Anal fissure
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Anal fissure ranks second in frequency among diseases of the rectum, occurs in 60% of cases in women.
Anal fissure (rectal fissure, anal ulcer) is an acute longitudinal rupture or chronic, ovoid form of the ulcer of the flat epithelium of the anal canal. It causes severe pain, sometimes with bleeding, especially when defecating. The diagnosis is established upon examination. Treatment of anal fissure is in local hygiene, the use of stool softeners and, occasionally, injections of botulinum toxin.
What causes an anal fissure?
An anal fissure is believed to develop due to damage to the anal canal with a hard or copious stool with the development of a secondary infection. Injuries (eg, anal sex) are a rare cause. Anal fissure can cause spasm of internal sphincter, which in turn disrupts blood supply and creates conditions for chronic flow.
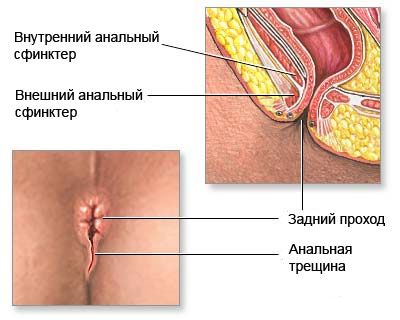
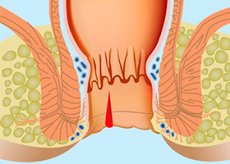
Anus fracture is a defect in the wall of the anal canal of a linear or triangular shape 1 to 1.5 cm in length, located near the transitional fold above the Hilton line. The origin of the fissure is associated with many causes, but the most important factor is the trauma of the mucous membrane of the anal canal by calves, foreign bodies, damage to it during childbirth. A predisposing factor may be hemorrhoids. Acute anal fissure has a slit shape, smooth even edges, the bottom of it is the muscular tissue of the sphincter.
With a long course of the pathological process, the connective tissue grows along the edges of the crack, its bottom is covered with granulations and fibrous plaque. In the region of the outer edge of the crack, excess tissue forms the anal (guard) tubercle. Thus, the acute anal fissure turns into a chronic fissure, which in fact is an ulcer with cicatricial margins and a scar's bottom. Sometimes an acute anal fissure disappears on its own, but more often than not, it changes into a chronic one. As a rule, there is only one crack and more often it is located on the back, closer to the coccyx, the wall of the anal canal. Occasionally there are 2 cracks on the back and front walls, which are one above the other. It is necessary to distinguish the true cracks from various surface damages of the perianal skin.
Symptoms of anal fissure
Anal fissure, as a rule, is located on the back wall along the middle line, but sometimes it can also appear on the front wall. Cracks located away from the midline may have a specific etiology, especially Crohn's disease. In the outer end of the fracture, the dermal papilloma (borderline tubercle) can be located, and in its upper corner there may be an enlarged (hypertrophied) hairy papilla.
Acute cracks can be observed in infants, but chronic cracks are rare. Chronic fractures must be differentiated from cancer, primary lesions of syphilis, tuberculosis and ulceration in Crohn's disease.
Cracks cause pain in the anus and bleeding. Pain usually occurs during or after a bowel movement, lasts for several hours and disappears until the next bowel movement.
Where does it hurt?
What's bothering you?
What do need to examine?
How to examine?
Who to contact?
Treatment of anal fissure
Anal fissure often enough yields to conservative treatment, aimed at minimizing trauma during defecation (eg, softeners, stool, psyllium, fiber). Zazhivaniya helps the application of protective ointments based on zinc oxide or soothing suppositories (eg, glycerol), which lubricate the anal canal and facilitate the stool.
Temporary effect is provided by local anesthetics (eg, benzocaine, xichain) and warm (not hot) sedentary baths for 10 or 15 minutes after each defecation and if necessary.
Effective 0.2% nitroglycerin ointment, 0.2% or 0.3% nifedipine cream, arginine gel and injections of botulinus toxin into the internal sphincter, which relax the anal sphincter and reduce the maximal anal rest pressure, creating conditions for healing. If the conservative treatment is ineffective, surgical treatment of the anal fissure (internal anal sphincterotomy and dosed anus enlargement) is shown, which allows eliminating the spasm of the internal anal sphincter.
More information of the treatment


 [
[