Medical expert of the article
New publications
Anal fissure
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Anal fissure is the second most common disease of the rectum, occurring in 60% of cases in women.
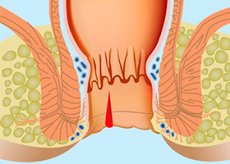
An anal fissure (rectal fissure; anal ulcer) is an acute longitudinal rupture or chronic, ovoid ulcer of the squamous epithelium of the anal canal. It causes severe pain, sometimes with bleeding, especially during defecation. Diagnosis is made by examination. Treatment of anal fissure consists of local hygiene, the use of stool softeners and, sometimes, injections of botulinum toxin.
What causes anal fissure?
An anal fissure is thought to develop due to damage to the anal canal by hard or heavy stools, with secondary infection developing. Trauma (eg, anal sex) is a rare cause. An anal fissure can cause spasm of the internal sphincter, which in turn disrupts the blood supply and creates conditions for chronicity.
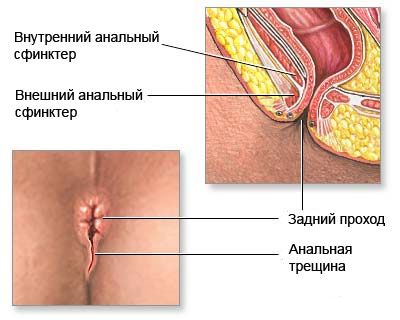
An anal fissure is a linear or triangular defect in the anal canal wall, 1 to 1.5 cm long, located near the transitional fold above the Hilton line. The origin of the fissure is associated with many reasons, but the most important factor is trauma to the mucous membrane of the anal canal by feces, foreign bodies, or damage during childbirth. A predisposing factor may be hemorrhoids. An acute anal fissure has a slit-like shape, smooth even edges, and its bottom is made up of sphincter muscle tissue.
With a long-term course of the pathological process, there is an overgrowth of connective tissue along the edges of the crack, its bottom is covered with granulation and fibrous plaque. In the area of the outer edge of the crack, excess tissue forms an anal (sentinel) tubercle. Thus, an acute anal fissure turns into a chronic one, which is essentially an ulcer with cicatricial edges and a cicatricial bottom. Sometimes an acute anal fissure disappears on its own, but most often it turns into a chronic one. As a rule, there is only one crack and most often it is located on the back wall of the anal canal, closer to the coccyx. Occasionally, 2 cracks appear on the back and front walls, which are located one above the other. True cracks should be distinguished from various superficial lesions of the perianal skin.
Symptoms of anal fissure
An anal fissure is usually located on the posterior wall along the midline, but can sometimes occur on the anterior wall. Fissures located away from the midline may have a specific etiology, especially Crohn's disease. A cutaneous papilloma (border tubercle) may be located at the outer end of the fissure, and an enlarged (hypertrophic) hair papilla may be present in its upper corner.
Acute fissures may be seen in infants, but chronic fissures are rare. Chronic fissures must be differentiated from cancer, primary syphilitic lesions, tuberculosis, and ulceration in Crohn's disease.
Fissures cause anal pain and bleeding. The pain usually occurs during or after a bowel movement, lasts for several hours, and disappears before the next bowel movement.
Where does it hurt?
What's bothering you?
What do need to examine?
How to examine?
Who to contact?
Treatment of anal fissure
An anal fissure can often be treated conservatively, with the aim of minimizing trauma during defecation (e.g., stool softeners, psyllium, fiber). Healing is aided by applications of protective zinc oxide ointments or soothing suppositories (e.g., glycerin), which lubricate the anal canal and facilitate stool.
Temporary relief is provided by local anesthetics (eg, benzocaine, xycaine) and warm (not hot) sitz baths for 10 or 15 minutes after each bowel movement and as needed.
Effective are 0.2% nitroglycerin ointment, 0.2% or 0.3% nifedipine cream, arginine gel and botulinum toxin injections into the internal sphincter, which relax the anal sphincter and reduce the maximum anal resting pressure, creating conditions for healing. If conservative treatment is ineffective, surgical treatment of anal fissure (internal anal sphincterotomy and dosed dilation of the anus) is indicated, which allows eliminating the spasm of the internal anal sphincter.
More information of the treatment


 [
[