Medical expert of the article
New publications
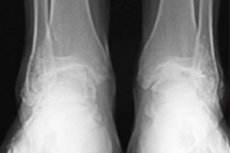
Osteoarthritis of the ankle.
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Disease of the joint articulating the bones of the lower leg and foot, associated with its dystrophic changes and bone and cartilage degeneration, is defined as osteoarthritis or osteoarthritis of the ankle joint.
Epidemiology
Aetiologically, ankle osteoarthritis is most often associated with trauma: according to statistics, up to 20% of all sports injuries affect this joint. According to some data, secondary post-traumatic ankle osteoarthritis accounts for 70-78% of cases and develops almost 10 years earlier than primary osteoarthritis.
Twelve percent of patients have osteoarthritis of rheumatoid etiology, and 7% have idiopathic primary osteoarthritis. [1]
Causes of the ankle osteoarthritis
In medicine, arthrosis (from the ancient Greek arthron - joint with suffix-os, indicating a pathological condition) is a pathology, the causes of which lie in the wear and tear of articular cartilage and the joints themselves, and thus distinguish its primary and secondary types or forms.
Primary bone and cartilage degeneration may develop in patients with systemic diseases that provoke cartilage matrix destruction: rheumatoid and juvenile idiopathic arthritis, polyarthritis, gout, osteoporosis, hereditary osteochondrodysplasia, and others. Such autoimmune diseases as scleroderma, systemic lupus erythematosus, recurrent polychondritis also negatively affect the condition of cartilage of the musculoskeletal system.
There is also a connection between osteoarthritis and thyroid gland dysfunction, because with the participation of thyroid hormones of this gland occurs the maturation of cartilage cells (chondrocytes) and the synthesis of cartilage tissue.
But secondary ankle osteoarthritis most often occurs after a serious injury to the ankle and is post-traumatic arthrosis ankle - the synovial hinge articulation of the distal ends of the tibia and fibula bones of the lower leg with the proximal end of the talus bone. [2]
His injuries could be in the form of:
- Joint ligament sprains with damage to the distal intertibial syndesmosis (a fibrous joint stabilizing the joint), resulting in joint instability and displacement of the articulating bones;
- Partial or complete tear of the ankle ligament;
- Fracture of the ankle joint, as well as the medial and lateral ankle (the epiphyses of the tibial epiphyses and the lower ends of the fibula adjacent to the articular surfaces of the talus).
For example, in many cases, ankle arthrosis is observed after a fracture of the distal metaepiphysis (lower rounded end) of the tibia near the ankle, as well as after a fracture of the talus.
In addition to trauma, osteochondral lesions of this joint can be caused by chronic overloading of the foot, congenital disturbance of its correct position, avascular necrosis in dissecting osteochondritis. In such cases, secondary deforming osteoarthritis of the ankle joint is diagnosed. [3]
Also read - what is osteoarthritis?
Risk factors
Risk factors for ankle arthrosis (osteoarthritis) identified in rheumatology are associated not only with trauma to the joint, including fractures, repeated sprains of its ligaments (especially in athletes), but also with congenital foot deformities: flatfoot (flat feet), cavus (high arch of the feet), cavovarus (high arch of the feet with the heel tilted inward) or equinovarus (clubfoot).
Biomechanical factors also include damage to the cartilage layer of the ankle bones due to overloading (e.g., due to overweight in obesity and metabolic syndrome) and impaired collagen fibers, which lose their proper elasticity - with increased stress on the cartilage and their gradual degeneration.
Biochemical factors include impaired synthesis of type II collagen, the main fibrillar protein of articular cartilage, by cartilage cells (chondroblasts), resulting in pathological changes in the articular membrane and the composition of synovial (intra-articular) fluid, which worsens the trophism of the joint and the condition of its bone structures. And, of course, genetic factors play a role here. [4]
Read more in the publications:
Pathogenesis
Osteoarthritis or osteoarthritis of the ankle joint usually results from damage to the articular cartilage, and the pathogenesis of theof cartilage degeneration is due to increased localized pressure in this joint, which has wide areas of contact at the ankle joint proper (articulatio talocruralis), subtalar joint (articulatio subtalaris), and lower tibiofibular joint (articulatio tibiofibularis). [5]
In this case, the cartilage becomes thinner and the cavity between the cartilaginous surfaces of the joint - the articular gap - narrows (with a decrease in synovial fluid and hyaluronic acid contained in it), which is accompanied by a decrease in the shock-absorbing ability of the cartilage extracellular matrix, which consists of chondrocytes, chondroitin sulfates (sulfated heteropolysaccharide), fibrils of several types of collagen, a number of proteins and other components. More details in the publication - osteoarthritis: how is articular cartilage organized?
In serious injuries of the articulatio talocruralis, the structure of articular cartilage and bone tissue changes; erosion of the articular surface with exposure of the subchondral bone begins; an inflammatory reaction occurs (with the production of enzymes causing further damage); inflammation of the inner (synovial) membrane of the articular bag develops - synovitis; deformation of the joint occurs due to the formation of osteophytes (bone growths) around it.
In cases of anatomical foot problems, the stability and biomechanics of the ankle joint are compromised: the articular cartilage is subjected to unilateral loading for many years, leading to its degeneration and damage to the underlying bony structures. [6]
Also read:
Symptoms of the ankle osteoarthritis
As noted by experts, pathological processes in this disease, as a rule, develop slowly, go through several stages and can give different severity of symptoms. And its first signs include swelling of the joint - swelling of soft tissues above the ankles (ankles). [7]
The condition of the articular cartilage and the extent of its degenerative changes are assessed using the Kellgren-Lawrence scale in ankle x-rays.
And it should be borne in mind that the initial ankle osteoarthritis, caused by primary bone and cartilage degeneration of cartilage - gradual softening of the cartilage matrix, in most patients runs latent. This is grade 1 ankle osteoarthritis.
Damage to the cartilage with the appearance of roughness and irregularities on its surface, as well as initial changes in the structure of cartilage tissue is considered as grade 2 ankle arthrosis. At this stage of the disease there may be periodic pain in the ankle and limitation of mobility. [8]
About pain in ankle arthrosis, which is localized along its anterior part, can be felt in the foot and lower leg and is felt at the first steps after a period of rest, and after prolonged load on the foot increases, more in the article - pain in the ankle joint.
The process progresses, and arthrosis of the 3rd degree - with frequent dull or stabbing pain, pronounced stiffness of the joint and crunch when walking, changes in gait with forced limping - is determined by the presence on the surface of articular cartilage deeper cracks and foci of its delamination and exposure of subchondral bone with the formation of bony outgrowths (osteophytes).
Extremely severe bone and cartilage pathology - with partial or complete loss of the ability to walk independently and severe pain (including at night) - is osteoarthritis of the 4th degree. At this stage, irreversible changes in articular cartilage are already present, and ulceration of unprotected bone surfaces is aggravated by the formation of cavities (subchondral pseudocysts with joint effusion) and an increase in marginal exostoses (bone overgrowths). [9]
More information in the material - main symptoms of osteoarthritis
Complications and consequences
The effects and complications caused by ankle osteoarthritis are expressed as:
- Deformity and instability of the joint with displacement of the articulating bones and progressive osteophytosis - formation of bone growths;
- Stiffness and limitation of joint mobility;
- Atrophy of the muscles associated with that joint;
- The development of arthritis of neighboring joints.
Therefore, walking with grade 3-4 ankle osteoarthritis is extremely difficult.
In adults, cartilage cells do not naturally regenerate, and progressive bone and cartilage degeneration is virtually irreversible.
Diagnostics of the ankle osteoarthritis
All details in the publication - clinical diagnosis of osteoarthritis
See laboratory diagnosis of osteoarthritis at.
Instrumental diagnosis includes various types of imaging and ankle arthroscopy. For more information see the article - instrumental Diagnosis of Osteoarthritis
In the course of radiologic diagnostics of osteoarthritis certain X-ray signs of this disease are detected, including narrowing of the joint gap, presence of osteophytes of the subchondral bone, deformity of the joint, foci of calcification (calcification) of the ligaments. [10]
Differential diagnosis
Differential diagnosis is made with ankle sprain/fracture, sprain and tear of its ligaments, tarsal syndrome, rheumatoid arthritis, inflammation of the Achilles tendon (tendinitis), ankle gout, plantar fasciitis.
It is important to differentiate between arthritis and arthrosis of the ankle joint: arthralgia in bone and cartilage degeneration of the ankle from the pain caused by rheumatoid suppurative or exudative arthritis (including subtalar arthritis). Achilles tendon bursitis, periarthritis, and synovial cysts (foot hygroma) should also be differentiated.
Who to contact?
Treatment of the ankle osteoarthritis
What does comprehensive treatment of osteoarthritis or ankle osteoarthritis include and what are its goals?
Conservative drug treatment is aimed at alleviating symptoms, slowing the progression of the disease, and preserving the joint and maintaining its function for as long as possible.
Read about which main medications are used in the publications:
Pain exhausts patients and reduces their quality of life, so the question they often ask is: how to relieve pain in ankle osteoarthritis?
The main painkillers for ankle osteoarthritis are Diacerein (Diamax, Diaflex, Flexerin, Arthroker), Paracetamol, Ibuprofen, Diclofenac and other NSAIDs. For more information see. - treatment of osteoarthritis: nonsteroidal anti-inflammatory drugs (NSAIDs)
Also read:
Topical, i.e. topical treatment of osteoarthritis is also performed - with the help of various ointments and gels that are applied to the painful area.
For a list of the best ointments for ankle osteoarthritis see:
In addition, ointments with chondroitin sulfate are used in the initial stages of osteoarthritis: chondroitin ointment, hondroflex or hondroxide. These remedies belong to the so-called chondroprotectors, that is, they inhibit the process of destruction of articular cartilage tissue. But they also have anti-inflammatory and analgesic effect, because they contain Dimethoxide (Dimethyl sulfoxide).
Many patients use chondroprotective products-nutroceuticals such as teraflex, Structum and ArthroMax (with sulfated chondroitin and glucosamine), or supplements containing these ingredients and various vitamins. Although the level of evidence of effectiveness of such products in foreign studies (analyzed in the Cochrane Database of Systematic Reviews) is recognized as average and below average, they help some people, especially with osteoarthritis of 1-2 degrees.
By the way, make intramuscular medication injections with solutions Artiflex Chondro, Chondrosat, Arteja, Hitart, etc., containing sodium chondroitin sulfate. More information - treatment of osteoarthritis: chondroprotectors
Intra-articular injection of systemic corticosteroids is practiced - injections of Diprospan (Betamethasone, Betaspan) into the ankle joint. As clinical experience shows, complex cases and exacerbation of ankle osteoarthritis require the use of drugs of this pharmacological group. In osteoarthritis of moderate and severe degree for short-term pain relief may require injections of corticosteroids into the joint. More information from the material - treatment of osteoarthritis: use of glucocorticosteroids [11]
Hyaluronic acid in the form of a gel-like solution of sodium hyaluronate (trade names of preparations - Gialgan, adant, Synvix, Sinocrom) is also used by intra-articular injections. And in some cases, adding hyaluronic acid to a joint affected by osteoarthritis can facilitate movement and reduce pain. [12]
In mild to moderate ankle osteoarthritis, physiotherapy treatment is prescribed to reduce periarticular swelling, improve microcirculation and control pain. Read more:
- Physiotherapy for osteoarthritis
- Physiotherapy for joint diseases
- Health resort treatment of osteoarthritis
In addition to electro and ultrasound procedures, mud and water therapy, massage for ankle osteoarthritis helps to improve tissue trophism, maintain range of motion and muscle strength. The Vitaphone device can be used at home for vibroacoustic massage.
Within therapeutic physical therapy for osteoarthritis there are exercises for the ankle joint in osteoarthritis that help strengthen the muscles of the foot and lower leg, for example, simple gymnastics for the ankle joint in osteoarthritis according to Evdokimenko - with alternating notion on the toes, with raising the toes (standing on the heels), rotations of the feet, etc.
For minor pain you can use kinesitherapy - treatment of ankle osteoarthritis according to Bubnovsky. Read the article - arthritis? Osteoarthritis? Positive prognosis!
Ankle joint support is an important part of conservative treatment, so supportive devices are used that can help strengthen or, if possible, preserve the joint. These are orthotic insoles or shoes for ankle osteoarthritis, ankle orthosis. Which can minimize joint pain when walking.
For the same purpose, fixation of the joint with elastic bandages - ankle taping - is used.
How are treatments carried out at home?
At home, take a pain relieving tablet internally, use appropriate ointments externally, do exercises. You can do foot baths with the addition of iodobromic sea salt, turpentine, table salt, with decoctions of birch leaf, willow bark or pine needles.
Can help relieve pain compresses on the joints with osteoarthritis of the ankle joint with a strong decoction of willow bark, ginger root juice, from fresh crushed leaves of nettle dicot; for compresses also use bischofite.
Attention should be paid to the diet, as the recommended diet for ankle osteoarthritis - joint Osteoarthritis Diet.
Surgical treatment
Surgical intervention may be indicated in severe osteoarthritis or when conservative therapy is ineffective. Possible options for surgical treatment:
- Arthroscopy of the ankle joint (with synovectomy, sanation, removal of free bodies, excision of osteophytes and cartilage plasty);
- Arthroscopic or open arthrodesis (rigid fixation of the joint) for post-traumatic and severe primary osteoarthritis;
- Osteotomy (during which the deformed joint is aligned to redistribute the load of the ankle joint);
- Tibial osteotomy (for osteoarthritis associated with foot or tibial deformity);
- Ankle joint endoprosthetics (arthroplasty).
Prevention
Recommended steps to prevent the development of ankle osteoarthritis include:
- Regular joint-sparing exercises (cycling, swimming);
- Normalization of body weight;
- Reducing the intake of animal proteins and fats;
- Treatment of diseases that increase the risk of bone and cartilage degeneration of joints.
Details in the material - prognosis and prevention of osteoarthritis
Forecast
Osteoarthritis (osteoarthritis), a degenerative, progressive joint disease, is not completely curable. Therefore, loss of ankle joint function and disability (resulting in limited walking ability, chronic pain, lower limb instability) are its long-term consequences, worsening the overall prognosis.

