Medical expert of the article
New publications
Cervical precancerous lesions
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Precancerous diseases of the cervix or dysplasia are diseases characterized by atypia of the cells of the mucous membrane of the cervix and cervical canal.
Precancerous conditions are not cancer yet, but under certain circumstances and without treatment they have a high chance of transforming into cervical cancer.
Pathogenesis
The pathogenesis of this process is based on a disruption in the maturation and differentiation of cells in part of the layer of stratified squamous epithelium covering the cervix.
The formation of dysplasia can occur in two directions:
- in the process of squamous cell metaplasia of reserve cells and
- against the background of disruption of physiological transformations in the stratified squamous epithelium, occurring under the influence of the hypothalamic-pituitary-ovarian system.
In mild dysplasia, proliferation of cells in the deepest layers of squamous epithelium - basal and parabasal - is observed; the cells of the upper part of the layer are mature and differentiated and retain normal structure and polarity of location.
The moderate form of dysplasia is characterized by the involvement of the lower half of the epithelial layer in the pathological process; cell atypia is not observed in mild and moderate forms of dysplasia.
The classification of severe dysplasia or preinvasive cancer into the CIN III category is determined by the similar clinical manifestation of these processes and treatment approaches. The peculiarity of this form of dysplasia is the preservation of maturation and differentiation of cells only in the superficial layer of squamous epithelium, as well as pronounced atypia of its cells (enlargement and hyperchromia of nuclei).
Macroscopically, dysplasia can appear as ectopia, ectropion, or leukoplakia.
Symptoms cervical precancerous lesions
In most women, background and precancerous diseases of the cervix are latent. Women consider themselves practically healthy and do not complain.
Clinical manifestations of a more pronounced process suspicious for malignant transformation include the appearance of watery leucorrhoea, contact bleeding, and scanty bloody discharge before and after menstruation.
Where does it hurt?
Diagnostics cervical precancerous lesions
A comprehensive examination of patients with background and precancerous processes of the cervix includes bacterioscopic and bacteriological examination of discharge from the vagina, cervical canal and urethra, colposcopy, cytological and histological examination of the cervix.
 [ 17 ], [ 18 ], [ 19 ], [ 20 ]
[ 17 ], [ 18 ], [ 19 ], [ 20 ]
Colposcopy
Extended colposcopy is a mandatory method of comprehensive examination of patients, since many pathological processes of the cervix, including early forms of cancer, are asymptomatic. Colposcopy evaluates:
- color;
- state of the vascular pattern;
- surface and level of stratified squamous epithelium;
- transition zone of the epithelium (cervical canal and cervix);
- the nature and shape of the glands;
- reaction to a test with acetic acid solution;
- reaction to Schiller's test.
The test with acetic acid (3% solution) has the following purposes:
- remove mucus from the surface of the cervix;
- cause short-term swelling of the epithelium and, accordingly, change the color of the mucous membrane;
- cause spasm of unchanged vessels.
Against the background of pale edematous mucous membrane, the boundaries of flat and columnar epithelium, the level of columnar epithelium, as well as various pathological transformations of multilayered flat epithelium are more clearly identified. Moreover, against the background of mucous membrane edema, unchanged vessels spasm, while atypical vessels, on the contrary, become more pronounced and distinct.
Schiller test - iodine molecules, interacting with glycogen (substrate of mature stratified squamous epithelium), stain the unchanged mucous membrane dark (iodine-positive zones). Immature, keratinized squamous epithelium, cylindrical and atypical epithelium, not containing or having a small amount of glycogen, are not stained at all or acquire a weak shade (iodine-negative zones)
Colpomicroscopy
The method is a lifetime histological examination of the cervix. Colpomicroscopy has an advantage over colposcopy, since the results of this method are comparable with histological examination. In comparison with cytological examination, colpomicroscopy differs in that it allows studying the morphological structure of not individual cells or their complexes, but the structure of the tissue without violating the integrity of the cells. However, due to the relative complexity of the technique, colpomicroscopy is not widely used in everyday practice.
Cytological examination
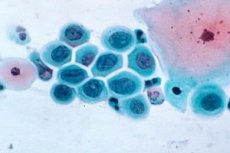
Normally, cytological preparations of smears from various parts of the cervix contain unchanged cells of the stratified squamous epithelium, as well as prismatic cells lining the cervical canal. In background processes, smears contain a significant amount of cylindrical epithelial cells. Mild dysplasia is characterized by the predominance of cells of the intermediate layer of squamous epithelium with signs of dyskaryosis in the form of nuclear hypertrophy and a slight violation of the nuclear-cytoplasmic ratio; with a moderate degree of dysplasia, parabasal layer cells with signs of nuclear atypia prevail. Severe dysplasia is characterized by the appearance in smears of an increased number of basal and parabasal cells with pronounced signs of dyskaryosis, a violation of the nuclear-cytoplasmic ratio, and an increase in the number of mitoses.
The accuracy of cytological diagnostics of dysplastic changes does not exceed 30%, background processes - 50%. Therefore, diagnostics of pathological conditions of the cervix is carried out only in accordance with the results of histological examination of biopsy material.
 [ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ], [ 32 ], [ 33 ]
[ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ], [ 32 ], [ 33 ]
Biopsy
Biopsy is the most accurate method of diagnosing cervical diseases. Biopsy is recommended in all cases of long-term non-healing erosions. Cervical tissue for biopsy is taken from an iodine-negative area.
What do need to examine?
Who to contact?
Treatment cervical precancerous lesions
In the treatment of background processes of the cervix, two methods are distinguished - medicinal and non-medicinal.
Medicinal method
The method is based on the general or local effect of drugs on the pathologically altered integumentary epithelium of the cervix and uterus. Drug therapy is carried out in the form of local applications of drugs (solkovagin, vagotyl). The drugs are a mixture of organic and inorganic acids that have a selective coagulating effect on the cylindrical epithelium. During treatment, they are applied to the pathological focus without damaging healthy tissue. The treatment is painless and does not cause side effects. Cicatricial changes in the cervix after drug treatment do not form; a correctly applied drug ensures complete destruction of the pathological focus due to sufficient penetration depth.
 [ 38 ], [ 39 ], [ 40 ], [ 41 ], [ 42 ], [ 43 ], [ 44 ]
[ 38 ], [ 39 ], [ 40 ], [ 41 ], [ 42 ], [ 43 ], [ 44 ]
Non-drug method
Non-drug treatment of background processes of the cervix includes:
- laser exposure (high and low intensity);
- cryodestruction;
- surgical intervention.
 [ 45 ], [ 46 ], [ 47 ], [ 48 ], [ 49 ]
[ 45 ], [ 46 ], [ 47 ], [ 48 ], [ 49 ]
Low-intensity laser therapy (infrared or helium-neon radiation)
The mechanism of biological action of low-intensity laser radiation is based on the interaction of the electric field created by the laser beam with the body's own electromagnetic fields of cells and tissues. Infrared laser radiation stimulates the activity of the most important bioenergetic enzymes - dehydrogenase and cytochrome oxidase, catalase, and other enzymes of cellular metabolism. Low-intensity laser accelerates regenerative processes of epithelial tissues, stimulates blood circulation and hematopoiesis, and also has an anti-inflammatory, analgesic and bactericidal effect. The method of low-intensity laser therapy involves irradiating the affected area of the cervix for 3-5 minutes (10-15 procedures).
Medicinal and/or low-intensity laser therapy is carried out for no more than 3 weeks; if there is no positive effect, destructive treatment methods are indicated. High-intensity laser exposure. Carbon dioxide (CO 2 ) radiation is used to treat cervical diseases. The mechanism of action of the CO 2 laser is based on a sufficiently strong absorption of coherent radiation by biological tissues, which results in rapid heating and destruction of the biotissue in the laser beam exposure zone. At the initial stage of laser radiation, decomposition of the biotissue is observed with evaporation of the liquid and carbonization of the solid phases; subsequently, with an increase in temperature, the carbonized framework of the biotissue burns out.
CO2 laser vaporization of the epithelial layer of the cervix is painless, does not cause scab formation or stenosis of the cervical canal, tissue necrosis is minimal, and recovery times are shorter than with other methods of physical destruction.
Cryodestruction
Low-temperature exposure has a wide range of biological effects - from cryopreservation to cryodestruction of tissues.
Cryocoagulation is carried out by contact method, liquid gases are used as a cooling agent - nitrogen and its oxide, freon, carbon dioxide, as well as physical factors that potentiate the cryoeffect - electromagnetic radiation, ultrasound, exposure to radioactive isotopes. The duration of cryoapplication is determined by the nature and prevalence of the pathological process and is on average 3-4 minutes.
The advantages of cryodestruction include the formation of a limited necrosis zone with minor damage to surrounding tissues, the absence of sclerosis of connective tissue, and the painlessness of the procedure; the disadvantages include long periods of regeneration of squamous epithelium, prolonged tissue exudation, incomplete freezing both in depth and on the surface, which does not ensure the death of all pathologically altered cells and, thus, increases the possibility of relapse of cervical diseases, the frequency of which after cryotherapy reaches 42%.
Post-traumatic background diseases of the cervix are subject to surgical treatment - ruptures, ectropion, cicatricial deformation, cervicovaginal fistulas. For these purposes, various types of reconstructive plastic surgeries are used (wedge and cone amputation, plastic surgery of the cervix, suturing of cervicovaginal fistulas).
In case of congenital or physiological ectopia, only dynamic observation is carried out.

