Medical expert of the article
New publications
Cytologic studies of vaginal discharge
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The cytological method of research is one of the main methods for diagnosing precancerous and malignant diseases of the female reproductive system.
All women are subject to cytological examination for prophylactic purposes at least once every 6 months, and dispensary patients - once every 3 months; this examination method plays a major role primarily in high-risk disease groups.
For cytological examination of the cervix, the material should be taken from the ectocervix and cervical canal using anatomical tweezers, a Volkman spoon, a grooved probe, a special metal Eyre spatula, wooden plates. The material is taken with dry sterile instruments to avoid cell destruction.
Native smears can be examined using a phase-contrast microscope or stained with hematoxylin and eosin and treated with fluorochrome.
The nature of the pathological process is recognized by the following features: morphological characteristics of cells, quantitative relationship of individual cell groups, location of cellular elements in the preparation.
When evaluating the results of a cytological study, it should be borne in mind that the main control over the correctness of the cytological diagnosis is the histological conclusion.
Screening cytological methods
They are produced for the purpose of early detection of uterine cancer and cervical cancer. The nature of the pathological process is recognized based on the following features: morphological features of cells, quantitative relationship of individual cell groups, location of cellular elements in the preparation.
Pap smear
This is a simple and effective test for detecting changes in the cells of the cervical epithelium. Developed in 1943, this test was originally designed to detect only cancer cells. Currently, this test can be used to detect background and precancerous diseases of the cervix. The Papanicolaou test uses a specially selected composition of fixatives and dyes, which allows for the highest degree of reliability in detecting early precancerous diseases of the cervix. This method is standard for developed countries in Europe and America, as it gives the least number of false negative results.
Hormonal colpocytology
The method is based on the determination of individual types of epithelial cells (superficial, keratinizing, intermediate, parabasal and basal) in vaginal smears. The material for the study is taken from the posterior vaginal fornix. In women of reproductive age with a two-phase menstrual cycle, only superficial and intermediate cells are found in various ratios in the smear during microscopy. The karyopyknotic index (KPI) is calculated based on the ratio of keratinizing cells and the total number of superficial cells.
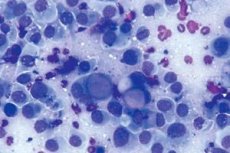
Colpocytology (cytological examination of vaginal discharge)
Colpocytological examination of the cellular composition of vaginal smears is based on cyclic changes in the vaginal epithelium (vaginal cycles). They are characterized by the degree of epithelium maturation, as a result of which parabasal (oval with a large nucleus) and intermediate cells (spindle-shaped with transparent cytoplasm and a vesicular nucleus with a clear chromatin pattern) are determined in the smear. Superficial cells originate from the uppermost layers of the epithelium. These are large polygonal cells with a structureless (pyknotic) nucleus. They appear with maximum proliferation of the epithelium, which is observed with increased estrogenic stimulation of the body.
The quantitative ratio of cells in a smear and their morphological characteristics are the basis of hormonal cytodiagnostics.
Research methodology.
- The material is taken from the lateral parts of the vault of the upper third of the vagina, as they are most sensitive to hormonal influences.
- When taking a smear, one must not manipulate it roughly, since the cells that are being examined are those that have separated from the vaginal walls. Failure to comply with this rule results in cells from the lower layers of the epithelium getting into the smear, the presence of which is interpreted as hormonal deficiency.
- When analyzing a smear, the patient's age and the day of the menstrual cycle should be taken into account.
- 2-3 days before the examination, it is necessary to stop all vaginal manipulations and recommend the woman to abstain from sexual activity. Polychrome staining methods are predominantly used.
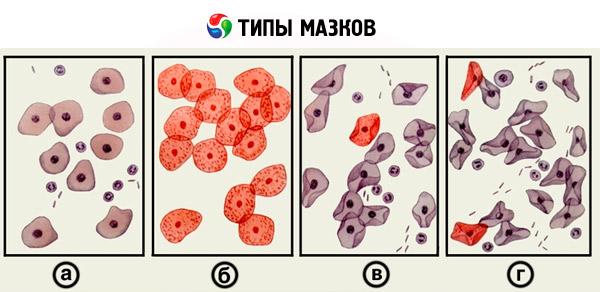
In the cellular composition of vaginal smears, four degrees of estrogen saturation of the body are distinguished.
- The first type of smear (the first reaction) - basal cells with large nuclei are determined in it. Epithelial cells of other layers are absent. Leukocytes may be present. Such a picture of the smear reflects significant estrogen deficiency.
- The second type of smear (second reaction) - predominantly parabasal cells with large nuclei are visible. Among them, there may be individual cells of the intermediate and basal layers. Leukocytes are single or absent. The picture reflects the average degree of estrogen deficiency.
- The third type of smear (the third reaction) - mainly intermediate layer cells with medium-sized nuclei are represented, sometimes superficial cells are encountered. This type of smear characterizes minor estrogen deficiency.
- The fourth type of smear (the fourth reaction) - predominantly large and flat, well-defined cells of the superficial layer with a small (pyknotic) nucleus are found. The smear indicates sufficient estrogenic saturation.
The following indices are calculated:
- maturation index (MI, numerical index) - the percentage ratio of superficial, intermediate and parabasal cells. It is written as follows: 2/90/8, which means that in the examined smear there are 2% parabasal, 90% intermediate and 8% superficial cells;
- karyopyknotic index (KI) - the percentage of superficial cells with pyknotic nuclei (less than 6 µm in diameter) to cells with vesicular (non-pyknotic) nuclei more than 6 µm in diameter. Characterizes the estrogenic saturation of the body, since only estrogenic hormones cause proliferative changes in the vaginal mucosa;
- eosinophilic index (EI) - the percentage of surface cells with eosinophilically stained cytoplasm to cells with basophilic cytoplasm. Characterizes exclusively the estrogenic effect on the vaginal epithelium.
Due to the embryological similarity of the vaginal and urinary bladder mucosa, the latter also reflects hormonal changes occurring in the woman's body. Urocytology is indicated in cases where colpocytological studies are difficult or impossible ( colpitis, vulvovaginitis, prolonged uterine bleeding ).
What's bothering you?
What do need to examine?
What tests are needed?

