Medical expert of the article
New publications
Cystitis before, during and after your period
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Pain in the lower abdomen, frequent urge to urinate, change in the color of urine - such symptoms can occur both with the onset of menstruation and with inflammation of the bladder. But sometimes both menstruation and the disease appear together. How does cystitis before, during and after menstruation differ from the usual inflammatory process? Is there a connection between these two conditions?
Can acute and chronic cystitis be caused by menstruation?
The monthly cycle itself does not affect the development of cystitis. However, a number of factors are known that contribute to the development of the disease, and these factors are related to menstruation to one degree or another:
- pronounced hormonal changes during, before or after menstrual bleeding;
- failure to comply with individual hygiene rules during menstrual bleeding;
- sex during menstruation;
- failure to change pads or tampons in a timely manner;
- a sharp change in diet before menstruation (the so-called “hormonal gluttony”, consumption of large amounts of sweets);
- acute or chronic pathologies of the reproductive system.
Any of the above nuances can cause cystitis to become active at the very moment of the beginning of a new monthly cycle, although menstrual bleeding itself, of course, has nothing to do with it.
Causes menstrual cystitis
Cystitis associated with menstruation can develop for several reasons:
- activation of pathogenic microbes;
- infection from a sexual partner;
- uncontrolled intake of medications, self-medication;
- mechanical damage to the mucous tissues of the urethra or bladder.
The female reproductive organs are closely adjacent to the urinary system, so they indirectly affect each other. Pathogenic microbes that initially provoke cystitis easily "migrate" to the genitals. Therefore, it is possible for cystitis to affect menstruation, and vice versa.
Menstruation, its onset and course depend entirely on a woman's hormonal background. Often, with an imbalance of progesterone after menstruation, cystitis begins due to its relaxing effect on the smooth muscles of the urethra. As a result, it becomes much easier for infections to penetrate the urinary tract and bladder.
However, there are other circumstances that can lead to the problem.
For example, why do I get cystitis before my period? It could be the result of a disrupted vaginal microflora or changes in nutrition. Other reasons cannot be ruled out:
- stagnation of blood clots in the vagina and on the external genitalia, which is usually associated with untimely replacement of pads and tampons;
- inflammation in the genital area (for example, in the ovaries);
- thrush;
- allergic reactions to pads or tampons, to detergents.
Cystitis with a delay in menstruation does not always indicate the beginning of pregnancy. Of course, the regularity of the cycle depends on the hormonal background and the normal functioning of the ovaries, and inflammatory processes can cause failures - both hormonal and functional. Experts point out that the delay sometimes occurs during the inflammatory process, and even when the symptoms of cystitis have already subsided. The latter is due to the effect of certain medications on the functioning of the reproductive organs.
So can cystitis be the cause of a delay in menstruation? Most often, several factors are present at once. For example, hormonal imbalances or inflammatory diseases of the genital area provoke the development of cystitis, and, as a result, the monthly cycle is disrupted. The inflammatory process in the bladder itself, in the absence of additional factors, very rarely becomes the direct cause of a delay.
If cystitis begins during menstruation, the reasons are quite obvious:
- it is possible that particles of discharge entered the urethral canal and then into the bladder, which caused an inflammatory reaction;
- sometimes irritation of the mucous membranes occurs due to the use of unsuitable sanitary pads - especially scented ones;
- we may be talking about sexually transmitted diseases (in the early stages they sometimes reveal themselves through the development of cystitis);
- It is possible that there was untreated candidiasis - a fungal infection that becomes active with the onset of monthly bleeding.
Thus, if you are concerned about thrush, cystitis, or your periods have disappeared, the causes must be sought through diagnostics. Such a condition is a serious stress for the body and requires immediate treatment. The examination must begin with blood and urine tests, as well as an ultrasound of the pelvic organs.
Risk factors
Cystitis before, during or after menstruation can be provoked by the following factors:
- sexual intercourse during menstrual bleeding;
- exacerbation of chronic pathologies of the reproductive system;
- disturbed vaginal microflora;
- frequent constipation associated with intestinal atony;
- ignoring individual hygiene rules;
- changes in diet before or during menstruation (for example, eating a lot of sweets, smoked foods);
- physical inactivity;
- frequent changes of partners, practice of unprotected sex;
- overwork, reduced immunity, chronic diseases in other organs;
- regular changes in hormonal levels;
- untimely change of pads, prolonged use of tampons;
- swimming in open water during menstrual bleeding;
- a special anatomical structure in some women (for example, the external opening of the urethra being too close to the vaginal vestibule).
Pathogenesis
Most often, cystitis during menstruation is caused by E. coli, Proteus or Staphylococcus. These microbes belong to the category of opportunistic pathogens and are activated only under the influence of certain factors that promote inflammation. In addition, cystitis can also occur for reasons not related to the monthly cycle - this is chemical, toxic and parasitic effects.
The fact that cystitis and menstruation often go "shoulder to shoulder" can be explained by the special anatomy of the female genitourinary system. A short and wide canal for urination, paraurethral glands, which can serve as a place for bacteria accumulation - all these factors are often indicated in the pathogenesis of the disease.
Other contributing factors include:
- prolapse of the pelvic organs, which is accompanied by a disruption of the blood supply to the bladder and topographic changes in the bladder and urinary canal;
- sexual intercourse during menstruation, since this results in retrograde penetration of vaginal contents into the urethral opening;
- failure to maintain genital hygiene during menstruation;
- hormonal fluctuations leading to temporary atony of the urinary tract, which facilitates infection.
A significant role in the pathogenesis of the disease is played by pathogens of infectious pathologies - for example, chlamydia, mycoplasmosis, ureaplasmosis; penetration of bacteria into the bladder is possible from inflamed tissues of nearby organs - for example, a similar mechanism of infection spread is characteristic of salpingo-oophoritis.
Symptoms menstrual cystitis
Most women experience the following initial symptoms when they develop period-related cystitis:
- frequent and painful urge to urinate;
- relatively small amount of urine excreted;
- burning sensation in the urethra during the release of urine;
- general malaise, pain in the lower abdomen, above the pubis;
- slight increase in temperature, signs of intoxication.
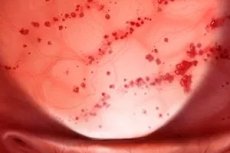
The shade of urine also changes: even visually, you can determine the appearance of turbidity and blood (especially at the end of the urinary process).
When the inflammatory reaction spreads to the kidneys, more severe symptoms occur: lumbar pain, dyspepsia, high temperatures.
Some patients complain of a feeling of cystitis before menstruation; cystitis a week before menstruation can manifest itself with the following symptoms:
- pain during urination;
- frequent and insufficient emptying of the bladder;
- pain of varying nature above the pubis;
- general discomfort;
- turbidity of urine.
Such exacerbations are generally associated with weakened immune defenses and hormonal imbalances. To be sure of this or that cause, it is necessary to undergo appropriate laboratory tests.
Cystitis and delayed menstruation are relatively rare developments. But if this happens two or more times, the problem must be solved comprehensively, since in such a situation there are always disorders not only in the urinary system, but also in the reproductive system. Cycle irregularities should always be alarming, and such "signs" from the body cannot be ignored. It is necessary to examine the hormonal state, check the functionality of the entire female reproductive system.
Cystitis and menstruation at the same time is not just a coincidence. In many cases, upon careful questioning, a woman is found to have other “hidden” symptoms:
- difficulties in conceiving;
- menstrual irregularities;
- chronic inflammatory processes of the female reproductive system;
- hormonal disorders.
In case of hormonal imbalances, cystitis before each period may manifest itself with the following symptoms:
- constant urge to urinate, frequent nighttime visits to the toilet;
- aching and tingling sensations above the pubis;
- spasms in the lower abdomen, radiating to the groin;
- pain when urinating.
Women may especially complain of constant fatigue that has no explanation. If you collect urine in a glass jar, you will notice a change in its color - turbidity appears, the shade becomes dark or pinkish.
When cystitis and a delay in menstruation are both troubling, a negative test may indicate inflammatory diseases of the reproductive system. The following are typical for such a situation:
- lumbar pain;
- chills, constant subfebrile temperature;
- periodic nausea and general weakness;
- sleep disturbances, headaches;
- pain during sexual intercourse;
- frequent periods of irritability and nervousness.
If you are bothered by similar symptoms, you should definitely see a doctor. Firstly, to find out the exact cause of the symptoms. Secondly, to undergo treatment and get rid of several problems at once: the inflammatory process and menstrual cycle disorders.
Cystitis and menstrual pain may be a coincidence, but sometimes they are still related to one cause. And such a cause most often lies in problems with the female reproductive system. Think: where is the pain most often localized? In the groin, back, abdomen (in the center, on the sides, below)? How long ago was it that you visited a gynecologist? The fact is that chronic pathologies of the internal genital organs are not always accompanied by clearly expressed symptoms. Therefore, cystitis can be one of the manifestations of the problem. And only a doctor can recognize the true root cause, guided by the results of diagnostics.
Cystitis with blood during menstruation is a reason to go to the doctor as soon as possible. You should not wait until the painful process spreads to still healthy organs and tissues. After all, some changes may become irreversible.
Complications and consequences
The most unfavorable complication of cystitis associated with menstruation can be pyelonephritis. The fact is that against the background of the inflammatory process, the function of the bladder is upset, ureteral-vesical reflux is formed - a disorder associated with the throwing of urine into the ureter and even into the kidneys. In addition, the edematous mucosa can put pressure on the ureter, which will disrupt the outflow of urine from the kidney. The pressure inside the pelvis increases, which contributes to the development of acute inflammation.
Does cystitis go away during menstruation? It is unlikely that you should hope that the inflammatory process will subside on its own. To avoid unpleasant complications, you need to visit a doctor in a timely manner, undergo a number of diagnostic procedures and begin treatment.
Diagnostics menstrual cystitis
The diagnosis is established based on the patient's complaints, as well as information obtained during examination and palpation. Laboratory and instrumental diagnostic data are additionally taken into account.
The following analyses are carried out in the laboratory:
- a general blood test will help to record the symptoms of an inflammatory reaction (leukocytosis, accelerated ESR);
- a general urine analysis will allow you to assess the functioning of the kidneys and bladder and detect pathological inclusions;
- biochemistry of urine fluid provides information on the content of salts, proteins, nitrites, etc.;
- urine culture to identify the pathogen and assess its resistance to antimicrobial drugs;
- analysis for sexually transmitted and fungal infections (gonorrhea, ureaplasmosis, chlamydia, candidiasis, etc.).
Additional instrumental diagnostics:
- Ultrasound examination of the kidneys and bladder visualizes the size, configuration, and condition of organs and tissues;
- cystoscopic examination and biopsy (microscopic examination of the bladder mucosa).
Differential diagnosis
Differential diagnostics are carried out after consultation with a urologist and gynecologist. Cystitis-like symptoms may appear in diseases of the female reproductive system - for example, adnexitis, parametritis, perimetritis. In this case, signs of inflammation are often observed on the mucous membrane of the bladder, since the infection can spread to nearby tissues.
In addition, it is necessary to exclude the presence of stones or tumors in the bladder.
Who to contact?
Treatment menstrual cystitis
After the necessary diagnostic measures have been carried out, the doctor will prescribe drug therapy. The treatment regimen usually uses drugs depending on the etiology of cystitis. Thus, antibiotics are used for microbial origin, fungicides are used for fungal infection, and antihistamines are prescribed for allergic reactions. Other possible prescriptions may include antispasmodics, painkillers, hormonal and anti-inflammatory drugs. Herbal medicines are also indicated, in particular, Canephron.
Diet is an essential condition for successful treatment. The consumption of products that can irritate the mucous tissue of the urinary system is limited or excluded. Such products include strong spices, salt, marinades (vinegar or sauces), smoked foods, sweets. Abundant fluid intake is recommended.
It is possible to connect physiotherapeutic methods: electrophoresis, inductothermy, UHF therapy, ultrasound therapy, laser treatment.
If the doctor prescribes antibiotic therapy, then the appropriate medications should be taken in full, and not until the main signs of the disease disappear. Untreated acute cystitis can quickly transform into a chronic form of the pathology.
What to do if you have cystitis during your period?
If cystitis starts to bother you periodically with the onset of menstruation, the first thing you need to do is go to see a specialist (urologist or gynecologist). Attempts to cope with the disease on your own can cause a new exacerbation, since incomplete or incorrect impact on the infection can cause "adaptation" of bacteria or fungi to a new type of treatment. And some drugs may be completely useless or even harmful.
What advice can you give to a woman suffering from cystitis during her period?
- try not to overcool your body;
- wash regularly, change intimate hygiene products (tampons, pads);
- give up strong spices, alcohol, carbonated drinks, sweets, and establish a drinking regime;
- abstain from sexual intercourse during treatment.
There are quite a few reasons that can lead to the appearance of an inflammatory reaction during menstruation. Therefore, the doctor prescribes treatment based on the identified causes of the disease.
Medicines
The choice of medication to eliminate cystitis during menstruation is the doctor's business. You should not try to solve the problem on your own, so as not to create conditions for the development of a new round of the disease.
In most cases, to eliminate the inflammatory reaction and destroy pathogenic flora, the doctor prescribes one of the following medications:
Monural |
An antibiotic successfully used to treat acute and recurrent microbial cystitis. The drug in the amount of one packet is diluted in a third of a glass of water, drunk before bedtime on an empty stomach, after emptying the bladder. In most cases, one dose of the drug is enough, but sometimes a second dose may be prescribed - in a day. Possible side effects: heartburn, dyspepsia. |
Furagin |
Furazidin is a drug, a representative of nitrofuran antimicrobial agents. Take 100 mg 4 times a day (day 1), then 3 times a day. The average duration of therapy is one week. Treatment may be accompanied by drowsiness, allergic reactions, nausea. |
Furamag |
Another drug is furazidin, which is taken 50-100 mg three times a day for a week. In general, Furamag rarely causes side effects, and only occasionally allergic reactions, headaches, nausea are observed. |
Amoxiclav |
A combined antimicrobial drug that combines amoxicillin and clavulanic acid. The tablets are taken with food, in an individually determined dosage. The duration of the treatment course is from one to two weeks. Side effects: nausea, bloating, stomatitis, allergy. |
Nolitsin |
An antimicrobial agent based on norfloxacin, a quinolone drug. Take 1 tablet twice a day, between meals. Treatment can last from three to ten days, at the discretion of the doctor. Nolitsin can cause digestive disorders, which disappear after the end of treatment. |
Ciprolet |
A fluoroquinolone antibiotic based on ciprofloxacin. Taken in tablets, 250-500 mg twice a day, regardless of food (at equal intervals - that is, once every 12 hours). Side effects are reversible: tachycardia, loss of appetite, sweating, skin itching, allergies. |
To relieve pain that occurs during menstruation, drugs with an antispasmodic effect are used - for example, Drotaverine or Papaverine.
Drotaverine |
An antispasmodic that eliminates spasms and spastic pain. Take 40-80 mg two or three times a day, or once. Side effects: decreased blood pressure, headache. |
Papaverine |
Myotropic drug, which is used in an individually selected dosage. Side effects: weakness, sweating, constipation, nausea, hypersensitivity reactions. |
In addition to basic therapy, it is appropriate to prescribe herbal remedies that have a diuretic, analgesic and anti-inflammatory effect. Such remedies include Kanefron and Fitolizin.
Canephron |
A herbal preparation with lovage, centaury, and rosemary. It has anti-inflammatory and antispasmodic properties. It is recommended to take two tablets of the preparation in the morning, afternoon, and evening. The duration of treatment is determined individually. During therapy, allergic reactions and stool disorders are sometimes noted. |
Phytolysin |
Diuretic, anti-inflammatory, bacteriostatic and analgesic medication. Take one teaspoon of paste-like mass in 100 ml of warm water, up to 4 times a day, for a long time. Side effects - allergy. |
 [ 21 ]
[ 21 ]
Vitamins for cystitis associated with menstruation
Doctors recommend taking multivitamin preparations containing antioxidants on a regular basis. The following must be included in the treatment plan:
- ascorbic acid 0.5-1 g per day to strengthen the immune system;
- omega-3 fatty acids (for example, flaxseed oil or fish oil) one tablespoon, or two capsules twice a day, to speed up the body's recovery;
- preparations with probiotics (from 5 to 10 billion KE per day) to improve the microbiome;
- grapefruit juice or encapsulated grapefruit seed extract for mild antimicrobial and antifungal action.
How to treat cystitis during menstruation at home?
When cystitis periodically bothers you during your period, the first thing you need to do is consult a doctor.
As for the procedures that you can carry out at home, we can recommend the following:
- During the day, wash yourself several times with warm boiled water with the addition of baking soda (1 teaspoon per 200 ml of water);
- drink plenty of pure water or herbal tea, without sweeteners;
- temporarily stop eating sweets, bread, milk, vinegar, sauces, salt and seasonings;
- eat more plant foods (preferably vegetables and greens);
- give up drinking alcohol.
What else is needed? In case of severe pain and spasms, first aid for cystitis during menstruation may consist of taking 1-2 No-shpa tablets. Do not forget to wear warm clothes to avoid hypothermia, remember to frequently clean your genitals, rest more, and do not be nervous.
Is it possible to heat the bladder area for cystitis during menstruation? No, it is better not to do this, as it can significantly increase menstrual bleeding. It is more reasonable to use medications and herbs with anti-inflammatory, analgesic and antispasmodic properties.
 [ 22 ]
[ 22 ]
Folk remedies
Folk remedies have been used by people for many centuries: proven medicines helped to fight infection, relieve pain, and also had a pronounced antifungal, antispasmodic and analgesic effect.
To prevent and treat cystitis associated with menstruation, you can use various tinctures, decoctions, and even fresh plants - they are taken internally or externally, depending on the recipe.
Before trying to cure cystitis during menstruation using folk remedies, you should consult a doctor in advance.
To improve the quality of urine and eliminate its irritating effect, it is recommended to drink 200 ml of warm water with lemon juice at least three times a day. This juice can be replaced with cranberries or horsetail infusion.
A remedy based on parsley has a good healing effect. One teaspoon of crushed leaves is poured with a glass of boiling water, infused under a lid for a couple of hours. Take the remedy one third of a glass before meals.
Cranberry decoction has also proven itself to be excellent. To prepare it, half a glass of berries are blended, the juice is squeezed out and placed in the cold. The resulting pulp is placed in a saucepan, 500 ml of water is added, and boiled for 6-8 minutes. The resulting product is cooled, the juice obtained earlier is added to it, as well as 2 tbsp. honey. The drink is drunk throughout the day.
 [ 23 ], [ 24 ], [ 25 ], [ 26 ], [ 27 ]
[ 23 ], [ 24 ], [ 25 ], [ 26 ], [ 27 ]
Herbal treatment
To eliminate cystitis associated with menstruation, it is necessary to take herbal infusions or decoctions every day, without skipping doses or reducing the dosage. The following herbs and plants are optimally used:
- Yarrow - it astringents, tones the bladder, relieves spasms, destroys fungus and bacteria.
- Thyme - perfectly relieves pain, easing painful urination during exacerbation of cystitis after menstruation.
- Plantain leaves – have a diuretic effect, soothe and soften the symptoms of inflammation.
- Parsley leaves are able to cleanse the urinary system of toxic products and stop the development of the inflammatory process.
- Juniper - has antiseptic properties, helps to destroy fungal and microbial infections. The plant is used for chronic cystitis outside the exacerbation phase, to prevent relapse.
- Horsetail is a mild diuretic and antimicrobial agent that, when used over a long period of time, can cure even chronic cystitis.
- Horse chestnut – strengthens not only the vascular walls, but also the bladder.
- Ivy – suitable for external use (washing, sitz baths), eliminates spasms in the acute period of cystitis.
- Ginseng – optimizes immune defense, enhances the body’s response to bacterial infection.
- Echinacea is widely used for frequently recurring cystitis, as it quickly eliminates the inflammatory reaction, thanks to its antimicrobial and antiviral properties.
- Couch grass – eliminates pain and burning during urination, reduces the frequency of urges, and has a pronounced anti-inflammatory effect.
- Chamomile flower is suitable for both external and internal use. The infusion of flowers is taken internally instead of tea, used for washing and irrigation. The plant has antimicrobial, antispasmodic, anti-inflammatory properties.
- Dandelion leaves - speed up the healing of cystitis by accelerating the removal of toxic substances from the urinary tract.
- Burdock – has antifungal and antimicrobial properties.
- Alfalfa is an effective antiseptic and diuretic that will speed up the healing process.
Homeopathy
Treatment with homeopathic remedies is an excellent addition to basic therapy. It qualitatively increases the body's immune defense, promoting active resistance to the pathogen. In addition, such drugs have a number of advantages:
- practically do not cause allergies;
- do not lead to addiction;
- accessible and safe;
- they can be combined with any other types of treatment (including antibiotic therapy);
- suitable for both treatment and prevention;
- are allowed for both adults and children.
Usually the course of homeopathic remedies is long, lasting several months (at the discretion of the specialist).
Recommended drugs:
- Cantharis - used for severe pain and burning, frequent urination with dark bloody urine. The most common dosage is 5 granules of 9CH every hour and a half.
- Mercurius corrosivus - prescribed for painful tenesmus, blood in the urine. The dosage can be 5 granules of 7 or 9CH every hour and a half.
- Arsenicum album – taken for burning pains that can be relieved by applying heat. Dosage – 5 granules 9CH every 2.5 hours.
- Terebinthina - prescribed in the presence of dark urine with sediment, 5 granules of 5CH every six hours.
After the acute symptoms of cystitis have been eliminated, the frequency of taking the drug is reduced. During the entire treatment, it is recommended to pay sufficient attention to rest and drink plenty of fluids.
Surgical treatment
In the vast majority of cases, when cystitis develops during menstruation, the doctor will prescribe drug therapy. Only in complex, advanced situations may the help of a surgeon be needed. Surgical intervention is indicated in the presence of a tumor process or a growing cystic formation.
 [ 33 ]
[ 33 ]
More information of the treatment
Drugs
Prevention
Cystitis before, during and after menstruation is always easier to prevent. To do this, you just need to remember a few rules:
- maintain hygiene before and after sexual contact;
- avoid synthetics in underwear;
- carefully select cleaning and hygiene products;
- visit your gynecologist regularly for routine examinations;
- do not overcool, dress according to the weather;
- change pads frequently (both daily and those used during menstruation);
- eradicate bad habits (do not smoke, do not drink alcohol, limit consumption of sweets, do not overeat);
- stop using tampons.
Cystitis is a common, but not as harmless disease as it seems at first glance. If such a problem has appeared, it will not disappear on its own: the lack of treatment can cause a lot of other problems in the body. Therefore, in order to protect yourself from health problems, it is necessary to consult a doctor at the first painful signs.
Forecast
The prognosis of cystitis, directly or indirectly related to the onset of the menstrual cycle, may depend on many factors. However, the main condition for a favorable outcome of the disease is the timely start of treatment prescribed by the doctor. Independent searches for a miracle cure usually do not lead to anything good: in most patients, as a result of self-medication, cystitis becomes chronic.
The first thing the doctor will do is try to establish the underlying cause of the inflammatory process by diagnostics. Only by knowing this cause exactly, the doctor will be able to prescribe the appropriate individual treatment.
Cystitis before, during and after menstruation can be cured without much difficulty: the main thing is not to start the painful process and to see a doctor in a timely manner.

