Medical expert of the article
New publications
Chronic Bronchitis - Information Overview
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Chronic bronchitis is classically described as chronic cough and sputum production for at least 3 months of the year for 2 consecutive years.
Chronic bronchitis was originally defined by Dr. Charles Badham in 1814 as “a cough… which persists for many weeks or months… such patients always have difficulty in breathing, often with a feeling of heaviness or fluttering… the expectoration is usually profuse, tenacious, and persistent.” Much later, chronic bronchitis was defined as chronic cough and expectoration for at least 3 months of the year for 2 consecutive years. This definition has been used for decades and remains the gold standard. However, several other definitions have been used in clinical studies. For example, chronic bronchitis is defined as chronic hypersecretion of mucus. 5 Other definitions include bronchial hypersecretion, chronic cough with expectoration, chronic sputum, and chronic productive cough.
Epidemiology
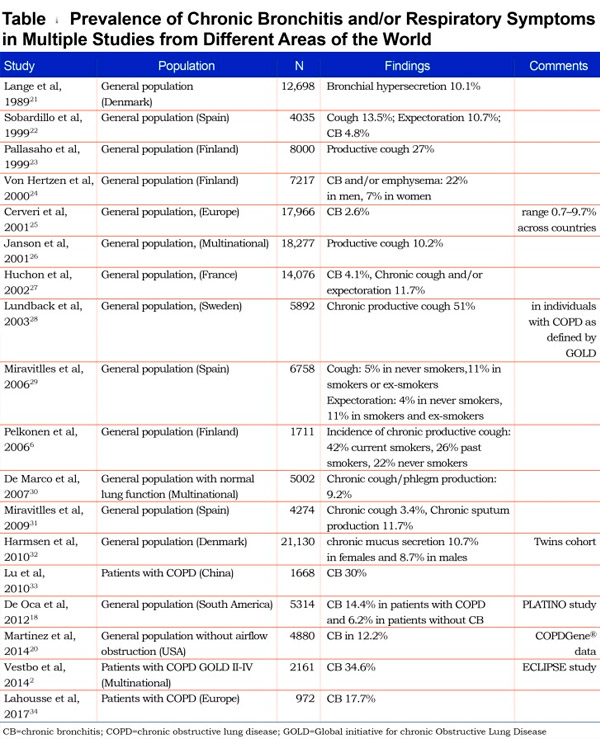
The prevalence of chronic bronchitis varies worldwide, from 3.4–22.0% in the general population to 74.1% in patients with COPD. [ 9 ] The table describes the prevalence of chronic bronchitis and/or respiratory symptoms in multiple studies conducted in different regions of the world.
Causes chronic bronchitis
There are many risk factors for developing chronic bronchitis (CB) and COPD, but cigarette smoking is the most important risk factor. A Finnish study of 1,711 men over 40 years found that the cumulative incidence of chronic bronchitis was 42% in current smokers and 26% in former smokers.[ 10 ]
However, a significant proportion of chronic bronchitis is not related to cigarette smoking, particularly in young people, women, and people in developing countries. In the above-mentioned Finnish study, the pooled incidence of chronic bronchitis among non-smokers was 22%. An analysis of two separate cross-sectional studies in 1998/2000 and 2007/2010 showed similar prevalence of chronic bronchitis, but an increase in the number of never smokers (from 7.6% to 9.1%), an overall decrease in the number of current smokers (from 33.6% to 26.9%), and an increase in the incidence of allergic rhinitis (from 19.5% to 24.5%). 40
Specific occupational exposure studies (coal and hard rock miners, tunnel workers, concrete manufacturers and non-mining workers).
A meta-analysis by Mamane et al. found that exposure to agricultural pesticides was associated with respiratory symptoms, impaired respiratory function and an increased prevalence of chronic bronchitis.[ 11 ] Air pollution may also be a risk factor; a comprehensive study by the Committee on the Medical Effects of Air Pollutants (COMEAP) in the United Kingdom found a possible association between the incidence and prevalence of chronic bronchitis and long-term exposure to air pollution.[ 12 ] A systematic review found an association between solid fuel use and COPD and chronic bronchitis, particularly with wood smoke compared with other biomass fuels. [ 13 ] Additionally, marijuana smoking has been linked to chronic bronchitis, [ 14 ] and there is emerging evidence that e-cigarettes may be linked to CB.
Read also: What causes chronic bronchitis?
Pathogenesis
Hypertrophy and hyperfunction of the bronchial glands, increased mucus secretion, relative decrease in serous secretion, change in the composition of the secretion - a significant increase in acidic mucopolysaccharides in it, which increases the viscosity of sputum are revealed. Under these conditions, the ciliated epithelium does not ensure the cleansing of the bronchial tree and the normal renewal of the entire layer of secretion; emptying of the bronchi in this state of mucociliary clearance occurs only when coughing. Such conditions are detrimental to the mucociliary apparatus: dystrophy and atrophy of the ciliated epithelium occur. At the same time, the glandular apparatus, which produces lysozyme and other antibacterial protectors, is subject to the same degeneration. Under these conditions, bronchogenic infection develops, the activity and relapses of which largely depend on the local immunity of the bronchi and the development of secondary immune deficiency.
Spasm, edema, fibrous changes in the bronchial wall with stenosis of its lumen or its obliteration are of great importance in the pathogenesis of the disease. Obstruction of small bronchi leads to overstretching of the alveoli during exhalation and disruption of the elastic structures of the alveolar walls, as well as to the appearance of hyperventilated and completely non-ventilated zones that function as an arteriovenous shunt. Since the blood passing through these alveoli is not enriched with oxygen, arterial hypoxemia develops. In response to alveolar hypoxia, spasm of the pulmonary arterioles occurs with an increase in total pulmonary-arterial resistance; precapillary pulmonary hypertension occurs. Chronic hypoxemia leads to polycythemia and increased blood viscosity, accompanied by metabolic acidosis, which further increases vasoconstriction in the pulmonary circulation.
In large bronchi, superficial infiltration develops, in medium and small bronchi, as well as in bronchioles, this infiltration can be deep with the development of erosions, ulcerations and the formation of meso- and panbronchitis. The remission phase is characterized by a decrease in inflammation in general, a significant decrease in the amount of exudate, proliferation of connective tissue and epithelium, especially with ulceration of the mucous membrane. The final phase of the chronic inflammatory process in the bronchi is sclerosis of their walls, atrophy of glands, muscles, elastic fibers, cartilage. Irreversible stenosis of the bronchial lumen or its expansion with the formation of bronchiectasis is possible.
Read also: Chronic bronchitis - Pathogenesis
Symptoms chronic bronchitis
The onset of the disease is gradual. The first symptom is a morning cough with the separation of mucous sputum. Gradually, the cough begins to occur at night and during the day, intensifying, as with chronic bronchitis, when inhaling cold damp or hot dry air. The amount of sputum increases, it becomes mucopurulent and purulent. Dyspnea appears and progresses, first during physical exertion, and then at rest.
Read also: Chronic Bronchitis - Symptoms
Stages
In the clinical course of chronic bronchitis, four stages are distinguished: catarrhal, purulent, obstructive and purulent-obstructive. The third stage is characterized by emphysema and bronchial asthma, the fourth - by purulent complications (bronchiectasis).
Forms
Most pulmonologists suggest distinguishing between primary and secondary chronic bronchitis.
Primary chronic bronchitis is understood as chronic bronchitis as an independent disease, not associated with any other bronchopulmonary pathology or damage to other organs and systems. In primary chronic bronchitis, there is a diffuse lesion of the bronchial tree.
Secondary chronic bronchitis is etiologically associated with chronic inflammatory diseases of the nose, paranasal sinuses; with chronic limited inflammatory diseases of the lungs (chronic pneumonia, chronic abscess); with previous pulmonary tuberculosis; with severe heart diseases occurring with congestion in the pulmonary circulation; with chronic renal failure and other diseases. Usually secondary chronic bronchitis is local, less often - diffuse.
Chronic bronchitis is the most common disease of the bronchopulmonary system. In the USA, for example, only chronic obstructive bronchitis (COB), i.e. the most prognostically unfavorable form of chronic bronchitis, affects about 6% of men and 3% of women, in Great Britain - 4% of men and 2% of women. In people over 55 years of age, the prevalence of this disease is about 10%. The share of chronic bronchitis in the overall structure of diseases of the respiratory system of non-tuberculous origin currently reaches more than 30%.
Depending on the nature of the course, the severity of the pathological process in the bronchi and the characteristics of the clinical picture of the disease, two main forms of chronic bronchitis are distinguished:
- Chronic simple (non-obstructive) bronchitis (CNB) is a disease characterized by damage to predominantly the proximal (large and medium) bronchi and a relatively favorable clinical course and prognosis. The main clinical manifestation of chronic non-obstructive bronchitis is a constant or periodic cough with sputum production. Signs of mild bronchial obstruction occur only during periods of exacerbation or at the very latest stages of the disease.
- Chronic obstructive bronchitis (COB) is a disease characterized by deeper degenerative-inflammatory and sclerotic changes not only in the proximal but also in the distal airways. The clinical course of this form of chronic bronchitis is usually unfavorable and is characterized by a prolonged cough, gradually and steadily increasing dyspnea, and decreased tolerance to physical activity. Sometimes, with chronic obstructive bronchitis, signs of local bronchial damage are detected (bronchiectasis, cicatricial changes in the bronchial wall, pneumosclerosis).
The main distinguishing feature of chronic obstructive bronchitis is early damage to the respiratory parts of the lungs, manifested by signs of respiratory failure, slowly progressing in parallel with the increase in the degree of bronchial obstruction. It is believed that with chronic obstructive bronchitis, the annual decrease in VC is more than 50 ml per year, while with chronic non-obstructive bronchitis - less than 30 ml per year.
Thus, clinical assessment of patients with chronic bronchitis requires mandatory identification of two main forms of the disease. In addition, diagnosis of the phase of the disease (exacerbation, remission), the nature of inflammation of the bronchial mucosa (catarrhal, mucopurulent, purulent), the severity of the disease, the presence of complications (respiratory failure, compensated or decompensated chronic pulmonary heart disease, etc.) is important.
Below is the simplest and most accessible classification of chronic bronchitis.
Classification of chronic bronchitis
Form of chronic bronchitis:
- simple (non-obstructive);
- obstructive.
Clinical, laboratory and morphological characteristics:
- catarrhal;
- mucopurulent or purulent.
Disease phase:
- exacerbation;
- clinical remission.
Severity:
- mild - FEV1 greater than 70%;
- average - FEV1 within 50 to 69%;
- severe - FEV1 less than 50% of predicted value.
Complications of chronic bronchitis:
- pulmonary emphysema;
- respiratory failure (chronic, acute, acute on the background of chronic);
- bronchiectasis;
- secondary pulmonary arterial hypertension;
- pulmonary heart disease (compensated and decompensated).
The given classification takes into account the recommendations of the European Respiratory Society, in which the severity of chronic bronchitis is assessed by the magnitude of the decrease in FEV1 compared to the expected values. It is also necessary to distinguish between primary chronic bronchitis - an independent nosological form, and secondary bronchitis, as one of the manifestations (syndrome) of other diseases (for example, tuberculosis). In addition, when formulating a diagnosis of chronic bronchitis in the acute phase, it is advisable to indicate the possible causative agent of the bronchopulmonary infection, although this approach has not yet become widespread in wide clinical practice.
Read also: Chronic Bronchitis - Classification
Diagnostics chronic bronchitis
The diagnosis is established using fibrobronchoscopy, which visually evaluates the endobronchial manifestations of the inflammatory process (catarrhal, purulent, atrophic, hypertrophic, hemorrhagic, fibro-ulcerative endobronchitis) and its severity (but only up to the level of subsegmental bronchi). Bronchoscopy allows for a biopsy of the mucous membrane and histological methods to clarify the nature of its morphological changes, as well as to identify tracheobronchial hypotonic dyskinesia (increased mobility of the walls of the trachea and bronchi during breathing, up to expiratory collapse of the walls of the trachea and main bronchi - as in laryngomalacia, only with the opposite sign) and static retraction (change in configuration and decrease in the lumen of the trachea and bronchi), which can complicate chronic bronchitis and be one of the causes of bronchial obstruction. However, with chronic bronchitis, the main pathological changes occur in the smaller bronchi, so broncho- and radiography are used in the diagnosis of this disease.
Read also: Chronic Bronchitis - Diagnosis
What do need to examine?
What tests are needed?
Differential diagnosis
Chronic bronchitis is differentiated from bronchial asthma, tuberculosis and lung cancer. Chronic bronchitis differs from bronchial asthma primarily by the absence of asthma attacks, while obstructive bronchitis is characterized by constant cough and shortness of breath. There are also other laboratory methods for differential diagnosis of these diseases, such as sputum microscopy.
Who to contact?
Treatment chronic bronchitis
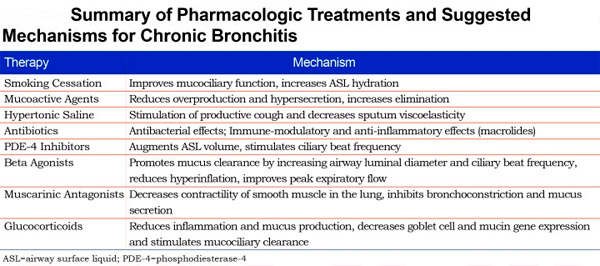
Pharmacological therapy of chronic bronchitis is aimed at achieving three main goals: relief of symptoms in stable disease (mucoactive agents, beta-adrenergic agonists, muscarinic receptor antagonists), reduction of loss of lung function (smoking cessation), prevention of exacerbations (mucoactive agents, macrolides, phosphodiesterase-4, PDE-4 inhibitors) and treatment of exacerbations (antibiotics, glucocorticoids) when they occur.
If purulent sputum, signs of intoxication, leukocytosis, and elevated ESR appear, chronic bronchitis should be treated with antimicrobial therapy (aminopenicillins in combination with beta-lactamase inhibitors, macrolides, fluoroquinolines, etc.) in courses sufficient to suppress the activity of the infection over a period of 7-14 days.
Read also: Chronic Bronchitis - Treatment


 [
[