Medical expert of the article
New publications
Bronchi
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The right main bronchus is a kind of continuation of the trachea. Its length is from 28 to 32 mm, the diameter of the lumen is 12-16 mm. The left main bronchus is 40-50 mm long and has a width of 10 to 13 mm.
Towards the periphery, the main bronchi are dichotomously divided into lobar, segmental, subsegmental and further down to the terminal and respiratory bronchioles. However, division into 3 branches (trifurcation) and more is also encountered.
The right main bronchus is divided into the upper lobe and intermediate, and the intermediate is divided into the middle lobe and lower lobe. The left main bronchus is divided into the upper lobe and lower lobe. The total number of generations of the respiratory tract is variable. Starting from the main bronchus and ending with the alveolar sacs, the maximum number of generations reaches 23 - 26.
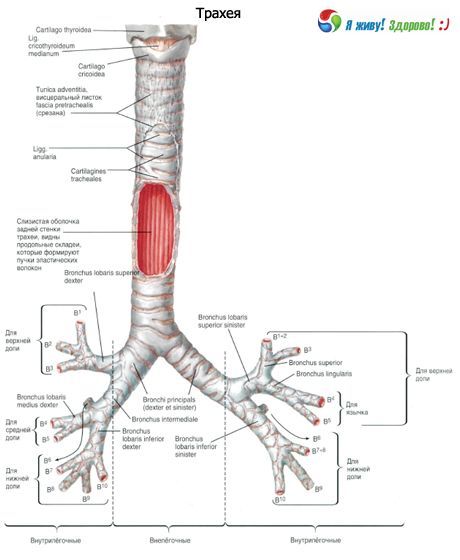
The main bronchi are the first order bronchi, the lobar bronchi are the second order, the segmental bronchi are the third order, etc.
Bronchi from the 4th to the 13th generation have a diameter of about 2 mm, the total number of such bronchi is 400. In the terminal bronchioles, the diameter fluctuates from 0.5 to 0.6 mm. The length of the airways from the larynx to the acini is 23-38 cm.

The right and left main bronchi (bronchi principles dexter et sinister) begin at the bifurcation of the trachea at the level of the upper edge of the 5th thoracic vertebra and go to the hilum of the right and left lungs, respectively. In the area of the hilum of the lungs, each main bronchus divides into lobar (second-order) bronchus. The aortic arch is located above the left main bronchus, and the azygos vein is located above the right. The right main bronchus has a more vertical position and is shorter (about 3 cm) than the left main bronchus (4-5 cm in length). The right main bronchus is wider (diameter 1.6 cm) than the left (1.3 cm). The walls of the main bronchi have the same structure as the walls of the trachea. From the inside, the walls of the main bronchi are lined with a mucous membrane, and from the outside they are covered with adventitia. The basis of the walls are cartilages that are not closed at the back. The right main bronchus contains 6-8 cartilaginous half rings, the left one - 9-12 cartilages.
Innervation of the trachea and main bronchi: branches of the right and left recurrent laryngeal nerves and sympathetic trunks.
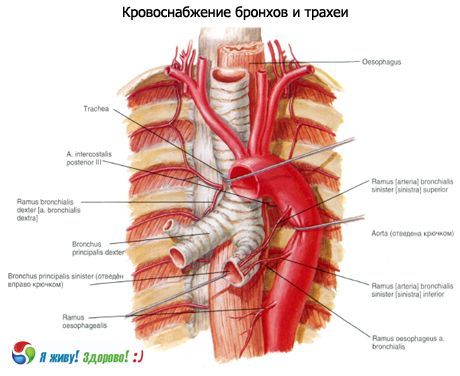
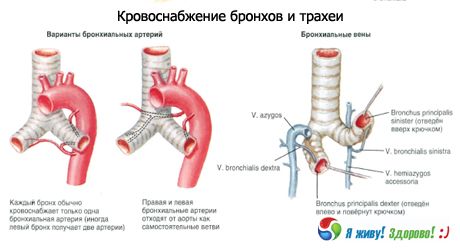
Blood supply: branches of the inferior thyroid artery, internal thoracic artery, thoracic aorta. Venous outflow is carried out into the brachiocephalic veins.
Lymph drainage: into the deep cervical lateral (internal jugular) lymph nodes, pre- and paratracheal, upper and lower tracheobronchial lymph nodes.
Histological structure of the bronchi
The trachea and large bronchi are covered externally by a loose connective tissue sheath, the adventitia. The outer shell (adventitia) consists of loose connective tissue containing fat cells in the large bronchi. Blood lymphatic vessels and nerves pass through it. The adventitia is not clearly demarcated from the peribronchial connective tissue and, together with the latter, provides the possibility of some displacement of the bronchi in relation to the surrounding parts of the lungs.
Further inward are the fibrocartilaginous and partially muscular layers, the submucous layer and the mucous membrane. In the fibrous layer, in addition to the cartilaginous half-rings, there is a network of elastic fibers. The fibrocartilaginous membrane of the trachea is connected to the adjacent organs by means of loose connective tissue.
The anterior and lateral walls of the trachea and large bronchi are formed by cartilages and annular ligaments located between them. The cartilaginous skeleton of the main bronchi consists of half rings of hyaline cartilage, which decrease in size as the diameter of the bronchi decreases and acquire the character of elastic cartilage. Thus, only large and medium bronchi consist of hyaline cartilage. Cartilages occupy 2/3 of the circumference, the membranous part - 1/3. They form a fibrocartilaginous skeleton, which ensures the preservation of the lumen of the trachea and bronchi.
Muscle bundles are concentrated in the membranous part of the trachea and main bronchi. A distinction is made between the superficial, or outer, layer, consisting of rare longitudinal fibers, and the deep, or inner, layer, which is a continuous thin membrane formed by transverse fibers. Muscle fibers are located not only between the ends of the cartilage, but also enter the inter-annular spaces of the cartilaginous part of the trachea and, to a greater extent, the main bronchi. Thus, in the trachea, smooth muscle bundles with a transverse and oblique arrangement are found only in the membranous part, i.e., the muscular layer as such is absent. In the main bronchi, rare groups of smooth muscles are present around the entire circumference.
With a decrease in the diameter of the bronchi, the muscular layer becomes more developed, and its fibers go in a slightly oblique direction. Contraction of the muscles causes not only a narrowing of the lumen of the bronchi, but also some shortening of them, due to which the bronchi participate in exhalation due to a decrease in the capacity of the respiratory tract. Contraction of the muscles allows the lumen of the bronchi to be narrowed by 1/4. When inhaling, the bronchus lengthens and expands. The muscles reach the respiratory bronchioles of the 2nd order.
Inside the muscular layer is the submucous layer, consisting of loose connective tissue. It contains vascular and nerve formations, a submucous lymphatic network, lymphoid tissue and a significant portion of the bronchial glands, which are of the tubular-acinous type with mixed mucous-serous secretion. They consist of terminal sections and excretory ducts that open into flask-shaped expansions on the surface of the mucous membrane. The comparatively large length of the ducts contributes to the long-term course of bronchitis during inflammatory processes in the glands. Atrophy of the glands can lead to drying of the mucous membrane and inflammatory changes.
The greatest number of large glands are located above the bifurcation of the trachea and in the area where the main bronchi divide into lobar bronchi. A healthy person secretes up to 100 ml of secretion per day. It consists of 95% water, and 5% is an equal amount of proteins, salts, lipids and inorganic substances. Mucins (high-molecular glycoproteins) predominate in the secretion. There are currently 14 types of glycoproteins, 8 of which are found in the respiratory system.
Mucous membrane of the bronchi
The mucous membrane consists of the integumentary epithelium, the basement membrane, the lamina propria of the mucous membrane and the muscularis mucosa.
The bronchial epithelium contains high and low basal cells, each of which is attached to the basal membrane. The thickness of the basal membrane varies from 3.7 to 10.6 μm. The epithelium of the trachea and large bronchi is multi-row, cylindrical, and ciliated. The thickness of the epithelium at the level of segmental bronchi ranges from 37 to 47 μm. It consists of 4 main types of cells: ciliated, goblet, intermediate, and basal. In addition, serous, brush, Clara, and Kulchitsky cells are found.
Ciliated cells predominate on the free surface of the epithelial layer (Romanova L.K., 1984). They have an irregular prismatic shape and an oval bubble-shaped nucleus located in the middle part of the cell. The electron-optical density of the cytoplasm is low. There are few mitochondria, the endoplasmic granular reticulum is poorly developed. Each cell carries short microvilli and about 200 ciliated cilia on its surface, 0.3 μm thick and about 6 μm long. In humans, the density of cilia is 6 μm 2.
Spaces are formed between adjacent cells; cells are connected to each other by finger-like outgrowths of the cytoplasm and desmosomes.
The population of ciliated cells is divided into the following groups according to the degree of differentiation of their apical surface:
- Cells in the phase of formation of basal bodies and axonemes. At this time, cilia are absent on the apical surface. During this period, accumulation of centrioles occurs, which move to the apical surface of the cells, and the formation of basal bodies, from which the axonemes of the cilia begin to form.
- Cells in the phase of moderately expressed ciliogenesis and cilia growth. On the apical surface of such cells a small number of cilia appear, the length of which is 1/2-2/3 of the length of the cilia of differentiated cells. In this phase, microvilli predominate on the apical surface.
- Cells in the phase of active ciliogenesis and cilia growth. The apical surface of such cells is almost entirely covered with cilia, the sizes of which correspond to the sizes of cilia of cells in the preceding phase of ciliogenesis.
- Cells in the phase of completed ciliogenesis and cilia growth. The apical surface of such cells is completely covered with densely arranged long cilia. Electron diffraction patterns show that the cilia of adjacent cells are oriented in the same direction and curved. This is an expression of mucociliary transport.
All these groups of cells are clearly visible in photographs obtained using light electron microscopy (SEM).
The cilia are attached to the basal bodies located in the apical part of the cell. The axoneme of the cilium is formed by microtubules, of which 9 pairs (doublets) are located along the periphery, and 2 single (singlets) are in the center. Doublets and singlets are connected by nexin fibrils. Each of the doublets has 2 short "handles" on one side, which contain ATPase, which participates in the release of ATP energy. Due to this structure, the cilia rhythmically oscillate with a frequency of 16-17 in the direction of the nasopharynx.
They move the mucous film covering the epithelium at a speed of about 6 mm/min, thereby ensuring continuous drainage function of the bronchus.
Ciliated epithelial cells, according to most researchers, are at the stage of final differentiation and are not capable of dividing by mitosis. According to the modern concept, basal cells are precursors of intermediate cells that can differentiate into ciliated cells.
Goblet cells, like ciliated cells, reach the free surface of the epithelial layer. In the membranous part of the trachea and large bronchi, ciliated cells account for up to 70-80%, while goblet cells account for no more than 20-30%. In places where there are cartilaginous semirings along the perimeter of the trachea and bronchi, zones with different ratios of ciliated and goblet cells are found:
- with a predominance of ciliated cells;
- with an almost equal ratio of ciliated and secretory cells;
- with a predominance of secretory cells;
- with a complete or almost complete absence of ciliated cells ("non-ciliated").
Goblet cells are single-celled glands of the merocrine type that secrete mucous secretion. The shape of the cell and the location of the nucleus depend on the phase of secretion and filling of the supranuclear part with mucus granules, which merge into larger granules and are characterized by low electron density. Goblet cells have an elongated shape, which during the accumulation of secretion takes the form of a goblet with a base located on the basal membrane and intimately connected with it. The wide end of the cell protrudes dome-shaped on the free surface and is equipped with microvilli. The cytoplasm is electron-dense, the nucleus is round, the endoplasmic reticulum is of the rough type, well developed.
Goblet cells are distributed unevenly. Scanning electron microscopy revealed that different zones of the epithelial layer contain heterogeneous areas consisting either of only ciliated epithelial cells or of only secretory cells. However, continuous accumulations of goblet cells are relatively few. Along the perimeter of a healthy person's segmental bronchus section, there are areas where the ratio of ciliated epithelial cells to goblet cells is 4:1-7:1, while in other areas this ratio is 1:1.
The number of goblet cells decreases distally in the bronchi. In the bronchioles, goblet cells are replaced by Clara cells, which participate in the production of serous components of mucus and alveolar hypophase.
In small bronchi and bronchioles, goblet cells are normally absent, but may appear in pathology.
In 1986, Czech scientists studied the reaction of the epithelium of the airways of rabbits to the oral administration of various mucolytic substances. It turned out that the target cells of the mucolytics are goblet cells. After the mucus is removed, goblet cells usually degenerate and are gradually removed from the epithelium. The degree of damage to the goblet cells depends on the substance administered: lasolvan has the greatest irritating effect. After the administration of broncholysin and bromhexine, massive differentiation of new goblet cells occurs in the epithelium of the airways, resulting in goblet cell hyperplasia.
Basal and intermediate cells are located deep in the epithelial layer and do not reach the free surface. These are the least differentiated cell forms, due to which physiological regeneration is mainly carried out. The shape of intermediate cells is elongated, basal cells are irregularly cubic. Both have a round, DNA-rich nucleus and a small amount of cytoplasm, which has a higher density in basal cells.
Basal cells are capable of giving rise to both ciliated and goblet cells.
Secretory and ciliated cells are united under the name "mucociliary apparatus".
The process of mucus movement in the airways of the lungs is called mucociliary clearance. The functional efficiency of the MCC depends on the frequency and synchronicity of the movement of the cilia of the ciliated epithelium, and also, very importantly, on the characteristics and rheological properties of the mucus, i.e. on the normal secretory capacity of the goblet cells.
Serous cells are few in number, reach the free surface of the epithelium and are distinguished by small electron-dense granules of protein secretion. The cytoplasm is also electron-dense. Mitochondria and rough reticulum are well developed. The nucleus is round, usually located in the middle part of the cell.
Secretory cells, or Clara cells, are most numerous in the small bronchi and bronchioles. Like serous cells, they contain small electron-dense granules, but are distinguished by the low electron density of the cytoplasm and the predominance of smooth, endoplasmic reticulum. The round nucleus is located in the middle part of the cell. Clara cells participate in the formation of phospholipids and, possibly, in the production of surfactant. Under conditions of increased irritation, they can apparently transform into goblet cells.
Brush cells have microvilli on their free surface but lack cilia. Their cytoplasm has low electron density, and their nucleus is oval and bubble-shaped. In the manual by Ham A. and Cormack D. (1982), they are considered goblet cells that have secreted their own secretion. They are attributed with many functions: absorption, contractility, secretory, chemoreceptor. However, they have been practically unstudied in the human airways.
Kulchitsky cells are found throughout the bronchial tree at the base of the epithelial layer, differing from basal cells by the low electron density of the cytoplasm and the presence of small granules that are revealed under an electron microscope and under a light microscope with silver impregnation. They are classified as neurosecretory cells of the APUD system.
Under the epithelium is the basement membrane, which consists of collagen and non-collagen glycoproteins; it provides support and attachment to the epithelium, participates in metabolism and immunological reactions. The condition of the basement membrane and the underlying connective tissue determines the structure and function of the epithelium. The lamina propria is a layer of loose connective tissue between the basement membrane and the muscle layer. It contains fibroblasts, collagen and elastic fibers. The lamina propria contains blood and lymphatic vessels. Capillaries reach the basement membrane, but do not penetrate it.
In the mucous membrane of the trachea and bronchi, mainly in the proper plate and near the glands, in the submucosa, there are constantly free cells that can penetrate through the epithelium into the lumen. Among them, lymphocytes predominate, plasma cells, histiocytes, mast cells (labrocytes), neutrophilic and eosinophilic leukocytes are less common. The constant presence of lymphoid cells in the mucous membrane of the bronchi is designated by a special term "broncho-associated lymphoid tissue" (BALT) and is considered as an immunological protective reaction to antigens penetrating the respiratory tract with air.


 [
[