Medical expert of the article
New publications
Dissecting osteochondritis.
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
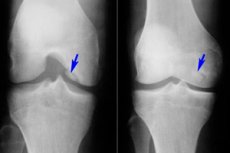
Among the many different diseases of the musculoskeletal system, osteochondritis dissecans is relatively rare - a disease that is a limited form of aseptic necrosis of the subchondral bone plate. The pathology is characterized by the separation of a small cartilaginous element from the bone and its displacement into the joint cavity.
Osteochondritis dissecans was first described in the 19th century by Dr. Paget, a British surgeon and pathologist. At that time, the disease was called "latent necrosis." The pathology acquired its current name of osteochondritis dissecans a little later, at the end of the same 19th century: this term was introduced by the German surgeon Franz Koenig.
The disease most often affects the knee joint, but can also develop in other joints, regardless of their size. [ 1 ]
Epidemiology
Osteochondritis dissecans occurs in only 1% of cases of joint diseases. The pathology is most often diagnosed in young men (mainly athletes), but can also occur in children. The ratio of affected men and women is 2:1. In approximately every fourth patient, the disease is bilateral.
Osteochondritis dissecans affects the internal condyle of the femur in 85% of cases, resulting in Koenig's disease. In 10% of cases, the external condyle is affected, and in 5%, the patella (Leuven's disease develops). [ 2 ]
The overall incidence of the pathology is 15-30 cases per hundred thousand population. [ 3 ] The average age range of those affected is 10-20 years. [ 4 ]
In childhood, the pathology proceeds more favorably: recovery occurs as a result of drug therapy. Adult patients often require surgical intervention.
Causes dissecting osteochondritis
The most common cause of osteochondritis dissecans is trauma, injury, excessive compression. With these effects, the blood supply to the tissues inside the joint deteriorates (ischemia). Such processes, in turn, cause gradual necrosis of the bone fragment, which eventually separates.
The exact causes of the disease are unknown. Experts believe that the pathology is the result of several factors at once. Thus, the most likely cause is trauma, direct or indirect damage to the joint. Additional factors may include:
- hereditary predisposition;
- genetic diseases;
- individual features of anatomy;
- metabolic disorders;
- abnormal maturation of the skeletal system.
Existing osteochondritis dissecans can be aggravated by further joint loads. In particular, people who actively engage in sports such as basketball or football, tennis, weightlifting, biathlon, shot put, gymnastics or wrestling suffer most from the pathology. The risk group also includes people whose professional activities are associated with the constant performance of the same type of repetitive movements that have an excessive effect on joint function. [ 5 ]
Risk factors
The origin of osteochondritis dissecans is currently not well understood. Among the factors that contribute to the emergence and development of the disease, the following can be distinguished:
- local necrotic processes in the subchondral bone plate;
- recurring joint injuries, including those of an exogenous nature (contusive injuries) and endogenous (impeachment syndrome, which develops with internal rotation of the joint, as well as habitual dislocations, chronic joint instability, old injuries);
- impaired enchondral ossification;
- endocrine diseases;
- genetic predisposition (anatomical defects of the joint structure, congenital anomalies of the subchondral layer, etc.);
- insufficient blood circulation, impaired trophism of bone and cartilage tissue, ischemic disorders;
- excessive regular stress on the joint.
Many authors suggest familial inheritance, even describing it as a mild form of skeletal dysplasia with associated short stature.[ 6 ],[ 7 ] However, challenging the evidence for familial inheritance, Petrie[ 8 ] reported a radiographic examination of first-degree relatives and found only 1.2% with acute osteochondritis dissecans.
Pathogenesis
The pathogenetic mechanism of osteochondritis dissecans development has not been sufficiently studied to date. There are several theories that are considered by specialists as the main ones. However, none of them has been officially confirmed yet. Nevertheless, let us consider them separately:
- Inflammatory process.
Some researchers have described inflammatory changes in the histological material of patients with osteochondritis dissecans. Detailed microscopic analysis revealed necrotic, non-specific, aseptic signs of inflammation, but in some biomaterials such changes were still absent. [ 9 ]
- Acute traumatic injury.
Cases of development of osteochondritis dissecans have been described as a consequence of chronic or acute trauma that caused ischemic processes with the formation of free bone-cartilaginous elements.
- Repeated injuries.
Repeated microdamage can become a provoking factor for the disease, which is especially typical for children. [ 10 ], [ 11 ]
- Genetic predisposition.
There is evidence of a hereditary predisposition to the development of joint pathologies. In particular, some patients had anatomical features that contributed to the emergence of this problem. [ 12 ]
- Ischemic processes.
The theory of involvement of ischemia or deterioration of vascular trophism in the affected area has existed for a long time. Many cases indicated a deficiency of the vascular network, weak arterial branching in the area of pathology. [ 13 ], [ 14 ]
Currently, osteochondritis dissecans is considered an acquired lesion of the subchondral bone, characterized by varying degrees of resorption and sequestration of bone tissue with possible involvement of articular cartilage through detachment, not associated with an acute osteochondral fracture of normal cartilage. [ 15 ]
Symptoms dissecting osteochondritis
Clinical symptoms of osteochondritis dissecans are non-specific and may differ in different patients. Children and adolescents often complain of diffuse pain in the affected joint: inconstant, sometimes intermittent, acute, accompanied by blocking of movement in the joint and its swelling.
In case of instability of the separated element, instability, blocking and crunching are observed. During examination, the load limitation on the affected joint is noticeable. Palpation is accompanied by pain. A long-term disease can manifest itself in atrophic changes of the leading muscles.
The first signs of osteochondritis dissecans in adults and children are practically the same: usually it is a slight aching pain or discomfort, which increases with motor activity and joint load. As the pathology progresses, the pain syndrome increases, the joint becomes swollen, and palpation pain appears.
After the detachment of the necrotic fragment, complaints of regular crunching and the appearance of motor "jamming" appear, which is explained by the appearance of an obstacle during the movement of the joint surfaces. Blockages may occur - the so-called joint "jamming", which manifests itself as acute pain and the inability to perform the intended movement.
The pathology can grow and worsen over several years – 2, 3, and sometimes ten or more. The main symptoms can be:
- pain (aching or sharp); 80% of patients typically experience mild pain for an average of 14 months and mild or mild claudication after physical activity [ 16 ]
- edema;
- motor crunching;
- limitation of motor ability;
- joint locking;
- increasing lameness (with damage to the joints of the lower extremities);
- muscular atrophic processes.
Osteochondritis dissecans in children
The causes of osteochondritis dissecans in childhood are also unclear. However, the prognosis in young children is more optimistic than in adults.
The disease is most often registered in boys aged 10-15 years, but the disease can also affect 5-9 year old children. In most cases, the disorder smooths out as they grow older.
The main symptoms of a problem in a child:
- causeless pain (usually in the knee), which intensifies with physical activity;
- swelling and blockage of the joint.
These symptoms require urgent diagnostics – in particular, X-ray, MRI, CT.
A favorable course of osteochondritis dissecans is not a reason not to carry out treatment. To begin with, the doctor advises the patient to completely exclude physical activity on the affected limb. If the disease affects the lower limbs, the child is prescribed crutches, with which he walks for several months (usually up to six months). Physiotherapy and exercise therapy are additionally included.
If there is no improvement within the specified time, then only in this case is surgical intervention prescribed:
- arthroscopic mosaic chondroplasty;
- revascularizing osteoperforation.
Stages
Based on the information obtained during X-ray examinations, the following stages of the pathological process in osteochondritis dissecans are determined:
- Formation of a necrotic focus.
- Irreversible phase of limitation of the necrotic area, dissection.
- Incomplete separation of the necrotically limited element.
- Complete separation of the bone-cartilaginous element.
In addition to the above classification, stages are distinguished depending on the endoscopic picture of osteochondritis dissecans:
- Intactness of the hyaline cartilage; softness and swelling are detected upon palpation.
- The cartilage is separated and torn along the periphery of the necrotic focus.
- The necrotically altered element is partially separated.
- A niche-like crater is formed in the affected area, and free intra-articular elements are present.
Koenig's disease is divided into the following stages:
- The cartilage softens without damaging its integrity.
- Part of the cartilage is separated, stability is noted.
- The cartilage becomes necrotic and the continuity is disrupted.
- A free element is formed, localized in the formed defect or behind it.
Forms
The pathology of osteochondritis dissecans is divided into adult and juvenile (developing in children and adolescents).
Classification depending on the localization of the pathological process:
- Osteochondritis dissecans of the knee joint is a limited subchondral aseptic necrosis of the articular bone surface. The incidence of the disease is 18-30 cases per hundred thousand patients. The predominantly loaded cartilaginous area is affected, which is the lateral segment of the medial condyle of the femur, near the intercondylar notch (internal or external condyle, patella). Osteochondritis dissecans of the patella has the most unfavorable prognosis, since it is difficult to treat. Osteochondritis dissecans of the medial condyle of the femur is otherwise called Koenig's disease. [ 17 ], [ 18 ]
- Osteochondritis dissecans of the talus occurs in children aged 9-16 years and is an osteochondropathy of the talus, with aseptic necrosis and damage to the articular cartilage. Other names for the pathology are Diaz's disease, or osteochondritis dissecans of the ankle joint. The etiology of the disease is unknown. In the absence of treatment, gross defects of the articular cartilage are formed. [ 19 ]
- Osteochondritis dissecans of the shoulder joint is a lesion of the head of the humeral condyle in the central or anterolateral sections. The disease is rare, found mainly in adolescents; it is also called Panner's disease. Even rarer are cases of damage to the head of the radius, olecranon process and fossa. [ 20 ]
- Osteochondritis dissecans of the hip joint affects the head of the femur. The disease may have minimal clinical and radiological manifestations for a long time, but over time, changes in the configuration of the articular surfaces become pronounced, movements in the joint become painful or blocked. Most often, the pathology begins to develop in childhood.
Complications and consequences
The most unfavorable complication of osteochondritis dissecans is considered to be the development of deforming arthrosis with motor blocking of the joint and disruption of the axis of the affected limb.
The altered mechanical and biological component caused by aseptic necrosis of the bone plate and the appearance of free intra-articular elements leads to the formation of deforming arthrosis with damage to the hyaline cartilage. This complication is typical for osteochondritis dissecans of the knee joint, femur and tibia. The first signs of aggravation of the pathological process: increased pain, lameness (especially when walking down stairs). Joint blockages and a sensation of a foreign body inside the joint occur.
The progression of the pathology leads to the following consequences:
- development of contracture and the appearance of crepitus;
- curvature of the joint contours caused by disturbances in bone tissue and loss of cartilage, as well as muscle atrophy;
- narrowing of the joint space;
- the appearance of bone growths along the edges of the gap.
In the later stages of the disease, the patient loses the ability to fully straighten the limb in the affected joint, and as a result, the limb (especially the lower one) is deformed. Radiologically, deformation and sclerosis of the articular surfaces, subchondral necrosis, significant narrowing of the joint space, extensive bone growths, and free intra-articular fragments are noted.
Diagnostics dissecting osteochondritis
Diagnostic measures begin with questioning and examining the patient. Osteochondritis dissecans is characterized by complaints of pain, blocking in the joint, crunching and clicking, limited range of motion. The patient may indicate previous metabolic-dystrophic pathologies, injuries, intra-articular administration of medications.
During the examination, the doctor notes:
- joint blocking or severe limitation of movement;
- clicking, crepitation.
Joint pain and deformities are detected by palpation.
Laboratory tests are prescribed as part of a general and differential examination of the body:
- general clinical blood test with determination of leukocyte formula;
- determination of ESR;
- fibrinogen;
- antistreptolysin O;
- serum uric acid level;
- C-reactive protein (quantitative method);
- rheumatoid factor;
- antinuclear factor on HEp-2 cells;
- level of antibodies to extractable nuclear antigen.
Laboratory diagnostics are necessary to exclude arthritis, systemic autoimmune diseases, rheumatoid arthritis, Sjogren's syndrome, etc.
Instrumental diagnostics are represented, first of all, by magnetic resonance imaging. It has been experimentally proven that MRI is the most preferred method for diagnosing osteochondritis dissecans, as it allows one to assess the size of the lesion and the condition of the cartilage and subchondral plate, determine the extent of bone marrow edema (increases signal intensity), detect a free element in the joint, and track the dynamics of the pathological process. In addition, MRI helps to examine the condition of other joint structures: menisci, ligaments, synovial folds, etc. [ 21 ]
Ultrasound diagnostics and other methods of examination do not provide complete information about the disease. Conventional radiography and computed tomography are uninformative in the initial stages of osteochondritis dissecans (2-4 weeks). These methods can only be used to clarify some points after MRI.
Differential diagnosis
Pathology |
Main differences from osteochondritis dissecans |
Deforming osteoarthritis |
Osteophytes and ossified areas of ligaments often appear as intra-articular free elements. However, they are usually irregular in shape and have sharp edges. There is also no condyle defect. |
Chondromatosis |
There is no characteristic crater in the epiphysis of the tibia or femur. The chondromous bodies are bean-shaped, their number reaches or even exceeds 10. |
Lipoarthritis (Hoffa's disease) |
There is a structural change in the infrapatellar or suprapatellar lipid body, which is compacted and can provoke signs of strangulation. X-ray and magnetic resonance methods allow differential diagnostics. |
Fracture within the joint |
The intra-articular separated element of traumatic origin has an irregular shape, uneven outlines. There is no characteristic crater. |
Misinterpretation without joint pathology |
In some cases, inexperienced specialists mistake the sesamoid bone of the gastrocnemius tendon for an intra-articular separated fragment. The characteristic crater of the lateral condyle of the femur is sometimes mistaken for a subchondral lumen, one of the variants of the normal anatomical structure of the joint. |
Treatment dissecting osteochondritis
Treatment is aimed at improving the trophism of the bone-cartilaginous elements and fixing the separated parts. Arthroscopy is used to visualize the location and extent of the damage and determine the degree of detachment. If the effectiveness of conservative treatment is initially questioned, surgical intervention is prescribed.
Osteochondritis dissecans, which is accompanied by characteristic symptoms but does not have an obvious rupture of the bone-cartilaginous element, is treated using the osteochondroperforative method, using Kirschner wires.
Conservative treatment is applicable only in the initial stages of osteochondritis dissecans. Physiotherapeutic treatment is practiced against the background of unloading the affected joint for up to one and a half years. During this time, the patient is completely prohibited from playing sports. The patient uses crutches to walk, excluding the load on the affected limb. After the pain subsides, therapeutic exercise is prescribed, which involves non-strengthening exercises, to prevent muscle atrophy. [ 22 ]
Medicines
If an intra-articular inflammatory process is detected, antibiotic therapy is prescribed. The most likely ones are Cefazolien or Gentamicin. Vancomycin is suitable when Methicillin-resistant Staphylococcus aureus is detected.
Nonsteroidal anti-inflammatory drugs are used for pain relief. If the patient has contraindications to taking such drugs (ulcer, gastric bleeding), then Paracetamol becomes the drug of choice. In case of severe pain, opioid analgesics may be indicated.
Antibiotics |
|
Cefazolin |
The average daily dosage is 1-4 g, in the form of intravenous or intramuscular injections. The drug is not used in case of hypersensitivity to cephalosporin and beta-lactam antibiotics. |
Gentamicin |
The standard daily dosage of the drug is 3 mg/kg of weight intramuscularly or intravenously in 2-3 injections. Duration of therapy is 7 days. The drug has ototoxicity. |
Vancomycin |
Prescribed individually, taking into account therapeutic indications. Administered intravenously by drip. Rapid administration can provoke a number of side effects, including anaphylactic shock, shortness of breath, heart failure. |
Opioid pain relievers |
|
Tramadol |
A single dose of the drug (intravenous or oral) is 50-100 mg. The maximum possible daily dose of the drug is 400 mg. The treatment period is 1-3 days. |
Trimeperidine |
It is administered intramuscularly, intravenously in the form of a 1% solution, in the amount of 1 ml per day. Duration of use is 1-3 days. |
Nonsteroidal anti-inflammatory drugs |
|
Ketoprofen |
Taken orally at 200-300 mg per day in 2-3 doses, or administered intramuscularly at 100 mg 1-2 times per day. Possible side effects: dyspepsia, gastritis, skin rashes. |
Ketorolac |
A single dose of the drug is 10 mg. The maximum daily dosage is 40 mg. The duration of the course cannot exceed 5 days. Intramuscular or intravenous administration in minimally effective doses is also possible. Possible side effects: abdominal pain, diarrhea, stomatitis, cholestasis, headache. |
Paracetamol |
Prescribed at 0.5-1 g up to 4 times a day, for 3-5 days. The drug is well tolerated and rarely causes side effects. Exception: allergy to Paracetamol. |
Physiotherapy treatment
Physiotherapy is most often used at the rehabilitation stage after surgery for osteochondritis dissecans. Preference is given to the following procedures:
- local cryotherapy (a course of treatment includes up to 10 procedures);
- UFO therapy (course duration – 10 days, one procedure daily);
- magnetic therapy (a course of treatment includes from five to ten sessions);
- UHF therapy (7-10 sessions);
- laser therapy (daily for 1 week).
To improve blood circulation in the affected joint and to prevent muscle atrophy, special exercise therapy exercises are prescribed:
- Muscle tension with a gradual increase in intensity, lasting 6 seconds, with a number of repetitions of about 10 per approach.
- Repeated flexion and extension of the fingers of the limb, exercises to train peripheral circulation (lowering and raising the limbs).
- Exercises for the prevention of joint stiffness (up to 14 movements per approach).
It is possible to use mud therapy and water therapy, at the discretion of the attending physician.
Herbal treatment
Osteochondritis dissecans in adults is a dynamically unfavorable pathology, which in the absence of competent treatment can lead to disability. Therefore, the sooner measures are taken to combat the disease, the better.
Treatment for osteochondritis dissecans should be comprehensive. If the attending physician does not object, some folk methods can be used, in particular, herbal medicine.
- Grate the horseradish root, heat it slightly until it is warm, put it on a cloth and apply it as a compress to the affected area. Repeat the procedure every other day.
- Prepare a herbal mixture of 1 teaspoon of birch leaves, the same amount of nettle and dandelion leaves, marigold flowers and willow rhizomes. Pour 1 liter of boiling water over the mixture and leave it under the lid for 10 hours. Drink half a glass of the remedy three times a day half an hour before meals. The treatment period is 8 weeks.
- Prepare a mixture based on equal amounts of wild rosemary, hop cones, chamomile flowers and St. John's wort. Then take 2 tbsp of the mixture, pour 1 liter of boiling water, leave under the lid for about 10 hours, take half a glass 4 times a day before meals.
- Prepare a mixture of 1 teaspoon of raspberry stems, the same amount of elecampane and nettle leaves, 1 tablespoon of wild rosemary and 1 teaspoon of elderberry flowers. Add 0.5 liters of boiling water to the mixture and leave under a lid for 15-20 minutes. Filter and take 100 ml three times a day before meals. Duration of use: up to three months.
- Pour 500 ml of boiling water over 2 tbsp of lingonberry leaves and leave for 40 minutes. Take 100-150 ml three times a day before meals.
Rubbing the affected joint with elecampane tincture gives a good effect (50 g of rhizome is poured with 150 ml of vodka and kept in a dark place for 2 weeks).
Surgical treatment
Some authors [ 23 ], [ 24 ] believe that conservative treatment should be the first line of treatment for stable lesions in children. The only consensus regarding this method is that if this treatment is chosen, its duration should be 3 to 6 months before choosing surgical treatment. [ 25 ]
Surgery is usually indicated for unstable and stable lesions of acute osteochondritis dissecans that are not amenable to conservative treatment. [ 26 ], [ 27 ]
Differences in surgeon preferences for surgical treatment are reflected in the variety of surgical techniques. These include drilling (both retrograde and antegrade), [ 28 ], [ 29 ] bone grafting, [ 30 ], [ 31 ] fixation, [ 32 ], [ 33 ] alignment procedures, [ 34 ] and debridement. [ 35 ]
Osteochondritis dissecans, detected in an adult patient, often becomes an indication for surgical intervention. At the initial stage of the pathology development, the dead area is replaced by newly formed tissue, and at subsequent stages, free fragments are removed by arthrotomy.
The scale of the intervention is determined after performing magnetic resonance imaging and arthroscopy. As a rule, while maintaining contact of the free element with the surrounding tissue, the separated bone-cartilaginous fragment is drilled and replaced with living tissue. A Kirschner wire or a thin awl is used for tunneling. The wire is placed in the center of the necrotic zone, perpendicular to the joint surface. The intervention is completed by resection of the cartilaginous area and treatment of its edges.
If the OCD lesion is fragmented or cannot be fixed due to cartilage quality or mismatch, the fragment should be excised, the donor site removed, and the defect repaired based on individual findings.[ 36 ] Excision of the fragment may provide short-term pain relief.[ 37 ],[ 38 ]
If the free element has pronounced mobility, it is first fixed with a clamp. Then the connecting transition (bone or cartilage) is cut, after which the element is removed. Channels are drilled in the subchondral plate, the edges are processed. The joint is washed, sutures and an aseptic bandage are applied.
After refixation of the free element, the spokes are removed approximately 2-2.5 months later. In the postoperative period, the patient is prescribed antibiotic therapy and symptomatic drugs.
A new, modern technique of arthroplasty is autogenous chondrocyte transplantation. The method involves culturing and transplanting cells, but due to the high cost of the procedure, its practice is currently limited. [ 39 ], [ 40 ]
Most authors report that the time to radiographic healing ranges from 6 weeks to 2 years.
Prevention
Since the etiology of osteochondritis dissecans is not fully understood, there is no specific prevention of the disease yet. However, doctors still give a number of recommendations to prevent the development of such diseases. Such recommendations are of a primary and secondary nature.
Primary prevention consists of general maintenance of the health of the musculoskeletal system:
- fight against excess weight;
- regular moderate physical activity;
- injury prevention, wearing comfortable and high-quality shoes;
- practice of general strengthening measures;
- avoiding hypothermia, timely treatment of any pathologies in the body.
Secondary prevention involves preventing the worsening of existing osteochondritis dissecans. The main preventive points are considered to be the following:
- limitation of joint load;
- refusal from such sports as running, track and field, weightlifting, gymnastics, basketball, volleyball, football;
- correction of professional characteristics, avoidance of prolonged standing, frequent squatting, regular walking up and down stairs;
- reviewing your diet, avoiding starvation, avoiding fatty and monotonous foods, ensuring the body receives essential microelements and vitamins.
Exercise therapy should only be performed under the supervision of a doctor. Correct exercises should not burden the musculoskeletal system, but restore the strength and elasticity of joints, accelerate blood circulation and improve metabolic processes.
On the recommendation of a doctor, you can practice massage sessions for different muscle groups.
Forecast
Osteochondritis dissecans is a challenging orthopaedic problem because it is difficult to both identify and treat, even though new developments have emerged in this area.
The prognosis of the disease may depend on the type of treatment used (medicinal, surgical), on the maturity of the growth zones, on the localization, stability and size of the separated element, on the integrity of the cartilage. In childhood, the outcome of the disease is mostly favorable: osteochondritis dissecans responds well to treatment in children. In adulthood, early diagnosis of the pathology is important, which directly affects the long-term prognosis. The most unfavorable outcome is observed in patients with complications, as well as with pathology of the lateral condyle of the femur.

