussion sound is greater, the more dense elements there are, the more airiness is lost (fluid, infiltration, tumor tissue) in the percussion zone, which can reveal this area at different depths using different impact force: the stronger the impact (loud deep percussion), the deeper the area of compaction is detected. Dullness of the sound indicates the presence of fluid in the pleural cavities, a large amount of which causes a dull percussion sound (exudate, pus, transudate, blood). In this case, at least 500 ml of fluid should usually accumulate, but with the help of soft (weak) percussion, fluid can also be detected in the pleural sinuses. Features of the upper border of the dullness zone allow us to distinguish the nature of the pleural fluid. In the presence of inflammation (exudate), the upper border of dullness has the form of a curved line with a peak along the axillary lines, which is characteristic of an uneven rise in the fluid level (Damoiseau-Sokolov line), associated with different compliance of the underlying lung tissue to fluid pressure. Transudate is characterized by a level of the dullness zone closer to the horizontal.
Dullness of the pulmonary percussion sound is characteristic of the initial stages of the infiltrative process in the lungs ( pneumonia ), other compactions of the lung tissue (pronounced atelectasis, especially obstructive, pulmonary infarction, lung tumor, thickening of the pleural sheets).
With a decrease or thinning of the dense elements of the pulmonary structures, the tympanic tone of the percussion sound increases, which acquires a “box” or “pillow” character in pulmonary emphysema (loss of elasticity of the alveoli, but preservation of the integrity of most of the alveolar septa, which prevents the appearance of true tympanitis); the sound becomes pronounced tympanic over the cavity of the lung (cavern, emptied abscess, large bronchiectasis, pneumothorax, large emphysematous bullae).
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ]
Topographic percussion of the lungs
Topographic percussion of the lungs reveals the boundaries of a particular organ or detected pathological formation, using quiet percussion along the ribs and intercostal spaces, and the pleximeter finger is positioned parallel to the percussed boundary (for example, horizontally when determining the lower boundary of the lung). The position of the boundary being determined is fixed using identification landmarks. For the organs of the chest, these are the clavicles, ribs, intercostal spaces, vertebrae and vertical lines (anterior median, right and left sternal, parasternal, midclavicular, anterior, middle, posterior axillary, scapular, posterior median line). The ribs are counted from the front, starting with the second rib (the place of its attachment to the sternum is between the manubrium of the sternum and its body), the first rib corresponds to the clavicle. At the back, the ribs are counted based on the spinous processes of the vertebrae (it is easy to identify the spinous process of the 7th cervical vertebra: it protrudes most when the head is tilted forward) and the lower angle of the scapula, which corresponds to the 7th rib.
The lower edge of the lung on the right and left is located at the same level (naturally, on the left it is determined starting from the anterior axillary line due to the presence of the cardiac notch and the spleen area), respectively, along the right parasternal line - the upper edge of the 6th rib, the right midclavicular - the sixth intercostal space, both anterior axillary - the 7th rib, the middle axillary lines - the 8th rib, the posterior axillary - the 9th rib, the scapular lines - the 10th rib, the posterior median - the 11th thoracic vertebra.
The displacement of the lower border of the lungs downwards is detected primarily in pulmonary emphysema, less often - during an attack of bronchial asthma. In the first case, such a displacement is permanent, tends to increase due to the progression of hyperairiness of the lungs, in the second case it is observed even without emphysema as a result of acute expansion of the lungs due to the difficulty in exhalation characteristic of bronchial asthma. The presence of fluid and gas in the pleural cavity leads to the displacement of the lower edge of the lungs upwards, which is also observed with a high position of the diaphragm (pronounced obesity, pregnancy, large ascites, flatulence), which is usually accompanied by a decrease in the volume of the chest and filling of the lungs with air (a decrease in the vital capacity of the lungs), and this leads to respiratory failure and hemodynamic disturbances in the pulmonary circulation.
The indicated displacements of the lower border of the lungs are usually accompanied by a decrease in the mobility (excursion) of the lower pulmonary edge, which is determined by the midaxillary line: normally, in relation to the VIII rib, the pulmonary edge descends by 4 cm during a deep breath and rises by 4 cm during a maximum exhalation, and thus, the respiratory excursion of the lower pulmonary edge along this line is 8 cm. If it is difficult to take and hold a breath, this indicator is determined by successively using several regular breaths and noting the percussion position of the lower pulmonary edge each time.
Determining the border of the pulmonary margin and the degree of its displacement during breathing is an important technique for the early detection of pulmonary emphysema, which is certainly especially valuable during dynamic monitoring of the patient.
To clarify certain changes in the corresponding lobes of the lungs, it is important to know their topography. On the right, the upper and middle lobes are projected onto the anterior surface (the border between them begins at the level of attachment of the 4th rib to the sternum, then it goes obliquely to the 6th rib along the midclavicular line, where it reaches the border of the lower lobe), on the right side - the middle and lower lobes, on the left the anterior surface is occupied by the upper lobe, on the left side - the upper and lower (the border between them, as on the right, begins from the 6th rib along the midclavicular line, but then goes obliquely upward back to the scapula), a small part of the upper lobes is projected from both sides at the top at the back, the main surface of both halves of the chest is made up of the lower lobes.
Height of the tops
On the right |
Left |
|
| In front | 3 cm above the collarbone level |
3.5 cm above the collarbone |
| Behind | At the level of the spinous process of the 7th cervical vertebra |
0.5 cm above the level of the spinous process of the VII cervical vertebra |
Krenig margin width: right - 5 cm, left - 5.5 cm
Lower borders of the lungs
Typographic lines |
On the right |
Left |
| Parasternal | Fifth intercostal space |
- |
| Midclavicular | VI rib |
- |
| Anterior axillary | VII rib |
VII rib |
| Middle axillary | VIII rib |
VIII rib |
| Posterior axillary | IX rib |
IX rib |
| Scapular | X rib |
X rib |
| Paravertebral | Spinous process of the XI thoracic vertebra |
Spinous process of the XI thoracic vertebra |
Mobility of the lower edges of the lungs, cm
On the right |
Left |
|||||
Topographic line |
On inhalation |
On the exhale |
In total |
On inhalation |
On the exhale |
In total |
Midclavicular |
2 |
2 |
4 |
- |
- |
- |
Middle axillary |
3 |
3 |
6 |
3 |
3 |
B |
Scapular |
2 |
2 |
4 |
2 |
2 |
4 |

