Medical expert of the article
New publications
Crohn's disease
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Crohn's disease is a chronic transmural inflammatory disease of the gastrointestinal tract that typically affects the distal ileum and colon, but can develop at any level of the gastrointestinal tract. Symptoms include diarrhea and abdominal pain. Abscesses, internal and external fistulas, and intestinal obstruction may develop.
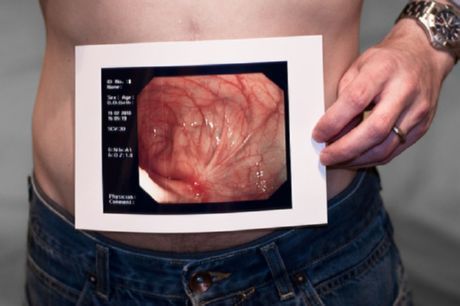
Crohn's disease - bowel pathology
Since this disease can be localized in any part of the gastrointestinal tract, there is a certain classification to differentiate the forms of the disease. Thus, with ileocolitis, the ileum and colon are mainly affected. With the gastroduodenal form - the stomach and duodenum. With ileitis, the ileum is affected. With jejunoileitis, the small intestine and ileum are damaged. With Crohn's disease of the colon, other parts of the gastrointestinal tract are not affected.
Extraintestinal symptoms, especially arthritis, may occur. The diagnosis of Crohn's disease is made by colonoscopy and barium contrast studies. Treatment consists of 5-ASA, glucocorticoids, immunomodulators, anticytokines, antibiotics, and often surgery.
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ]
ICD-10 code
ICD defines Crohn's disease as an inflammation of the gastrointestinal tract of unknown origin, which is characterized by damage to individual segments, a recurrent course, the appearance of ulcerative formations, which in some cases may be accompanied by complications. The disease can affect the small and large intestines together or separately. The incidence of the disease is approximately twenty-five cases per hundred thousand people. In this case, a mixed form of the disease is most common, when both the large and small intestines are affected. Risk factors for the development of the disease include genetic predisposition, chronic intestinal pathologies. Macroscopic examination distinguishes ulcers and granulomatous growths, while microscopic examination reveals edema in the damaged area and hyperplasia of the lymphofollicles of the submucosal membrane. Stages of disease development:
- Acute stage. Characterized by acute diarrhea, exhaustion, pain in the right side of the abdomen.
- Subacute stage. Characterized by an increase in the number of ulcerative lesions, the appearance of granulomas, and the development of intestinal stenosis. The pain syndrome is cramping.
- Chronic stage. Characterized by further development of the disease and occurrence of complications.
Causes of Crohn's Disease
The causes of Crohn's disease are currently not fully understood. There are suggestions that this disease can be inherited and can also be triggered by infectious pathologies and immunological factors.
 [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ]
[ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ]
How does Crohn's disease develop?
Crohn's disease begins with crypt inflammation and abscess formation, which progress to small focal aphthoid ulcers. These mucosal lesions may progress to deep longitudinal and transverse ulcers with preceding mucosal edema, forming the characteristic "cobblestone" bowel changes.
The spread of transmural inflammation leads to lymphedema and thickening of the intestinal wall and mesentery. Mesenteric adipose tissue usually extends to the serosal surface of the intestine. Mesenteric lymph nodes often enlarge. Extensive inflammation may lead to hypertrophy of the muscular layer, fibrosis and formation of stenosis, which may cause intestinal obstruction. Abscess formation and fistula formation with adjacent structures, including other intestinal loops, the bladder or psoas are characteristic; they may even open onto the anterior or lateral abdominal walls. Regardless of the intra-abdominal activity of the process, perianal fistulas and abscesses occur in 1/4-1/3 of cases; these complications are often the most unfavorable aspects.
Noncaseating granulomas may develop in the lymph nodes, peritoneum, liver, and affect all layers of the intestinal wall. The pathognomonic sign is the detection of granulomas, but Crohn's disease in 50% of patients is not characterized by the presence of granulomas. Their presence is most likely not associated with the clinical course.
The affected segment of the intestine is clearly demarcated from the normal intestine (the "silent zone"); hence the name - regional enteritis. Crohn's disease affects only the ileum in about 35% of cases (ileitis); in 45% - the ileum and colon are involved (ileocolitis), with predominant damage to the right flank of the colon; in about 20% of cases only the colon is affected (granulomatous colitis) and in most cases, unlike ulcerative colitis (UC), the rectum is not always affected. Sometimes the entire small intestine is involved (jejunoileitis). Very rarely the stomach, duodenum or esophagus are affected. In the absence of surgical intervention, the disease usually does not spread to areas of the small intestine that were not involved in the process at the initial diagnosis.
There is an increased risk of developing cancer in affected areas of the small intestine. Patients with colonic involvement have a long-term risk of developing colorectal cancer, similar to ulcerative colitis, depending on the extent and duration of the disease.
Symptoms of Crohn's Disease
Crohn's disease is characterized by the following initial symptoms: chronic diarrhea with abdominal pain, fever, anorexia, and weight loss. The abdomen is tender and may be tender to palpation, with a mass or tenderness. Significant rectal bleeding is uncommon, except in isolated colonic lesions, which may also occur in ulcerative colitis. Some patients develop an acute abdomen, simulating acute appendicitis or intestinal obstruction. About one-third of patients have perianal lesions (especially fissures), which are sometimes the main manifestations or even the cause of complaints. In children, extraintestinal manifestations often predominate over gastrointestinal symptoms; arthritis, fever of unknown etiology, anemia, or growth retardation may be the main manifestations, and abdominal pain or diarrhea may be absent.
If Crohn's disease recurs, its symptoms change. Pain is the main symptom and occurs with a normal relapse. Patients with severe exacerbation or abscess formation experience tenderness on palpation, protective tension, peritoneal symptoms, and signs of general intoxication. Areas of intestinal stenosis can cause intestinal obstruction with characteristic colicky pain, bloating, constipation, and vomiting. Adhesions after previous surgeries can also cause intestinal obstruction, which begins acutely, without fever, pain, and malaise characteristic of obstruction during exacerbation. Formation of a vesicointestinal fistula can cause air bubbles in the urine (pneumouria). Free perforation into the abdominal cavity is uncommon.
Chronic Crohn's disease causes a variety of systemic symptoms, including fever, weight loss, wasting, and extraintestinal manifestations.
Crohn's disease is divided into three main forms according to the Vienna classification: (1) primarily inflammatory, which after several years of disease progression usually becomes either (2) stenotic or obstructive, or (3) primarily penetrating or fistulous. These different clinical forms determine different approaches to treatment. Some genetic studies suggest a molecular basis for this classification.
Crohn's Disease and Pregnancy
Crohn's disease and pregnancy are viewed differently by different specialists. Some of them claim that Crohn's disease does not have a significant impact on the course of pregnancy, the birth process and the fetus, except in cases of exacerbation of the disease during this period. However, most specialists believe that pregnancy can have a negative impact on the development of the disease, since the enlarged uterus puts pressure on the intestinal sections, and the level of endogenous cortisol increases, which rapidly falls after childbirth. The prognosis of the disease also depends on whether the pregnancy occurred during remission or exacerbation. If the disease is uncomplicated, this usually does not affect the course of pregnancy. In severe cases, Crohn's disease can provoke the risk of miscarriage, and can also pose a threat to the life of the fetus during childbirth. Complications during the birth process most often occur if the disease arose or worsened during pregnancy. Exacerbation of the disease during pregnancy is difficult to detect, since the clinical picture practically does not change. In cases of intestinal obstruction, intestinal stenosis, and fistula formation, a negative impact on the course of pregnancy occurs even during the period of remission of the disease. With a persistent weakening of the symptoms of the disease, pregnancy in the presence of Crohn's disease is permissible, while its exacerbation is a contraindication for conception.
Where does it hurt?
Crohn's disease and ulcerative colitis
Crohn's disease and ulcerative colitis are believed to be related to hereditary predisposition, as well as to the impact of infectious agents on the gastrointestinal tract. The main difference between these diseases is that in ulcerative colitis, usually only the large intestine is vulnerable, while in Crohn's disease, various parts of the gastrointestinal tract are affected. The lesion in ulcerative colitis is usually concentrated in one segment of the large intestine. In Crohn's disease, the lesion can cover multiple areas of the intestinal tract. The symptoms of Crohn's disease and ulcerative colitis are very similar to each other, and it is not always possible to accurately distinguish them. A biopsy is usually prescribed to differentiate these two diseases. Common signs of these pathologies are diarrhea and fever, abdominal pain, loss or complete loss of appetite, weight loss, and general weakness. Nausea and vomiting, joint pain may also be present. It should be noted that similar symptoms can also be observed in other pathologies of the gastrointestinal tract, so qualified diagnostics are extremely important for establishing the correct diagnosis.
Why is Crohn's disease dangerous?
In order not to delay treatment and promptly seek help from a specialist, the patient needs to know why Crohn's disease is dangerous:
- As the disease progresses, the number of intestinal segments affected increases.
- Recurrence of the disease as a result of surgical intervention (lesion of the proximal intestine).
- Formation of fistulas in the rectum and other parts of the digestive tract.
- Development of extraintestinal pathologies (erythema, pyoderma, episcleritis, uveitis, ankylosing spondylitis).
- Intestinal obstruction.
- Risk of developing adenocarcinoma.
- Perforation of the colon, development of intestinal bleeding.
- Dilation of the colon.
- Insufficient absorption of nutrients in the small intestine.
Diagnosis of Crohn's disease
Crohn's disease should be suspected in patients with symptoms of inflammation or obstruction, in patients without obvious gastrointestinal symptoms but with perianal abscesses, and in those with unexplained arthritis, erythema nodosum, fever, anemia, or (in a child) poor growth. A family history also increases the suspicion of Crohn's disease. Similar symptoms and signs of Crohn's disease (eg, abdominal pain, diarrhea) may result from other gastrointestinal diseases. Crohn's disease is differentiated from ulcerative colitis; the diagnosis may be difficult in the 20% of cases in which Crohn's disease is limited to the colon. However, because the treatment of these diseases is similar, this distinction is important only when considering indications for surgical treatment or empirical therapy.
Patients with symptoms of acute abdomen (either new or recurrent) require AP and lateral abdominal radiography and abdominal CT. These studies can identify obstruction or other possible causes of acute abdomen (eg, appendicitis). Ultrasound can better evaluate gynecologic pathology in women with lower abdominal and pelvic pain.
If the initial manifestations of the disease are not acute, an upper GI and small bowel examination with targeted radiography of the terminal ileum is preferable to CT. GI studies are diagnostic if they show marked narrowing (producing a "string sign") or separation of bowel loops. If these findings are equivocal, enteroclymes or capsule enteroscopy may reveal superficial aphthous and linear ulcers. Barium enema may be used if colonic symptoms predominate (eg, diarrhea), which may show barium reflux into the terminal ileum with valve insufficiency, nodularity, rigidity, wall thickening, and luminal narrowing. Similar radiographic findings are seen in cecal cancer, ileal carcinoid, lymphosarcoma, systemic vasculitis, radiation enteritis, ileocecal tuberculosis, and amoebic granuloma.
In atypical cases (eg, predominantly diarrhea with minimal pain), Crohn's disease is diagnosed similarly to suspected ulcerative colitis, with colonoscopy (including biopsy, studies of pathogenic intestinal flora, and, if possible, imaging of the terminal ileum). Upper GI endoscopy may reveal gastric and duodenal involvement even in the absence of upper GI symptoms.
Laboratory studies should be performed to diagnose anemia, hypoalbuminemia, and electrolyte abnormalities. Liver function tests should be performed; elevated alkaline phosphatase and γ-glutamyl transpeptidase levels suggest possible primary sclerosing cholangitis. Leukocytosis or elevated acute phase reactants (eg, ESR, CRP) are nonspecific, but periodic monitoring can be used to monitor disease activity.
Perinuclear antineutrophil cytoplasmic antibodies are present in 60-70% of patients with ulcerative colitis and only 5-20% of patients with Crohn's disease. Crohn's disease is characterized by the presence of antineutrophil-Saccharomyces cerevisiae antibodies. However, these tests do not reliably differentiate between the two diseases. They have some value in cases of "indeterminate colitis" and are not recommended for routine diagnostics.
 [ 23 ], [ 24 ], [ 25 ], [ 26 ]
[ 23 ], [ 24 ], [ 25 ], [ 26 ]
Algorithm for diagnosing Crohn's disease
Crohn's disease is diagnosed using X-rays and endoscopy, which allow assessing the condition of the gastrointestinal tract. When analyzing feces, the presence of leukocytes is determined. The presence of leukocytes in feces indicates an inflammatory process in the intestinal walls. If the disease causes loose stools, they are examined for the presence of infectious agents, helminth eggs and clostridia. When diagnosing Crohn's disease, the irrigoscopy method is used - an X-ray of the colon with the introduction of a contrast agent (an aqueous solution of barium sulfate with tannin). Two to three days before the examination, the patient is recommended a special diet, and the day before - to take castor oil orally (about thirty grams). In the evening, an enema is given and no food is eaten until the end of the procedure. X-ray examination of the barium passage is carried out in order to assess the evacuation capacity of the colon and its interaction with other organs. The intubation enterography method allows examining the small intestine by introducing barium into it using a nasogastric tube. After X-ray, scintigraphy can be performed to differentiate inflammatory and non-inflammatory processes. This method allows examining the activity of the gastrointestinal tract and is based on the fact that the patient takes food labeled with a radioactive isotope, after which the process of its movement through the digestive tract is monitored using special equipment. As part of the comprehensive diagnostics, blood and stool tests and an immunogram are also performed.
 [ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ], [ 32 ]
[ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ], [ 32 ]
Tests for Crohn's disease
Blood tests for Crohn's disease show an increase in the erythrocyte sedimentation rate, water-salt imbalance, low plasma protein levels, and a deficiency of folic acid, vitamins B12, and D. Coproscopic examination reveals elevated levels of fatty acids and salts, the presence of a large amount of undigested starch in the feces, and elevated levels of nitrogen in the feces. Fibrogastroscopy reveals affected areas in the upper gastrointestinal tract. Rectosigmoidoscopy reveals pathological changes in the rectum. Endoscopy at the initial stage of the disease reveals aphthous erosive lesions, and mucus containing pus is present on the intestinal walls.
X-ray
When diagnosing Crohn's disease, X-rays are quite important, as they can be used to accurately determine the location of the inflammatory process. X-rays are especially important when examining the small intestine, as they are the only way to examine it. Before starting the procedure, the patient takes a barium-containing liquid orally, which can also be administered through the rectum (barium enema). On the X-ray, the liquid is recognized by its white color, which allows you to see ulcers, intestinal stenosis, etc. If such a study is ineffective, other types of X-rays are additionally prescribed.
Colonoscopy
Colonoscopy is quite important for diagnosing Crohn's disease. Colonoscopy for Crohn's disease allows you to get the most complete picture of the condition of the large intestine. It helps to identify the presence of ulcerative formations, inflammation and bleeding. Probing the large intestine allows you to examine it completely - from the cecum to the rectum. Usually, the procedure is carried out without prior anesthesia. Local anesthesia is done in cases where severe pain is localized in the anus, as well as in severe processes that disrupt the functioning of the small intestine, the formation of adhesions in the abdominal cavity. The procedure is carried out in a lying position with the introduction of a special device (colonoscope) through the anus into the rectum. Two days before the colonoscopy, the patient is shown a low-residue diet, the day before and on the day of the procedure, the diet should consist only of liquids (broths, teas). It is also recommended to take castor oil the day before the study. Two tablespoons of oil are dissolved in about half a glass of kefir and taken orally, which helps to completely cleanse the colon. In the morning, before the procedure, one or two more enemas are given - until the intestines are completely cleansed and water is released from it.
Who to contact?
How to treat Crohn's disease?
There is currently no clear answer to the question of how to treat Crohn's disease, since the causes of this disease have not been precisely established. Therefore, the main treatment for the development of this pathology is aimed at reducing inflammation, stabilizing the patient's condition and preventing complications. A gastroenterologist and a proctologist treat this disease. If there is an immediate threat to the patient's life, surgery is prescribed, for example, when an abscess develops, as well as when conservative treatment methods are ineffective. Conservative therapy for Crohn's disease primarily involves prescribing a diet, for example, table No. 4B. It helps reduce irritation of the gastrointestinal tract and fermentation processes, reduce gastric secretion and bile secretion. Various variations of dietary nutrition are aimed at minimizing pain and correcting the functioning of the digestive system. Drug treatment is aimed at relieving inflammation and symptoms of the disease, strengthening the body's defenses. The drug sulfasalazine is taken before meals four times a day, one to two grams in the acute phase of the disease. During the relief period, the dosage is gradually reduced to five hundred milligrams. The drug mesalazine is taken orally at 400-800 mg three times a day for two to three months. During the treatment, short-term use of corticosteroids, immunosuppressants, immunosuppressive agents that block cytokines that cause erosive and ulcerative formations on the intestinal walls is also possible. As an antibacterial therapy for the appearance of purulent formations, metronidazole and ciprofloxacin are used. Depending on the symptoms of the disease, the patient may be prescribed antidiarrheal or constipation medications, as well as anesthetics and hemostatic drugs, vitamin and mineral complexes.
Symptomatic treatment
Cramps and diarrhea may be relieved by loperamide 2-4 mg orally up to 4 times daily (preferably before meals). Such symptomatic therapy is safe except in cases of severe, acute colitis, which may progress to toxic megacolon as in ulcerative colitis. Hydrophilic mucilloids (e.g., methylcellulose or psyllium preparations) may sometimes help prevent rectal and anal irritation by increasing the stool consistency. Rough foods should be avoided in stenotic or actively inflamed colonic disease.
Treatment for mild cases
This category includes outpatients who are candidates for oral medication and who have no evidence of toxicity, tenderness, abdominal mass, or obstruction. 5-Aminosalicylic acid (5-ASA, mesalamine) is commonly used as the first line of treatment, although its efficacy in small bowel disease is limited. Pentasa is the most effective formulation for proximal ileal disease; asacol is effective in distal ileal disease; all formulations are roughly equivalent in colitis, although none of the newer agents rivals sulfasalazine in dose-dependent efficacy.
Some clinicians consider antibiotics to be the first line of treatment; they may be used in patients who fail 5-ASA for 4 weeks; their use is strictly empirical. Treatment with any of these drugs may be continued for 8-16 weeks.
Even if treatment is effective, patients with Crohn's disease require maintenance therapy.
Treatment for severe cases
In patients without abscesses but with persistent pain, tenderness on palpation, fever, and vomiting, or in case of ineffective therapy in mild cases, glucocorticoids are indicated, either orally or parenterally, depending on the severity of the disease and the frequency of vomiting. Oral prednisolone acts more rapidly and effectively than oral budesonide, but the latter has somewhat fewer undesirable effects. In patients in whom glucocorticoids are ineffective or in whom their dose cannot be reduced, azathioprine, 6-mercaptopurine, or possibly methotrexate should be prescribed. Infliximab is considered by some authors as a second-line drug after glucocorticoids, but its use is contraindicated in active infection.
Obstruction due to adhesions is initially treated with nasogastric aspiration, intravenous fluids, and sometimes parenteral nutrition. Uncomplicated Crohn's disease that has caused the obstruction resolves within a few days; failure to resolve promptly indicates a complication or other etiology of the obstruction and requires immediate surgical treatment.
Fulminant course of the disease or abscess formation
Patients with signs of intoxication, high fever, persistent vomiting, peritoneal symptoms, pain, and a palpable mass in the abdominal cavity should be hospitalized with intravenous fluids and antibacterial therapy. Abscesses should be drained by percutaneous puncture or surgery. Intravenous glucocorticoids should be administered only if infection has been excluded or suppressed. If glucocorticoids are ineffective within 5-7 days, surgical treatment is indicated.
Fistulas
Fistulas are treated primarily with metronidazole and ciprofloxacin. If treatment fails within 3-4 weeks, patients should be given immunomodulators (immunosuppressants, eg, azathioprine, 6-mercaptopurine) with or without infliximab for a more rapid response. Cyclosporine is an alternative, but they often recur after treatment. Perianal fistula tracts that are severe and refractory to treatment may be an indication for temporary colostomy, but they almost always recur after passage is reestablished; therefore, bowel disconnection should be considered an adjunct to radical surgery rather than a primary treatment.
 [ 40 ], [ 41 ], [ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ], [ 48 ]
[ 40 ], [ 41 ], [ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ], [ 48 ]
Supportive care
Patients who achieve remission with 5-ASA require maintenance therapy with this drug. Patients who require acute treatment with glucocorticoids or infliximab generally require maintenance therapy with azathioprine, 6-mercaptopurine, or methotrexate. Glucocorticoids are neither safe nor effective for long-term maintenance therapy. In patients who have responded to infliximab acutely but who have failed antimetabolite maintenance therapy, repeat doses of infliximab 5-10 mg/kg at 8-week intervals may be given during periods of remission. Monitoring during remission is based only on symptoms and blood tests and does not require radiographic or colonoscopic examination (other than routine annual dysplasia monitoring) after 7 years of disease.
Treatment with surgical methods
Even though approximately 70% of patients eventually require surgical treatment, surgery is always performed with caution. Indications for surgery in patients with Crohn's disease include recurrent bowel obstruction. Resection of the affected bowel may result in resolution of symptoms but does not cure the disease, since Crohn's disease is likely to recur even after resection of all apparently diseased bowel. The recurrence rates, as determined by endoscopic examination of the anastomotic area, are greater than 70% within 1 year and greater than 85% within 3 years; clinical symptoms develop in approximately 25-30% of patients at 3 years and in 40-50% within 5 years. Ultimately, repeat surgery is required in almost 50% of cases. However, the recurrence rate is reduced by early postoperative prophylaxis with 6-mercaptopurine, metronidazole, or possibly 5-ASA. If surgical intervention is performed as indicated, almost all patients report an improvement in their quality of life.
Nutrition for Crohn's Disease
Proper nutrition for Crohn's disease is quite important. With this disease, it is recommended to give up dairy and cereal products, caffeine, sugar, and alcoholic beverages. The daily water intake for this disease should be about one and a half liters. Diet No. 4 and its various variations are prescribed as a therapeutic diet for Crohn's disease. In the acute phase of the disease, diet table No. 4 is prescribed, you should eat five to six times a day, then switch to diet No. 4b. To restore bowel function, you can take glutamine before bed (five to ten grams of this substance should be diluted in a glass of water). Parenteral nutrition is recommended for severe exhaustion and constant diarrhea. An approximate menu for diet table No. 4 may be as follows:
- Wheat rusks.
- Low-fat broths.
- Rice or pearl barley soup with water.
- Strained porridge cooked without using milk.
- Steamed beef cutlets.
- Boiled lean fish.
- Kissel.
- Strong tea.
- Kefir.
- Blueberries or cherries.
- Rosehip decoction.
Diet table No. 4b includes low-fat soups, except for dairy and legume soups, dry biscuits, wheat bread, beef, veal, steamed chicken, low-fat boiled fish, fresh cottage cheese, kefir, boiled eggs, mashed porridge, boiled potatoes, carrots. The approximate menu for this table is as follows:
- First breakfast: steamed omelette, semolina, tea
- Second breakfast: baked apples
- Lunch: low-fat meat broth, boiled carrots, jelly
- Afternoon snack: rosehip infusion
- Dinner: low-fat boiled fish and mashed potatoes, tea or jelly
More information of the treatment
Prognosis for Crohn's disease
Crohn's disease is rarely cured and is characterized by intermittent attacks of relapse and remission. Some patients have a severe course with frequent, debilitating periods of pain. However, with adequate conservative therapy and, if necessary, surgical treatment, most patients achieve a good outcome and adaptation. Disease-related mortality is very low. Gastrointestinal cancer, including colon and small bowel cancer, is the leading cause of disease-related death.

