Medical expert of the article
New publications
Vaginitis (colpitis)
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Vaginitis is an infectious or non-infectious inflammatory process of the vaginal mucosa, and sometimes the vulva. The main clinical manifestations of the disease include the following symptoms: vaginal discharge, irritation, itching and hyperemia of the mucous membrane. Diagnosis is based on the study of vaginal secretions. Treatment is aimed at the cause of the disease and the elimination of clinical symptoms.
Vaginitis is one of the most common and frequent gynecological diseases. Most often, the vulva (vulvitis) or the vulva and vagina (vulvovaginitis) are affected.
Causes vaginitis
The most common causes of the disease change with the age of the patients.
In children, vaginitis is usually caused by an infection and microflora of the gastrointestinal tract (non-specific vulvovaginitis). Common triggers in girls aged 2-6 years include poor hygiene of the external genitalia (e.g., wiping the external genitalia from back to front after defecation; not washing hands after using the toilet; scratching the genitals when there is itching). Chemicals in bubble baths or soaps can cause inflammation. Foreign bodies (e.g., wipes) can also cause non-specific vaginitis with bloody vaginal discharge. Sometimes vulvovaginitis in girls is caused by infection with certain infectious agents (e.g., streptococci, staphylococci, candida), sometimes pinworms.
Women of reproductive age most often develop vaginitis of an infectious nature. The most common type of lesion is trichomonas vaginitis, which is sexually transmitted; bacterial vaginosis and candidal vaginitis. Normally, saprophytic lactobacilli are the predominant element of normal vaginal microflora in women of reproductive age. Microbial seeding with these bacteria maintains the pH of the vaginal contents in the normal range (3.8-4.2), thus preventing the proliferation of pathogenic bacteria and fungi. In addition, high estrogen levels maintain the thickness of the vaginal epithelium, thus supporting local protection.
Risk factors
There are factors that lead to the proliferation of bacterial and fungal infectious microorganisms in the vagina, shifting the pH of the vaginal contents to the alkaline side. These changes are enhanced during menstruation, during sexual contact with infected sperm. A decrease in the number of lactobacilli in the vagina is associated with wearing tight underwear with poor aeration, poor hygiene and frequent vaginal douching. Vaginitis can be the result of the introduction of foreign bodies into the vagina (for example, forgotten tampons). Non-infectious vaginitis is less common.
After menopause, there is a decrease in estrogen in the body, which leads to thinning of the vaginal mucosa and increases the risk of infection and inflammation. Some treatments (eg, removal of the ovaries, pelvic radiation, some types of chemotherapy) also lead to a decrease in estrogen levels. Poor genital hygiene (eg, in patients with urinary incontinence or confined to bed) can lead to chronic inflammation of the vulva and vagina due to chemical irritation from urine and feces or as a result of non-specific infection.
Bacterial vaginosis, candidal vaginitis and trichomonas vaginitis are less common in postmenopausal women, but inflammatory processes can develop in patients with risk factors. At any age, there are certain factors that predispose to the development of vaginal or vulvar infection. These are fistulas between the intestine and the genital tract, which allow intestinal microflora to settle in the genital tract; irradiation of the pelvic organs; the presence of tumors that affect tissues and thus lead to a decrease in the body's defenses. Noninfectious vulvitis can occur at any age as a result of hypersensitivity or allergic reaction to hygiene sprays or perfumes, menstrual pads, laundry soap, bleach, fabric softener, dye, synthetic fibers, bubble bath, toilet paper, sometimes spermicidal vaginal lubricants or creams, latex condoms, vaginal contraceptive rings, or diaphragms.
 [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ]
[ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ]
Symptoms vaginitis
Vaginitis causes increased vaginal discharge, which must be distinguished from normal discharge. Normal discharge is most common when estrogen levels in the body are high. For example, newborn girls often have slight vaginal bleeding during the first 2 weeks of life, which is due to the fact that the levels of estrogens transferred to her from the mother at birth decrease sharply. Estrogen levels increase during the few months leading up to menarche. During this period, normal vaginal discharge appears. Normal vaginal discharge is usually milky white and mucous, odorless, and does not irritate the vaginal epithelium. Normal discharge helps to moisturize the vagina and may leak onto underwear. Abnormal discharge resulting from vaginitis is accompanied by itching, hyperemia of the mucous membrane, sometimes burning, pain, or moderate bleeding. Itching intensifies during sleep. Dysuric disorders or dyspareunia also occur.
In atrophic vaginitis, vaginal discharge is scanty, dyspareunia is most common, the vaginal mucosa becomes thinner and dryness increases. Although symptoms vary with different types of vaginitis, they have much in common.
Vulvitis can cause hyperemia, itching and sometimes pain, discharge from the vulva.
Cervical discharge may be due to cervicitis (eg, due to pelvic inflammatory disease); may resemble vaginitis; abdominal pain, tenderness when moving the cervix, or cervicitis due to pelvic inflammatory disease. Watery discharge mixed with blood may be due to vulvar or vaginal cancer; cancer can be differentiated from vaginitis by performing a Papanicolaou test. If girls have vaginal discharge, a foreign body may be suspected. Vaginal itching and discharge may result from skin lesions (eg, psoriasis, dermatomycosis), which can be differentiated from the history of the disease and the results of skin examination.
Where does it hurt?
What's bothering you?
Forms
Violations |
Symptoms |
Criteria for diagnosis |
Results of microscopic examinations |
Differential diagnosis |
Inflammatory |
Symptoms related to the postmenopausal period: purulent discharge, vaginal dryness, thinning of the mucous membrane, dyspareunia, dysuria |
PH> 6, negative amine test and characteristic microscopic examination results |
Increased polymorphonuclear cells and cocci; decreased lactobacilli; parabasal cells |
Erosive lichen planus |
Bacterial vaginosis |
Gray, foul-smelling discharge, often itchy and irritating; no dyspareunia |
Three of the following: gray discharge, pH > 4.5, fishy odor, clue cells |
Key cells; decreased lactobacilli; increased coccobacillary microflora |
Trichomonas vaginitis |
Candidal |
Thick white discharge; vaginal or vulvar itching with or without burning, irritation, or dyspareunia |
Typical discharge, pH <4.5 and microscopic examination results |
Yeast-like fungi, pseudomycelium or mycelium; best tested with 10% potassium hydroxide solution |
Contact irritant or allergic vulvitis, chemical irritation, vulvodynia |
Trichomonas vaginitis |
Profuse, foul-smelling, yellow-green discharge; dysuria; dyspareunia; hyperemia |
Identification of a pathogenic microorganism by microscopy (sometimes culture diagnostics) |
Motile protozoa; enlarged polymorphonuclear cells |
Bacterial vaginosis, inflammatory vaginitis |
Diagnostics vaginitis
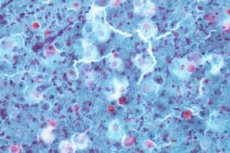
Vaginitis is diagnosed based on the clinical picture and laboratory data. First, vaginal secretions obtained during speculum examination are examined and the pH of the vaginal contents is determined (in the range from 4.0 to 6.0). The secretions are then applied to two slides using a cotton swab and diluted with 0.9% sodium chloride solution on the first slide (saline wet fixation) and 10% potassium hydroxide on the second slide (KOH fixation).
Culture data are required if microscopic examination results are negative or if symptoms persist.
If a fishy odor (amine test) is detected during the KOH test, which is a result of amine production, trichomonas vaginitis or bacterial vaginosis may be suspected. The wet saline smear should be examined microscopically as soon as possible to detect trichomonads. After some time from smear fixation, trichomonads become immobile and are more difficult to diagnose microscopically. KOH destroys cellular material, with the exception of yeast fungi, facilitating identification of the pathogen. If the clinical picture and laboratory data are insufficient to establish a diagnosis, it is necessary to take secretions for fungal culture.
In cases of trichomonas vaginitis in children, sexual abuse should be excluded; if they have unexplained vaginal discharge, cervicitis, testing for sexually transmitted infections is necessary. If women have bacterial vaginosis or trichomonas vaginitis (and thus have an increased risk of developing sexually transmitted diseases), cervical tests should be performed to detect gonorrhea or chlamydia as the most common causes of sexually transmitted diseases (sexually transmitted diseases) of the pelvic organs.
What do need to examine?
What tests are needed?
Who to contact?
Treatment vaginitis
Measures to reduce vulvar discharge and microbial growth include maintaining genital hygiene, wearing loose clothing, and using absorbent cotton balls to improve air circulation. Soaps and unproven hygiene products (such as feminine hygiene sprays) should be avoided. Periodic use of ice or warm sitz baths with or without baking soda may reduce soreness and itching.
If the symptoms of the disease are moderate or severe or do not respond to treatment with the above measures, it is necessary to prescribe medications. In case of itching, it is relevant to prescribe glucocorticoids (for example, 1% hydrocortisone for topical use) for treatment of the vulva, but not the vagina. Oral antihistamines reduce itching and cause drowsiness, helping to improve patient sleep.
Any infection or other causes of vaginitis require treatment. Foreign bodies should be removed. Prepubertal girls are taught proper genital hygiene (e.g., wiping the genitals from front to back after bowel movements; careful hand washing). If vulvar inflammation is due to urinary incontinence or in bedridden patients, proper genital hygiene may be the best solution.
More information of the treatment
Prevention
Prevention of candidal vaginitis includes the use of cotton underwear. Avoid using vaginal scented soaps, shower gels, deodorants. Douching is not recommended, as it disrupts the normal bacterial balance in the vagina.
Prevention of bacterial vaginosis includes healthy eating and minimizing stressful situations.
Prevention of the trichomoniasis form of colpitis consists of practicing safe sex by using condoms.

