Medical expert of the article
New publications
Bacterial vaginosis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Bacterial vaginosis is a disease that occurs as a result of a complex disorder of the vaginal microflora, in which the number of lactobacilli decreases and anaerobic infectious agents predominate. The following symptoms are characteristic: gray, scanty, foul-smelling vaginal discharge and itching. Diagnosis is based on clinical data and examination of vaginal secretions. Treatment is carried out using oral metronidazole or its combination with topical clindamycin.
 [ 1 ]
[ 1 ]
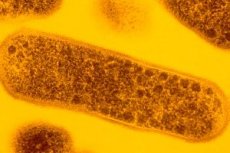
Causes bacterial vaginosis
Bacterial vaginosis is a non-specific infectious lesion of the vagina, the cause of which is unknown. The disease is caused by anaerobic infectious agents such as Prevotella spp., Peptostreptococcus spp., Gardnerella vaginalis, Mobiluncus spp., Mycoplsma hominis, the concentrations of which increase 10-100 times and lead to a decrease in lactobacilli. Risk factors include factors characteristic of sexually transmitted diseases. Bacterial vaginosis can occur in virgins. Treatment of the sexual partner is necessary to prevent recurrence of the disease in sexually active women. The use of intrauterine contraceptives is also a risk factor.
Previously, bacterial vaginosis was considered unimportant. Currently, it is believed that bacterial vaginosis increases the risk of developing pelvic inflammatory diseases, contributes to the growth of endometritis after abortion or childbirth, vaginal infection after hysterectomy, chorioamnionitis, premature rupture of the membranes of the fetal bladder, premature birth.
Pathogens
Pathogenesis
Bacterial vaginosis is caused by an imbalance of vaginal microflora with a reduction in lactobacilli. Bacterial vaginosis microbiota have been found on the coronary sulcus of the penis, the male urethra. Uncircumcised partners may act as a "reservoir" increasing the likelihood of infection after intercourse. Another mechanism of transmission is contact, skin-to-skin.
Symptoms bacterial vaginosis
Vaginal discharge is foul-smelling, grey, liquid, profuse. Discharge usually has a fishy odor, increases, becomes abundant and alkaline, after intercourse and menstruation. The most common symptoms are itching and irritation. Hyperemia and edema are less common.
The leading and most common symptoms of bacterial vaginosis are complaints of profuse leucorrhoea with an unpleasant odor. At the onset of the disease, the leucorrhoea has a liquid consistency, white or grayish in color. With a long course of the disease, it acquires a yellowish-green color. It becomes thicker, often resembling a curdled mass. It has the property of foaming, is slightly viscous, sticky, and is evenly distributed on the walls of the vagina. The amount of leucorrhoea is on average about 20 ml per day (approximately 10 times higher than normal). Some patients note local discomfort, itching and burning in the vulva, and dyspareunia. During an objective examination, it is necessary to pay attention to the condition of the external genitalia, the external opening of the urethra, the mucous membrane of the vagina, the cervix, and the nature of the discharge. A characteristic feature of bacterial vaginosis is the absence of signs of inflammation (edema, hyperemia) of the vaginal walls. The mucous membrane is of normal pink color. The colposcopic picture is characterized by the presence of dystrophic changes.
Where does it hurt?
What's bothering you?
Complications and consequences
The development of endometritis, salpingitis, chorioamnionitis, cervicitis and pelvic inflammatory diseases is possible, especially after invasive gynecological procedures.
In pregnant women, as a result of ascending infection, infection of the fetal membranes and amniotic fluid is possible, which may result in spontaneous abortions and premature births. The fetus can be infected both antenatally and intranatally. If there are complications of pregnancy in the anamnesis (premature rupture of membranes, low birth weight fetus, stillbirth, endometritis, premature birth, prematurity), it is advisable to conduct a study at 12-16 weeks to diagnose bacterial vaginosis.
Diagnostics bacterial vaginosis
Three of four criteria must be present for diagnosis: gray discharge, vaginal pH greater than 4.5, fishy odor, and clue cells. Clue cells are identified microscopically on a saline slide (bacteria adsorb to epithelial cells and obscure their edges). If leukocytes are found on a saline-fixed slide, a concomitant infection such as trichomonas, gonorrhea, or chlamydial cervicitis may be present and will require further investigation.
The diagnosis of bacterial vaginosis can be made based on clinical criteria or Gram stain. Clinical criteria are defined by the presence of at least three of the following symptoms or signs:
- Homogeneous, white discharge adhered to the vaginal walls in the absence of signs of inflammation;
- Presence of key cells on microscopic examination;
- pH of vaginal fluid > 4.5;
- Fishy odor of vaginal discharge before or after adding 10% KOH solution.
When a Gram-stained smear is examined, determination of the relative concentration of bacterial morphotypes characterizing the change in microflora is an acceptable laboratory method for diagnosing bacterial vaginosis. Culture of Gardnerella vaginalis for the diagnosis of bacterial vaginosis is not recommended, since it is not specific.
Physical examination for bacterial vaginosis
When examined in a mirror, there is abundant discharge in the absence of signs of vaginal inflammation.
 [ 25 ], [ 26 ], [ 27 ], [ 28 ]
[ 25 ], [ 26 ], [ 27 ], [ 28 ]
Laboratory methods for studying bacterial vaginosis
- Microscopic methods are the main ones. Wet (native) preparations of secretions taken from the anterior vaginal wall and from the posterior fornix are subjected to microscopy, and a smear is made for staining with methylene blue. The following indicators are characteristic of a vaginal smear in bacterial vaginosis:
- absence of leukocytes in the smear or a scanty number of them;
- absence of lactobacilli or their insignificant amount;
- a large number of bacteria covering the entire field of vision: small coccobacilli, cocci, vibrios;
- the presence of “key” cells - cells of the flat vaginal epithelium, covered with many bacteria due to direct adhesion to the cell surface, as well as “superadhesion” to adhered microbial cells.
- Cultural diagnostics are not used.
The most informative laboratory method for diagnosing bacterial vaginosis is the detection of clue cells (descended vaginal epithelial cells covered with small gram-negative rods) in Gram-stained smears. This indicator is detected in 94.2% of patients, while it is not determined in healthy women. The appearance of clue cells in bacterial vaginosis can be associated with dystrophic changes in the vaginal mucosa, increased epithelial desquamation and increased adhesion of gram-negative microorganisms to these cells. pH-metry and aminotest are of great importance in diagnosing bacterial vaginosis. They are screening methods and can be used directly during an outpatient appointment. In patients, the vaginal pH is always between 5.0 and 7.5. The aminotest is positive in 83.1% of cases (appearance or intensification of the unpleasant smell of rotten fish - isonitrile when mixing equal amounts of vaginal contents and a 10% solution of potassium hydroxide).
What do need to examine?
What tests are needed?
Who to contact?
Treatment bacterial vaginosis
Metronidazole vaginal gel 0.75% for 5 days or clindamycin vaginal cream 2% once daily for 7 days is prescribed. Metronidazole is given orally at a dose of 500 mg twice daily for 7 days or 2 g orally as a single dose. However, systemic adverse effects may occur. Women who use clindamycin cream cannot use latex devices (such as condoms or diaphragms) for contraception because the drug weakens latex. No treatment is required for asymptomatic sexual partners. Metronidazole vaginal gel is necessary for vaginosis during the first trimester of pregnancy; although metronidazole is used throughout pregnancy, it has not been shown to reduce the risk of pregnancy complications. Metronidazole can be prescribed prophylactically before abortion to all patients or only to those whose vaginal secretion examination reveals positive criteria characteristic of bacterial vaginosis.
The doctor's procedure when diagnosed with bacterial vaginosis
- Patient's message about diagnosis.
- Providing information about sexual behavior during treatment.
- Collection of sexual anamnesis.
- Discusses with the patient the possibility and necessity of testing for other STIs. Hepatitis B vaccination is recommended.
- Identification of predisposing factors and their elimination.
- If there are no results from treatment, the following possible reasons should be considered:
- false positive test result;
- non-compliance with treatment regimen, inadequate therapy;
- the presence of other predisposing and supporting factors.
A two-stage treatment method is used, the main principle of which is to create optimal physiological conditions for the vaginal environment and restore the microbiocenosis. At the first stage of treatment, local antibacterial therapy is carried out (metronidazole, clindamycin, chloramphenicol, etc.), lactic acid is prescribed to reduce pH, laser therapy, immunocorrectors, estrogens, prostaglandin inhibitors and antihistamines according to indications. In the presence of itching, burning, pain, local anesthetics are used. The second stage involves the use of bacterial biological preparations: lactobacterin, acylact, bifidumbacterin, bifidin locally to restore the vaginal microflora. Prescribing these drugs without the preliminary first stage is futile due to the pronounced competition between vaginal microorganisms. In essence, the introduction of live cultures of lactic acid bacteria into the vagina is a “transplantation” of these microorganisms, and their “survival” largely depends on the state of local immunity, endocrine status and the presence of risk factors.
The principal goal of therapy is to relieve vaginal symptoms and signs. Therefore, all women (non-pregnant and pregnant) who have symptoms should be treated. Bacterial vaginosis during pregnancy is associated with adverse pregnancy outcomes, and some studies suggest that treatment of pregnant women with bacterial vaginosis and those at high risk for preterm birth (i.e., those with a history of preterm birth) may reduce the incidence of preterm birth. Therefore, it is reasonable to consider whether asymptomatic pregnant women at high risk should be treated. Some authorities recommend treating bacterial vaginosis in high-risk pregnant women, while others believe that more clinical trial data are needed. Large randomized trials of treatment for bacterial vaginosis in asymptomatic women are underway to determine the benefits of treating bacterial vaginosis in low- and high-risk pregnant women.
Many of the bacterial flora that characterize bacterial vaginosis are isolated from the endometrium or fallopian tubes of women with PID. Bacterial vaginosis has been associated with endometritis, PID, or vaginal cellulitis following invasive procedures such as endometrial biopsy, hysterectomy, hysterosalpingography, intrauterine contraceptive device insertion, cesarean section, or curettage. Results of one randomized controlled trial showed that treatment of bacterial vaginosis with metronidazole significantly reduced the incidence of postabortion PID. Based on these data, it may be reasonable to treat bacterial vaginosis (symptomatic or asymptomatic) before surgical abortion. However, further studies are needed to determine whether asymptomatic women with bacterial vaginosis should be treated before other invasive procedures.
Recommended Treatments for Bacterial Vaginosis in Non-Pregnant Women
Metronidazole 500 mg orally 2 times daily for 7 days.
- or Clindamycin cream, 2%, one full applicator (5g) intravaginally at night - for 7 days,
- or Metronidazole gel, 0.75%, one full applicator (5g) intravaginally - once or twice a day, for 5 days.
NOTE: Patients should be advised to avoid drinking alcohol during treatment with metronidazole and for 24 hours after treatment. Clindamycin cream is oil-based and may damage latex condoms and diaphragms. Consult condom labeling companies for more information.
Alternative Treatments for Bacterial Vaginosis
Metronidazole 2 g orally once or Clindamycin 300 mg orally twice daily for 7 days.
Treatment with metronidazole, given as a single dose of 2 g, is an alternative regimen due to its lower efficacy in the treatment of bacterial vaginosis.
Oral metronidazole (500 mg twice daily, every day) has been shown in numerous studies to be effective in the treatment of bacterial vaginosis, causing resolution of symptoms, improvement in clinical status, and dysbiosis. In an efficacy study in four randomized controlled trials, overall cure rates at 4 weeks after completion of treatment were not significantly different between a 7-day regimen of oral metronidazole and clindamycin vaginal cream (78% and 82%, respectively). Randomized controlled trials also showed that there was no significant difference in cure rates between a 7-day regimen of oral metronidazole and metronidazole vaginal gel after 7 days of treatment (84% and 75%, respectively). The FDA has approved the use of Flagyl ER TM (750 mg) once daily for 7 days for the treatment of bacterial vaginosis.
Some health care professionals remain concerned about the potential teratogenicity of metronidazole, which has been demonstrated in animal studies using very high doses and long courses of treatment. However, a recent meta-analysis found no evidence of teratogenicity in humans. Some health care professionals prefer the intravaginal route of administration because it does not carry the risk of systemic side effects (eg, gastrointestinal effects are generally mild to moderate; the drug has an unpleasant taste). The mean peak serum concentration of metronidazole is 2% lower with intravaginal administration than with standard 500 mg oral doses, and the mean bioavailability of clindamycin cream is approximately 4%).
 [ 29 ], [ 30 ], [ 31 ], [ 32 ]
[ 29 ], [ 30 ], [ 31 ], [ 32 ]
Further observation
If symptoms resolve, there is no need for further monitoring. Recurrence of bacterial vaginosis is common. Because treatment of bacterial vaginosis in asymptomatic high-risk pregnant women may prevent adverse pregnancy outcomes, a follow-up examination at one month after treatment is recommended to assess cure. Alternative regimens may be used to treat recurrences. There is currently no regimen using any drug for long-term maintenance therapy.
 [ 33 ], [ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ], [ 39 ], [ 40 ]
[ 33 ], [ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ], [ 39 ], [ 40 ]
Management of sexual partners with bacterial vaginosis
Clinical trials have shown that treatment of sexual partners does not affect the effectiveness of the woman's treatment or the recurrence rate, therefore routine treatment of sexual partners is not recommended.
Bacterial vaginosis and associated diseases
 [ 41 ], [ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ]
[ 41 ], [ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ]
Allergy or intolerance
In patients with allergy or intolerance to metronidazole, clindamycin cream should be preferred. Metronidazole gel can be used in patients who are intolerant to systemic metronidazole, but patients with an allergy to oral metronidazole should not use it intravaginally.
Pregnancy and bacterial vaginosis
Bacterial vaginosis is associated with adverse pregnancy outcomes (early rupture of membranes, prematurity, and preterm birth), and organisms found in elevated concentrations in bacterial vaginosis are often isolated in postpartum or postcesarean section endometritis. Because treatment of bacterial vaginosis in asymptomatic high-risk pregnant women (history of preterm birth) may reduce the risk of preterm birth, such pregnant women should be evaluated and, if bacterial vaginosis is identified, treated. Screening and treatment should be initiated early in the second trimester. The recommended regimen is metronidazole 250 mg orally 3 times daily for 7 days. Alternative regimens include metronidazole 2 g orally as a single dose or clindamycin 300 mg orally 2 times daily for 7 days.
Low-risk pregnant women (women with no history of preterm birth) with symptoms of bacterial vaginosis should be treated until symptoms resolve. The recommended regimen is metronidazole 250 mg orally 3 times daily for 7 days. Alternative regimens include metronidazole 2 g orally as a single dose or clindamycin 300 mg orally 2 times daily for 7 days or metronidazole gel, 0.75%, one applicator full (5 g) intravaginally 2 times daily for 5 days. Some experts prefer systemic therapy for low-risk women in the treatment of possible upper reproductive tract infections with subclinical manifestations.
Lower doses of the drugs during pregnancy are recommended because of the desire to limit fetal exposure to the drugs. There are limited data on the use of metronidazole vaginal gel during pregnancy. Clindamycin vaginal cream is not recommended for use during pregnancy because two randomized trials showed an increased rate of preterm birth after treatment with clindamycin vaginal cream.
HIV infection
People with HIV infection and bacterial vaginosis should receive the same treatment as patients without HIV infection.
More information of the treatment
Forecast
Bacterial vaginosis usually has a favorable prognosis. With inadequate therapy, complications may develop.

