Medical expert of the article
New publications
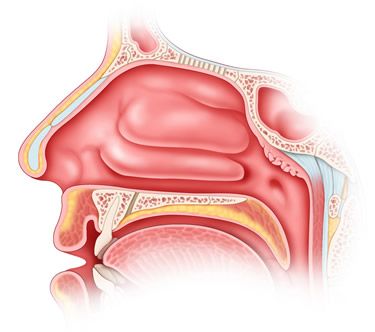
Vasomotor rhinitis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Vasomotor rhinitis comes from the name of the autonomic nerve fibers that innervate the smooth muscles of the arteries and veins. Vasomotor rhinitis is divided into vasoconstrictor (sympathetic) and vasodilator (parasympathetic) nerve fibers.
V. I. Voyachek defined vasomotor rhinitis as false rhinitis. In his famous textbook "Fundamentals of Otorhinolaryngology" he wrote that the name "false rhinitis" indicates that the symptom complex of a runny nose may not be accompanied by pathological signs of inflammation of the nasal mucosa. For the most part, this is a symptom of general vegetative neurosis and therefore is often only a link in a series of corresponding disorders, such as asthma. Thus, in its pure form, vasomotor rhinitis is functional. A subspecies of this group are allergic conditions, when vasomotor and secretory disorders from the nasal cavity occur under the influence of some allergen.
This definition, expressed more than half a century ago, remains relevant today, when the problem of chronic vasomotor (neurovegetative) and allergic rhinitis has been studied from many aspects of medical and biological science (immunology, allergology, neurovegetative neuroses, etc.). According to a number of authors, it is the latter that play the most important role in the pathogenesis of true vasomotor rhinitis, which is not accompanied in its classical manifestation by any inflammatory reactions.
It is important, however, to emphasize that it is the nasal vegetative-vascular dysfunctions provoked by endo- or exoallergens that can be complicated by inflammatory processes; in these cases, it is the primary allergy that is the main etiologic factor in the development of vasomotor rhinitis. In this regard, it should be recognized that the modern division of vasomotor rhinitis into neurovegetative and allergic forms is largely arbitrary and is mainly didactic in nature. Apparently, these are two sides of one pathological condition.
In its "pure form", the neurovegetative form of vasomotor rhinitis can be observed with any irritative processes in the nasal cavity, for example, caused by a contact thorn of the nasal septum, irritating the perivascular nerve vegetative endings of the lower nasal ridges. However, this mechanism can subsequently provoke the transition of the neurovegetative form to an allergic one. It is also possible that the nasal manifestations of the neurovegetative form of vasomotor rhinitis are a consequence of general vegetative neurosis; in this case, we can also observe other manifestations of this neurosis, for example, signs of neurocirculatory dystonia, hypotension, angina pectoris, etc.
In the genesis of the neurovegetative form of vasomotor rhinitis, pathological conditions of the cervical spine, manifested by alteration of the cervical sympathetic nodes, can play a major role. Thus, in the etiology and pathogenesis of vasomotor rhinitis, a whole complex of systemic pathological conditions can be traced, in which a runny nose is only the "tip of the iceberg" of a deeper and more widespread disease. An important role in the occurrence of vasomotor rhinitis can be played by provoking factors, which include occupational hazards, smoking, alcoholism, drug addiction. On the other hand, primarily occurring vasomotor and allergic rhinitis can play the role of specific triggers (trigger mechanisms), giving rise to more widespread and serious neurovascular diseases, such as migraine, perivascular neuralgia, diencephalic syndrome, etc.
Causes and pathogenesis of vasomotor rhinitis
Causes and pathogenesis of vasomotor rhinitis: the allergic form of vasomotor rhinitis is divided into seasonal (periodic) and constant (year-round) rhinitis.
Seasonal rhinitis is one of the syndromes of pollinosis (pollen allergy, pollen fever), characterized mainly by inflammatory lesions of the mucous membrane of the respiratory tract and eyes. In case of hereditary predisposition to pollinosis, plant pollen causes sensitization of the body, i.e. production of antibodies to the pollen allergen, as a result of which, when the latter gets on the mucous membrane, a reaction of interaction of the antigen with the antibody develops in it, manifested by signs of inflammation. Pathognomonic manifestations of seasonal rhinitis are seasonal attacks of acute rhinitis and conjunctivitis. In severe cases, bronchial asthma joins them. Pollen intoxication is also possible: increased fatigue, irritability, insomnia, sometimes an increase in body temperature. In the presence of chronic foci of infection, they can contribute to the development of acute sinusitis during pollinosis. Rare manifestations include diseases of the nervous system (arachnoiditis, encephalitis, damage to the optic and auditory nerves, development of attacks of Meniere's disease).
Symptoms. As a rule, an attack of rhinopathy occurs acutely, in the midst of complete health, at the end of May and in June, during the flowering period of trees and grasses, characterized by the appearance of severe itching in the nose, uncontrollable multiple sneezing, profuse watery discharge from the nose, difficulty in nasal breathing. At the same time, signs of conjunctivitis are also observed. An attack of seasonal rhinitis usually lasts 2-3 hours and can be repeated several times a day. The most common external factors can provoke vasomotor rhinitis here: exposure to the sun or a draft, local or general cooling, etc. It is noted that a state of psychological stress reduces the severity or interrupts an attack of hay fever.
During anterior rhinoscopy in the interictal period, no pathological changes in the nasal mucosa are detected, however, deformations of the nasal septum, contact spines, and in some cases, isolated mucous polyps may be present. During a crisis, the mucous membrane becomes sharply hyperemic or cyanotic, edematous, the nasal turbinates are enlarged and completely obstruct the nasal passages, in which abundant mucous discharge is observed. The vessels of the nasal turbinates react sharply by contracting to lubrication with adrenaline. In some patients, attacks of seasonal rhinitis may be accompanied by symptoms of irritation of the mucous membrane of the larynx and trachea (cough, hoarseness, secretion of viscous transparent sputum), as well as asthmatic syndrome.
Constant allergic rhinitis is one of the syndromes of the allergic condition of the body, manifested by various forms of allergy. In symptoms and clinical course it is similar to hay fever. The main distinguishing feature of constant allergic rhinitis is the absence of periodicity, more or less constant course, moderate severity of attacks. Allergens in this form of allergic rhinitis, unlike seasonal rhinitis, can be a variety of substances with antigenic and haptenic properties, constantly affecting a person and causing sensitization of the body with the formation of antibodies. These substances, when in contact with tissue antibodies, cause the same "antigen - antibody" reaction as in seasonal rhinitis, during which biologically active mediators are released (including histamine and histamine-like substances), irritating the receptors of the nasal mucosa, causing dilation of blood vessels and activating the activity of the mucous glands.
Symptoms of vasomotor rhinitis
Symptoms of vasomotor rhinitis are characterized by periodic or constant nasal congestion, often intermittent in nature, periodically occurring watery nasal discharge, at the height of the attack - itching in the nose, sneezing, a feeling of pressure in the depths of the nose, headache. During the day, an attack (V.I. Voyachek called this attack an "explosion" of the vasomotor reaction) of sneezing and rhinorrhea, as a rule, occurs suddenly and passes just as suddenly, can be repeated up to ten times a day or more often. At night, nasal congestion becomes constant due to the night cycle of increased function of the parasympathetic nervous system.
Typical is the stuffiness of the side of the nose on which the patient lies, and its gradual disappearance on the opposite side. This phenomenon indicates the weakness of vasoconstrictors. According to V.F. Undritz, K.A. Drennova (1956) and others, a long course of the functional stage of the neurovegetative form of vasomotor rhinitis leads to the development of the organic stage (proliferation of interstitial tissue and the occurrence of hypertrophic rhinitis), which is largely facilitated by the excessive use of decongestants. Vasoconstrictor fibers are related to adrenergic nerves, since when excitation is transmitted to the vessels, norepinephrine is released in the synapses. These fibers for the ENT organs originate from the superior cervical sympathetic ganglion. Parasympathetic vasodilator fibers are concentrated in the glossopharyngeal, facial, trigeminal nerves and the pterygopalatine ganglion.
During anterior rhinoscopy, enlarged inferior turbinates are determined, having a characteristic coloration, which V.I. Voyachek defined as "gray and white spots". The inferior turbinates are soft to the touch with a button probe, the probe easily goes deeper into the turbinate without damaging the mucous membrane. A pathognomonic sign is a sharp contraction of the turbinates when they are lubricated with adrenaline. The sense of smell is impaired depending on the degree of difficulty in nasal breathing.
Allergic form of vasomotor rhinitis
Allergic diseases have been known since ancient times. Hippocrates (5th-4th centuries BC) described cases of intolerance to certain food substances; K. Galen (2nd century AD) reported on a runny nose caused by the smell of roses; in the 19th century, hay fever was described and proven to be caused by inhaling plant pollen. The term "allergy" was proposed by the Austrian pediatrician C. Pirquet in 1906 to denote an unusual, altered reaction of some children to the administration of anti-diphtheria serum for treatment. Substances causing atypical (allergic) reactions were called allergens. Such substances include, for example, plant pollen, which causes seasonal diseases called hay fever. Allergens are divided into exogenous (chemical substances, food products, various plants, protein compounds, microorganisms, etc.) and endogenous, which are products of the vital activity of the allergen-prone organism, arising as a result of metabolic disorders, the occurrence of certain diseases, microbial associations vegetating in the organism. Chronic foci of infection, serums and vaccines, numerous medications, household and epidermal allergens, etc. can also be a source of allergy. A special group of allergens are physical factors - heat, cold, mechanical action, which cause the production of special substances with an allergogenic property in the organism sensitive to them.
When an allergen enters the body, an allergic reaction develops, which, depending on its nature, can be specific or non-specific. A specific reaction goes through three stages - immunological, the stage of mediator formation and the pathophysiological stage, or clinical manifestations. Non-specific allergic reactions (pseudo-allergic, non-immunological) occur upon first contact with an allergen without previous sensitization. They are characterized by only the second and third stages of an allergic reaction. Allergic rhinitis can occur both as a specific and as a non-specific reaction and mainly refer to allergic reactions of the first type, which also include anaphylactic shock, urticaria, atopic bronchial asthma, hay fever, Quincke's edema, etc.
Neurovegetative form of vasomotor rhinitis
As a rule, this form of vasomotor rhinitis is not characterized by seasonality. Vasomotor rhinitis is equally common at all times of the year and depends mainly on either external provoking factors (dustiness of rooms, aggressive vapors in the inhaled air, the presence of contact curvatures of the nasal septum), or on the previously mentioned general neurovegetative dysfunction. Usually, in the latter case, patients are patients not only of a rhinologist, but also of a neurologist.
What's bothering you?
Diagnosis of vasomotor rhinitis
Diagnosis of vasomotor rhinitis: pathological changes and clinical course of persistent allergic rhinitis can be divided into four stages:
- stage of transient aperiodic attacks;
- continue type stage;
- stage of polyp formation;
- carnification stage.
The first stage is characterized by a more or less constant moderate runny nose with periodic crises. Patients with this form of rhinitis are highly sensitive to the cold factor, reacting to the slightest cooling of the hands, feet or the whole body, as well as to drafts, with an exacerbation of the pathological process. Patients complain of constant, periodically increasing nasal congestion, decreased or absent sense of smell, poor sleep, dry mouth, headaches, increased physical and mental fatigue, as well as periodic attacks of expiratory dyspnea. At this stage, initial signs of impaired permeability of cell membranes occur.
During anterior and posterior rhinoscopy at this stage of the disease, the same changes are observed as during an attack of seasonal rhinitis, and the activity of decongestants in relation to the vessels of the nasal cavity is maintained.
However, with a longer course of persistent allergic rhinitis, its second stage occurs, manifested in the initial signs of degeneration of the nasal mucosa. It becomes pale, acquires a grayish tint, is covered with granular formations, especially noticeable in the area of the anterior ends of the middle and lower nasal conchae and the posterior end of the lower nasal conchae. At this stage, difficulty in nasal breathing becomes more or less constant, the effect of vasoconstrictor drugs is reduced to a minimum, the sense of smell is practically absent, general complaints intensify.
After some time, calculated from several months to 1-4 years, mucous polyps appear in the middle nasal passage (the stage of polyp formation or polypous rhinitis) in the form of translucent saccular formations hanging on a stalk into the lumen of the common nasal passage. Most often, they look flattened, squeezed between the lateral wall of the nose and its septum. Old polyps are usually covered with a thin vascular network and grow into connective tissue.
At the same time, the stage of carnification begins: the tissues of the middle and especially the lower nasal concha become denser, stop responding to vasoconstrictors and acquire all the signs of hypertrophic rhinitis. The third and fourth stages are characterized by constant nasal congestion, mechanical and sensory anosmia, and an increase in general symptoms of the disease.
General symptoms of the disease (increased fatigue, insomnia, frequent colds, sensitivity to cold, etc.) become constant. At the stage of polyp formation, attacks of bronchial asthma intensify and become more frequent. The temporal relationship between bronchial asthma and the stage of polyp formation may vary. Often, the stage of polyp formation, i.e. allergic rhinitis syndrome, occurs as the primary lesion. If the allergy is based on non-infectious genesis, then we speak of atopic bronchial asthma. It should also be noted that similar pathomorphological processes in allergic rhinitis develop in the paranasal sinuses and most often in the maxillary sinuses, from which polyps prolapse through its anastomosis into the middle nasal passage.
Treatment of allergic rhinitis involves the use of antiallergic, desensitizing, antihistamine, vasoconstrictor, local anesthetic and general sedative agents. This list of medications is recommended by the international community of rhinologists in the form of the so-called consensus of 1996, however, despite these recommendations and numerous original proposals from various authors, the treatment of patients suffering from allergic rhinitis remains a difficult and not fully resolved task. The most effective method is to identify and eliminate the allergen causing vasomotor rhinitis, however, with polyallergy, this method also becomes ineffective, especially since this form of allergic rhinitis can proceed according to the type of so-called creeping allergy, when previously indifferent substances, under the influence of the sensitizing effect of allergens, themselves become such and cause corresponding, sometimes hyperergic reactions.
What do need to examine?
What tests are needed?
Who to contact?
Treatment of vasomotor rhinitis
Treatment of vasomotor rhinitis is mainly symptomatic, aimed at the use of sympathomimetic drugs that have a vasoconstrictor effect (sanorin, naphthyzin, ephedrine, etc.). New generation drugs include dosage forms whose active ingredients are substances with sympathomimetic properties, such as oxymetazoline (Nazivin, Nazol), tetrahydrozoline hydrochloride (Tizin), xylometazoline hydrochloride (xylometazoline, Xymelin), etc. All of the listed drops for rhinitis have an alpha-adrenergic effect, constrict peripheral vessels, reduce swelling of the nasal mucosa, hyperemia and exudation. They are indicated for acute neurovegetative and allergic rhinopathy, hay fever, sinusitis and their tubal and otitis complications. They are used in the form of drops and aerosols. Methods of administration and dosage are indicated in the corresponding annotations.
Symptomatic treatment of vasomotor rhinitis
Symptomatic treatment should also include various surgical interventions, such as mechanical and ultrasound-guided submucosal destruction of the vascular plexuses of the inferior turbinates for subsequent scarring, galvanocautery of the inferior turbinates, the use of cauterizing silver nitrate salts, etc.
Elements of pathogenetic treatment of vasomotor rhinitis include various physiotherapeutic methods, both local and remote, aimed at normalizing the interaction of the sympathetic and parasympathetic parts of the ANS, improving microcirculation, enzymatic activity, enhancing the oxidation of biosubstrates, normalizing the function of cell membranes, etc. For example, local methods include the use of low-energy laser radiation, constant magnetic fields, etc. According to the method of A.F. Mamedov (1991), a combined action of the specified factors is used, in which a constant magnetic field is directed from the outside to the slope of the nose, and from the inside, using a laser light guide, the reflexogenic zones of the anterior ends of the middle and inferior nasal conchae are irradiated. At a distance, laser irradiation of the projection zone of the pterygopalatine ganglion, various physiotherapeutic effects on the collar zone, etc. are used.
In the treatment of the neurovegetative form of vasomotor rhinitis, a targeted study of the general neurovegetative status is important to identify possible general neurological disorders and neurotic conditions. Living and working conditions, the presence of bad habits, chronic foci of infection and diseases of internal organs are assessed.
All methods of treatment for allergic rhinitis are divided into local and general, symptomatic and pathogenetic. If an allergen is found and a corresponding anti-antigen serum is produced, then we talk about etiotropic or immunological treatment. Currently, there is a huge number of different drugs used for allergies, and in particular for allergic rhinitis, detailed information about which is provided in the Register of Medicines.
Local treatment of vasomotor rhinitis
Local treatment is mainly symptomatic and only partly pathogenetic, aimed at blocking local allergic reactions, i.e. nasal syndrome of general allergy. Local preparations are used in the form of nasal sprays, less often in the form of drops or powders blown into the nasal cavity. As local preparations, preparations prepared on the basis of azelastine hydrochloride (allergodil), levocabastine, etc. are used.
Allergodil is available as a nasal spray and eye drops. Levocabastip is used as endo-nasal and eye drops. Both drugs have antiallergic and antihistamine properties, selectively block H1 receptors. After intranasal use, it quickly eliminates the symptoms of allergic rhinitis (itching in the nasal cavity, sneezing, rhinorrhea) and improves nasal breathing by reducing swelling of the nasal mucosa. When applied to the conjunctiva, it reduces the symptoms of allergic conjunctivitis (itching, lacrimation, hyperemia and swelling of the eyelids, xsmosis). In addition to antihistamines, in case of allergic rhinitis, local use of alpha-blockers (naphthyzin, sanorin, galazolin) is possible, as well as new drugs with a similar effect (Dr. Theiss nasal spray, nazivin, tizin, ximeyain, etc.).
Each drug used for allergic and any other diseases is characterized by such concepts as contraindications, use during pregnancy and breastfeeding, side effects, overdose, precautions, special instructions, compatibility with other drugs, etc., which are detailed in the relevant manuals, reference books and annotations. Before using any drug, this information is subject to careful study.
Allergodil spray: adults and children over 6 years old, one spray into each half of the nose 2 times a day. Eye drops for adults and children over 4 years old, one drop in the morning and evening until the symptoms of the disease disappear.
Levocabastine: intranasally for adults and children over 6 years of age - 2 inhalations in each nasal passage 2 times a day (maximum 4 times a day). Treatment continues until symptoms disappear.
Dr. Theiss nose spray: the spray is based on kenlometazoline, which has a vasoconstrictor and anticongestive effect. The drug is administered into both halves of the nose while inhaling using a special sprayer, one spray into each half of the nose 3-4 times a day for 2 days.
Nazivin (oximstazoline) is available as drops and spray. Nasal drops: adults and children over 6 years old, 1-2 drops in each half of the nose 2-3 times a day, 0.05% solution; children from 1 year to 6 years old - 0.025%, under 1 year - 0.01% solution. Nasal spray and dosed nasal spray 0.5%: adults and children over 6 years old - one spray 2-3 times a day for 3-5 days.
Tizin (tetrahydrozoline hydrochloride) is a sympathomimetic amine. Drops, aerosol, gel for intranasal use (0.05-0.1%). Adults and children over 6 years old - 2-4 drops in each nostril no more often than every 3 hours. It also has a sedative property, applicable in pediatrics.
Ximelin (kenlometazoline) stimulates alpha-adrenergic receptors, has a rapid and long-lasting vasoconstrictor and anticongestive effect. Adults and children over 6 years old - 2-3 drops of 1% solution or one spray from a sprayer into each half of the nose 4 times a day. Infants and children under 6 years old - 1-2 drops of 0.5% solution into each nostril 1-2 (no more than 3) times a day. Nasal gel only for adults and children over 7 years old - 3-4 times a day; put a small amount into each half of the nose as deep as possible on a cotton swab for several minutes so that the stick with cotton wool can be easily removed.
The local treatment of allergic rhinitis should be supplemented selectively with the medications listed in the section on the treatment of the neurovegetative form of vasomotor rhinitis.
Pathogenetic treatment of vasomotor rhinitis
General treatment should be recognized as pathogenetic, and in cases where immunological methods are used, as well as etiotropic. As A.S. Kiselev (2000) notes, specific immunotherapy is very effective, but its difficulties lie in the laboratory isolation of an active allergen (antigen), especially in polyallergy. In addition, the use of specific antiallergic serums can cause hyperergic reactions such as anaphylaxis and exacerbation of atopic asthma, so immunotherapy has not become widespread either in our country or abroad. The use of general (oral) treatment is based on the assumption that atopic rhinitis (seasonal, year-round) is a local manifestation of a general allergic disease, so the use of drugs with appropriate pharmacological properties that act on the body as a whole is an obligatory method of treating not only rhinogenic manifestations of allergy, but also its manifestations in other organs and systems. The most common method of using antiallergic drugs of general action is oral. All of them have almost identical pharmacological effects.
Among the antihistamines that were widely used in the last century and have not lost their relevance in our time, it is necessary to mention such as diphenhydramine, diazolin, suprastin, tavegil, the main pharmacodynamic action of which is the replacement of endogenous histamine (the source of allergic reactions) in the histamine receptors of blood vessels and blocking the pathogenic properties of histamine in these receptors. Currently, there are many new generation drugs that have a more effective effect and are devoid of side effects characteristic of drugs of the previous generation. New generation drugs selectively block H1-histamine receptors, prevent the effect of histamine on the smooth muscles of blood vessels, reduce capillary permeability, inhibit exudation and excretory function of glands, reduce itching, capillary stasis, erythema, prevent the development and alleviate the course of allergic diseases.
Oral preparations for the treatment of vasomotor rhinitis
Astemizole. Indications: allergic seasonal and year-round rhinitis, allergic conjunctivitis, allergic skin reactions, angioedema, bronchial asthma, etc. Method of administration and dosage: per os on an empty stomach once a day; adults and children over 12 years old - 10 mg, children aged 6-12 years - 5 mg as tablets or suspension, under 6 years - 2 mg per 10 kg of body weight only as a suspension. The maximum treatment period is 10 days.
Loratadine. Indications are the same as for astemizole; in addition, it is indicated for allergic reactions to insect bites and pseudo-allergic reactions to histamine liberators. Method of administration and dosage: per os before meals. Adults and children (over 12 years old or weighing more than 30 kg) - 10 mg (1 tablet or 1 teaspoon of syrup) 1 time per day.
Other drugs with similar effects: histalong, dimeboi, clarisens, clariaze, claritin, desloratadine, cystin, ebastine, astafen, ketotif, ketotifen, pseudoephedrine and many others.
Steroid drugs. General steroid therapy for allergic rhinitis is used extremely rarely, only in cases complicated by attacks of atopic bronchial asthma, and is the prerogative of a pulmonologist, and in case of anaphylactic shock - a resuscitator. However, local application of corticosteroids in combination with antihistamine therapy significantly increases the effectiveness of the treatment of allergic rhinitis, especially in its severe clinical forms. In the last century, various ointments and emulsions containing steroid components became widespread. Currently, more modern composite drugs are used that do not have the side effects inherent in steroids used in pure form. Such drugs include beconase (beclomethasone dipropionate), syntaris (flunisolide), flixonase (fluticasone pronionate), etc.
Beconase is a metered aerosol of a glucocorticoid drug for intranasal use. 1 dose contains 50 mcg of the active substance beclomethasone dipropionate. The drug has a pronounced anti-inflammatory and antiallergic property, eliminates edema, hyperemia. It is used to prevent and treat seasonal and year-round allergic rhinitis. It is used only intranasally, two inhalations in each nostril < 2 times a day. The maximum daily dose is 8 inhalations per day.
Sintaris is a metered-dose aerosol (active ingredient flusinolide) of a glucocorticoid drug for intranasal use, available in 20 ml (200 doses) glass bottles equipped with a metered-dose spray device. It has anti-edematous, anti-exudative, and anti-allergic effects. It is indicated for seasonal and year-round rhinitis, including hay fever. Adults are prescribed 2 sprays in each nostril 2 times a day. During an exacerbation or in severe cases of the disease - 2 sprays in both halves of the nose 3 times a day. Children are prescribed one spray (25 mcg) once a day. Maximum dose: adults - 6, children - 3 sprays a day.
Similar nasal sprays (flixonase and flixotide) based on fluticasone give the same therapeutic effect as those named; they have minimal systemic action.
Currently, composite drugs containing substances with antihistamine and alpha-adrenomimetic action, such as clarinase and rinopront, are becoming widespread.
Clarinase-12 (composition - tablets containing 5 mg of loratadine and 120 mg of pseudoephedrine). They have antiallergic and vasoconstrictive properties; block H1 receptors, have decongestant properties (pseudoephedrine sulfate), reduce swelling of the mucous membrane of the upper respiratory tract, improve their patency and facilitate breathing. They are used per os, regardless of food intake, without chewing, with a glass of water. Adults and children aged 12 years and older - 1 tablet 1-2 times a day.
Rhinopront. Active ingredients - carbinoxamine maleate and phenylephrine hydrochloride, which have antihistamine and antiallergic effects. Carbinoxamine reduces the permeability of the capillaries of the nasal mucosa, phenylephrine has a sympathomimetic effect, causes vasoconstriction and reduces swelling of the mucous membrane. Within 10-12 hours, it eliminates the symptoms of acute rhinitis, burning and itching in the eyes, a feeling of heaviness in the head. This dosage form is used for acute rhinitis of various origins (vasomotor, allergic, infectious and inflammatory, hay fever).
Adults and children over 12 years old are prescribed 1 capsule 2 times a day at 12-hour intervals. In case of difficulty swallowing, 1 tablespoon of syrup is prescribed 2 times a day. Children from 1 year to 6 years old - 1 teaspoon of syrup 2 times a day, from 6 to 12 years old - 2 teaspoons 2 times a day.
Local steroid therapy is effective in combination with antihistamines and alpha-adrenoblockers. As a rule, corticosteroids used for local application are included in composite dosage forms manufactured according to special recipes or are used in monoform.
Among the latest generation of drugs, it is worth noting Rhinocort, the active ingredient of which is the semi-synthetic corticosteroid budesonide.
Rinocort is a glucocorticoid drug for inhalation use; it is available in an aerosol. It has a local anti-inflammatory effect, practically without causing a systemic effect. It is indicated for seasonal and year-round allergic rhinitis, as well as for the prevention of hay fever and relapse of polyps after polypotomy. The initial dose is 2 sprays (100 mcg) in each nostril in the morning and evening. When the therapeutic effect is achieved, the dose can be reduced.
More information of the treatment
Drugs


 [
[