Tumors of the ovaries
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Tumors of the ovaries can be divided into three main groups:
- Functional.
- Benign.
- Malignant.
In particular, functional cysts account for about 24% of all ovarian tumors, benign tumors - 70% and malignant tumors - 6%.
Epidemiology
Tumors of the ovaries occupy the second place among all neoplasms of the female genital organs, after uterine myoma. They occur at any age, but mostly after 40 years. Among them prevalent benign forms (75-80%), malignant forms occur in 20-25%. Over the past 10 years, the incidence of genital cancers has increased by 15%.
The incidence of cysts among ovarian tumors is 35%. First of all, these are follicular cysts, yellow body cysts, endometriomas. Ovarian cysts occur more often during puberty and in reproductive age.
Pathogenesis
Tumors of the ovaries in the clinical course are divided into benign, borderline and malignant.
Sources of origin of ovarian tumors:
- normal components of the ovary;
- embryonic remains and dystopia;
- postnatal proliferation, heterotopia, metaplasia of the epithelium.
Among the practical doctors, for the definition of ovarian tumors, the terms of the ovarian cyst and cystoma are common:
Ovarian cyst is a retention non-proliferating formation.
Ovarian cyst is a true proliferating formation.
In modern oncogynecology, "cysts and cysts" of the ovaries are usually called cystadenoma.
Forms
The histological classification and terminology of ovarian tumors was approved by WHO in 1973, but in view of its complexity for practical practitioner SK Serov (1978), a more simplified and compact classification was developed that includes all forms of tumors presented in the WHO classification.
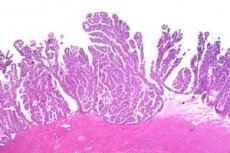
I. Epithelial tumors
A. Serous, mucinous, endometrioid, meson-fungal and mixed:
- benign: cystadenoma, adenofibroma, superficial papilloma;
- border: intermediate forms of cystaden and adenofibrom;
- malignant: adenocarcinoma, cystadenocarcinoma, papillary carcinoma.
B. Brenner's tumor:
- benign;
- border crossing point;
- malignant.
II. Sexual stroma tumors
- A. Granulose-Tecacellular Tumors: Granuloseocular, Tecom-Fibrom Groups, Unclassified Tumors.
- B. Androblastomas, tumors from Sertoli and Leydig cells (differentiated, intermediate, low-differentiated).
- S. Gynandroblastoma.
- D. Unclassified tumors.
III. Lipid-cell tumors
IV. Germinogenic tumors
- A. Disgerminoma.
- B. Tumor of the endodermal sinus.
- C. Embryonic carcinoma.
- D. Polyembrynoma.
- E. Chorioncinoma.
- F. Teratomas (mature, immature).
- G. Mixed germ cell tumors.
V. Gonadoblastoma
VI. Tumors of soft tissues (nonspecific for ovaries)
VII. Unclassified tumors
VIII. Secondary (metastatic) tumors
IX. Tumor and precancerous processes: pregnancy luteosis, hypertecosis, follicular cysts, yellow body cyst, endometriosis, inflammatory processes, parovarial cyst.
Based on this classification, we can conclude that in its histological structure, ovarian tumors are very diverse.
According to the clinical course of the tumor, the ovaries are divided into benign, borderline and malignant.
Benign ovarian tumors include tumors with minimal proliferation of epithelial cells or a small degree of atypicality.
Bordered tumors are a kind of transitional biological stage of blastomogenesis and belong to the group of potentially low degree of malignancy, there is no obvious invasion of the adjacent stroma. However, borderline tumors can sometimes be implanted over the peritoneum and cause distant metastases. Clinically proven high survival rates of patients with borderline ovarian tumors.
Malignant tumors of the ovaries are tumors of different degree of maturity of the cellular structure, they have rapid growth, spread, give metastases to various organs, their prognosis depends on early detection and completeness of the treatment.
To understand the clinical course of certain complications arising in patients with ovarian cystadenomas, as well as in the surgical treatment of this pathology, it is important to clearly define the concepts of the anatomical and surgical leg of the ovarian tumor.
Anatomic leg of the ovarian tumor: its own ligament, funnel-pelvic ligament, part of a broad ligament.
The surgical leg of the tumor: the ovary's own ligament, the funnel-pelvic ligament, part of the broad ligament, the uterine tube.

What do need to examine?
Who to contact?

