Medical expert of the article
New publications
Malignant ovarian tumors
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
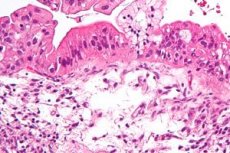
Primary cancer is a malignant tumor that primarily affects the ovary. Secondary ovarian cancer (cystadenocarcinoma) is the most common malignant tumor of this organ. It most often develops in serous, less often mucinous cystadenomas. Secondary ovarian lesions include endometrioid cystadenocarcinoma, which often develops in young women suffering from primary infertility.
Epidemiology
The incidence ranges from 3.1 cases per 100,000 women in Japan to 21 cases per 100,000 women in Sweden. Worldwide, more than 200,000 women develop ovarian cancer each year, and about 100,000 die from the disease. Epithelial cancer occurs most often in white women in the industrialized countries of northern and western Europe and North America, and least often in India and Asia.
Risk factors
- menstrual cycle disorders: early menarche, early (before 45 years) or late (after 55 years) menopause, uterine bleeding;
- reproductive function (infertility);
- uterine fibroids;
- genital endometriosis;
- hyperplastic processes of the endometrium;
- operations for tumors of the internal genital organs with the preservation of one or both ovaries;
- diseases of the mammary glands (mastopathy, fibroadenomatosis).
Pathogenesis
The clinical course of malignant ovarian tumors is characterized by aggressiveness, a short period of tumor doubling, and a universal nature of metastasis. The regional lymph nodes for the ovaries are the iliac, lateral sacral, para-aortic, and inguinal lymph nodes. The implantation route of distant metastasis is predominant - into the parietal and visceral peritoneum, pleura, carcinomatous ascites, and hydrothorax. Lymphogenous metastases (into the para-aortic and iliac collectors) are observed in 30-35% of primary patients. Hematogenous metastases in the lungs and liver are never isolated. They are often determined against the background of extensive implantation and lymphogenous dissemination.
Symptoms ovarian malignancies
Malignant ovarian tumors are characterized by the following symptoms: abdominal pain (pulling, constant, increasing, sudden, paroxysmal, etc.), changes in general condition (fatigue, weakness, dry mouth, etc.), weight loss, abdominal enlargement, changes in menstrual function, the appearance of acyclic bloody discharge from the genital tract, etc.
Where does it hurt?
Stages
Currently, oncology uses the TNM classification of malignant ovarian tumors:
T – primary tumor.
- T0 – the primary tumor is not detected.
- T1 – the tumor is limited to the ovaries.
- T1A – the tumor is limited to one ovary, there is no ascites.
- T1B – the tumor is limited to both ovaries, no ascites.
- T1C - the tumor is limited to one or both ovaries, ascites or malignant cells are present in the abdominal lavage.
- T2 – the tumor affects one or both ovaries with extension to the parametria.
- T2A - tumor with extension and/or metastases to the uterus and/or one or both tubes, but without involvement of the visceral peritoneum and without ascites.
- T2B – the tumor spreads to other tissues and/or affects the visceral peritoneum, but without ascites.
- T2C - tumor extends into the uterus and/or one or both tubes, and/or other pelvic tissues. Ascites.
- T3 - the tumor affects one or both ovaries, extends into the small intestine or omentum, is limited to the pelvis, or there are intraperitoneal metastases outside the pelvis or in the retroperitoneal lymph nodes.
N – regional lymph nodes.
- N0 – no signs of damage to regional lymph nodes.
- N1 – there is damage to regional lymph nodes.
- NX – insufficient data to assess the condition of regional lymph nodes.
M – distant metastases.
- M0 – no signs of distant metastases.
- Ml – there are distant metastases.
- MX – insufficient data to determine distant metastases.
In practice, a classification of ovarian cancer is used depending on the stage of the tumor process, which is determined on the basis of a clinical examination and during surgery.
Stage I – the tumor is limited to the ovaries:
- Stage 1a – the tumor is limited to one ovary, there is no ascites;
- Stage 16 – the tumor is limited to both ovaries;
- Stage 1b – the tumor is limited to one or both ovaries, but there is obvious ascites or atypical cells are detected in the washings.
Stage II – the tumor affects one or both ovaries and spreads to the pelvic area:
- Stage IIa – spread and/or metastases on the surface of the uterus and/or fallopian tubes;
- Stage IIb – spread to other pelvic tissues, including the peritoneum and uterus;
- Stage IIb – spread as in IIa or II6, but there is obvious ascites or atypical cells are detected in washings.
Stage III – spread to one or both ovaries with metastases to the peritoneum outside the pelvis and/or metastases to the retroperitoneal lymph nodes:
- Stage IIIa – microscopic metastases in the peritoneum;
- Stage IIIb – macrometastases in the peritoneum less than or equal to 2 cm;
- Stage IIIb – metastases in the peritoneum more than 2 cm and/or metastases in the regional lymph nodes and omentum.
Stage IV – spread to one or both ovaries with distant metastases (distant lymph nodes, liver, navel, pleura). Ascites.
Diagnostics ovarian malignancies
The age of the patient, which determines the frequency of occurrence of various tumors, disease progression and treatment prognosis.
The patient's profession, especially one associated with exposure to unfavorable production and environmental factors, may be a risk factor for the development of tumor processes.
General examination: skin color, weight loss, leg swelling, abdominal enlargement, condition of peripheral lymph nodes, abdominal palpation (size, soreness, mobility, tumor consistency, presence of ascites).
Gynecological examination and vaginal-rectal examination: condition of the cervix and body of the uterus, presence of a tumor in the appendages, its size, consistency, connection with surrounding organs, condition of the recto-vaginal septum, Douglas pouch and parametria.
Additional research methods
Ultrasound of the pelvic organs, computed tomography and magnetic resonance imaging, puncture of the Douglas pouch with subsequent cytological examination of the lavage, diagnostic laparoscopy (laparotomy) with express biopsy and taking smears-prints to clarify the histotype of the tumor, and revision of the abdominal organs (in the case of a malignant tumor, the extent of the spread of the process is determined).
In order to clarify the condition of adjacent organs and the features of the tumor topography, irrigoscopy, excretory urography, fibrogastroscopy, X-ray examination of the chest organs, etc. are indicated.
Immunological methods for early diagnosis of ovarian cancer – determination of tumor markers CA-125 (for serous and poorly differentiated adenocarcinoma), CA-119 (for mucinous cystadenocarcinoma and endometrioid cystadenocarcinoma), glycoprotein hormone (for granulosa cell and mucinous ovarian cancer).
What do need to examine?
What tests are needed?
Who to contact?
Treatment ovarian malignancies
Basic principles of treatment of patients with various ovarian tumors
Benign tumors - In reproductive age (up to 45 years) - removal of the uterine appendages on the affected side. In case of bilateral tumors in young women - tumor resection with possible preservation of ovarian tissue. In pre- and postmenopause - supravaginal amputation or extirpation of the uterus with appendages.
Malignant tumors - At stages I and II, treatment begins with surgery (extirpation of the uterus with appendages and removal of the greater omentum), followed by chemotherapy. At stages III and IV, treatment begins with polychemotherapy, followed by cytoreductive surgery (maximum possible removal of tumor masses and metastases, supravaginal amputation or extirpation of the uterus with appendages, removal of the greater omentum and metastatic nodes). Subsequently, repeated courses of polychemotherapy.
Borderline tumors - Extirpation of the uterus with appendages and omentectomy are indicated. In young women, organ-preserving surgery is possible (removal of the tumor and resection of the greater omentum), which is supplemented by several courses of adjuvant polychemotherapy (especially in case of tumor capsule invasion or the presence of implantation metastases).
Currently, comprehensive treatment of patients with malignant ovarian tumors is considered adequate: a combination of surgery with polychemotherapy and (or) remote irradiation of the pelvis and abdominal cavity. In most cases, it is preferable to begin treatment with surgery. In case of ascites and hydrothorax, platinum preparations can be administered into the abdominal or pleural cavity. Polychemotherapy includes several antitumor drugs with different mechanisms of action. In the postoperative period, polychemotherapy is carried out after receiving the results of a histological examination of the removed organs.
Standard regimens for polychemotherapy of ovarian cancer
| Scheme | Composition, course |
| SR | Cisplatin – 75 mg/ m2 and cyclophosphamide 750 mg/ m2 intravenously every 3 weeks, 6 courses |
| SAR | Cisplatin – 50 mg/ m2, doxorubicin 50 mg/ m2 and cyclophosphamide 500 mg/m2 intravenously every 3 weeks, 6 courses |
| Taxanes | Paclitaxel – 135 mg/m2 / 24 h, cisplatin 75 mg/ m2 intravenously every 3 weeks, 6 courses |
Most drugs have side effects associated with the suppression of bone marrow hematopoiesis and the development of leukopenia, thrombocytopenia, the maximum severity of which occurs by the end of the 2nd week after the course. In this regard, it is necessary to monitor blood counts and stop treatment with antitumor drugs when the number of leukocytes falls below 3 x 10 6 /l and platelets - below 1 x 10 6 /l.
The patient's tolerance of the drugs and the severity of reactions that occur during their use are also of significant importance. In particular, the use of cyclophosphamide causes nausea, vomiting, alopecia, sometimes muscle and bone pain, headache, and in rare cases toxic hepatitis and cystitis.
At the stage of chemotherapy, it is necessary to strive to achieve complete regression of the disease (disappearance of all manifestations of the disease, normalization of the CA-125 level), and then consolidate the effect by conducting 2-3 additional courses. Upon achieving partial regression, chemotherapy should be continued until the moment when, during the last two courses of treatment, stabilization of the process is noted, assessed by the size of the residual tumor masses and the value of tumor markers. In these cases, the number of treatment courses for most patients ranges from 6 to 12, but not less than 6.
To determine the dose of chemotherapy drugs, the body area (in m2) is calculated . On average, with a height of 160 cm and a body weight of 60 kg, the body area is 1.6 m2 , with a height of 170 cm and a weight of 70 kg - 1.7 m2.
Currently, radiation therapy is not an independent method of treating patients with ovarian tumors and is recommended as one of the stages of combined treatment in the postoperative period. Postoperative radiation therapy is indicated for patients with clinical stages I and II, as well as at stage III after cytoreductive surgical interventions that reduce the volume of tumor masses in the abdominal cavity. Most often, distant gamma therapy is used on the abdominal cavity at a dose of 22.5-25 gray with additional irradiation of the small pelvis (up to 45 g). At these stages, postoperative irradiation is supplemented by "preventive" chemotherapy for 2-3 years. Radiation therapy of patients with malignant ovarian tumors of clinical stage IV remains an unsolved problem, since the presence of large tumor masses and (or) effusion in the serous cavities is considered a contraindication to radiation therapy. In such patients, the choice of additional treatment methods to surgery should be decided in favor of chemotherapy.
According to the International Federation of Obstetricians and Gynecologists (RGO), 5-year survival rates for all stages of ovarian cancer do not exceed 30-35%, 5-year survival at stage I is 60-70%; II - 40-50%; III - 10-15%; stage IV - 2-7%.
More information of the treatment
Drugs
Prevention
- Periodic examinations (2 times a year) using ultrasound of the pelvic organs (1 time per year) of women with risk factors for ovarian cancer: menstrual and reproductive dysfunction, uterine fibroids, benign ovarian cysts, chronic inflammatory diseases of the uterine appendages, etc.
- Correction of anovulation and ovulation hyperstimulation using steroid contraception (primary prevention of ovarian cancer).
- Modern diagnostics of benign and borderline ovarian tumors and their surgical treatment (secondary prevention of ovarian cancer).
Forecast
The 5-year survival rates (rounded to the nearest whole number) for epithelial ovarian cancer according to FIGO staging are as follows:
- Stage IA - 87%
- Stage IB - 71%
- Stage IC - 79%
- Stage IIA - 67%
- Stage IIB - 55%
- Stage IIC - 57%
- Stage IIIA - 41%
- Stage IIIB - 25%
- Stage IIIC - 23%
- Stage IV - 11%
Overall, survival is about 46%.


 [
[