Medical expert of the article
New publications
Transurethral resection of the prostate.
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Not only does a man's reproductive function depend on his quality of life, self-esteem, psycho-emotional and physical condition. Some problems in terms of sexual life can occur in men of any age, but there are also those that are very common among men 40 years and older. We are talking about the infamous prostatitis and prostate adenoma, which not only negatively affect a man's sexual function, but also create an obstacle to the normal outflow of urine from the body. And since this condition creates noticeable discomfort for the stronger sex and also causes health-threatening conditions, the need for treatment of the above pathologies is obvious, and prostate resection is one of the most effective methods if drug therapy does not give the expected results.
The prostate gland and its treatment methods
The prostate gland is one of the few internal organs that men have but women do not. The gland is part of the reproductive system and is responsible for producing a fluid that is a nutrient medium for spermatozoa – male semen. The secretion of the prostate mixes with sperm and ensures the viability of the small “tadpoles”, thanks to which a new life can be born.
The prostate (another name for the prostate gland) helps a man become a father and does not cause any unpleasant symptoms until it begins to increase in size. An increase in the size of the prostate can occur as a result of a long-term inflammatory process in the organ ( prostatitis ). Many men are in no hurry to see a doctor with their problem, which leads to the transition of the disease to a chronic form. And long-term inflammation in the absence of effective treatment leads to the proliferation of tissues of the affected organ (prostatic hyperplasia or, more simply, prostate adenoma).
Prostatitis and prostate adenoma are not the only pathologies in which an increase in the size of the organ is observed. As we know, a similar situation can be observed with uncontrolled division (proliferation) of malignant cells inside the organ. In this case, we are talking about oncology, i.e. a malignant tumor.
If prostate adenoma is a benign tumor, which during its growth only compresses nearby organs, causing disruption of their functioning, then prostate carcinoma is already a malignant process, in which not only the tumor grows due to the active division of malignant cells, but also poisoning of the body with toxic substances and the death of healthy cells.
But be that as it may, both prostatitis and prostate adenoma or carcinoma cause an increase in the size of the organ. And the location of the prostate gland is such that it surrounds the urethra, through which urine and seminal fluid (prostate secretion mixed with spermatozoa) exit the male body. It is clear that an increase in the size of the prostate entails compression of the urethral canal. Hence, problems not only with erection, but also with urination.
What is the threat of such a situation and what symptoms may indicate an increase in the size of the prostate gland? Most often, men complain of difficulties at the beginning of the act of urination, i.e. there is a feeling of a full bladder, there is a desire to urinate, but the release of urine is absent or it is painful. Moreover, the desire to visit the toilet for a small need arises quite often, but the amount of urine released is much less than expected. What is even worse is that at night the number of urges to urinate increases, while the likelihood of false urges also increases.
If the act of urination is productive, the man may be stuck in the toilet for a long time, since the urine will be released in a thin stream or even in drops. Over time, more and more prolonged episodes of hematuria can be noted, when blood particles are found in the urine.
Urine retention in the body, as one of the variants of stagnation, can lead to irritation of the walls of the bladder and infectious and inflammatory processes in it, the formation of urinary stones ( urolithiasis ), inflammation of the kidneys and the development of nephrolithiasis, which ultimately lead to renal failure ( renal failure ).
As we can see, the consequences of prostate enlargement are quite dire for men, so even before dangerous complications arise, everything must be done to avoid compression of the urethra. To stop the inflammation that causes the prostate gland to enlarge, medication is used, but if it does not help, it is necessary to resort to removing some part of the prostate, which causes compression of the urethra, or even the entire organ. This operation is called prostate resection. If we are talking about complete removal of the prostate gland, radical resection or prostatectomy is prescribed.
Indications for the procedure
Since the removal of part of the prostate gland, and especially all of its tissues, is a serious and responsible operation that can subsequently affect a man’s reproductive function, surgery is prescribed only in severe cases when drug treatment has not yielded results, and the patient’s condition raises concerns due to possible or already developing complications.
Surgical intervention on the prostate gland is indicated for the following categories of patients:
- men suffering from chronic prostatitis, which causes hardening of the prostate tissue,
- patients with chronic inflammation of the prostate gland, who have stones inside the organ, in the bladder or in the kidneys,
- patients with prostate adenoma, i.e. benign hyperplasia of the prostate gland, which is usually a consequence of prostatitis,
- those who have been diagnosed with prostate carcinoma or prostate cancer (to relieve symptoms and prevent the spread of the malignant process).
TUR surgery is prescribed to those who have previously had open surgeries, patients with diseases for which open surgeries are contraindicated, and young men for whom maintaining sexual function is important.
What symptoms, in addition to the formation of stones, must a patient have in order for such a radical method of treating the above-described pathologies to be prescribed:
- symptoms of urinary retention (intoxication, water-electrolyte imbalance, change in color and odor of excreted fluid, presence of sand in the urine),
- severe pain at the beginning of urination,
- increased urge to urinate, some of which did not result in the release of urine,
- frequent nighttime trips to the toilet to urinate, the number of which exceeds that during the day,
- a slow and prolonged act of urination, when urine is released in a thin stream or drop by drop,
- the presence of blood in the urine, recorded over a period of time.
If these symptoms can be relieved with medication, removal of the enlarged parts of the prostate is not necessary.
It is important to understand that prostate resection is not a complete method of treating the above-described diseases. It only allows you to remove dangerous symptoms of urinary retention and prevent complications associated with it. And in the case of prostate tissue hyperplasia, it also helps prevent the process from becoming malignant.
In prostate cancer, prostate removal helps to avoid metastasis to other organs if performed at an early stage of the disease.
Preparation
Operations to remove part of an organ or all of its tissues are rarely performed without preliminary preparation, and prostate resection is no exception. The main part of the preparatory process is a complete examination of the patient by a therapist, urologist, andrologist, including the necessary laboratory and instrumental studies.
Mandatory tests are:
- clinical blood test and urine test,
- detailed (biochemical) blood test,
- a blood clotting test called a coagulogram,
- microflora culture, as well as determination of the sensitivity of the identified pathogen to antibiotics (this is necessary because a course of anti-inflammatory therapy with antibacterial agents is administered before the operation),
- examination of biomaterial for syphilis ( blood test for RW ), hepatitis, HIV infection (tests can be taken separately or as part of a complex offered by many laboratories),
Additionally, venous blood may be taken to determine the blood type and Rh factor. This is especially important if these parameters have not been previously examined or if the patient has undergone a blood transfusion procedure.
In addition to tests, the therapist prescribes an ultrasound of the pelvic organs ( bladder, prostate ), fluorography or x-ray of the lungs, electrocardiography. The last two studies are important from the point of view of the introduction of anesthesia, which can be either local (spinal) or general. Consultations with a urologist and anesthesiologist are mandatory.
If inflammation of the prostate is caused by bacterial microflora, an effective course of antibiotic therapy is administered beforehand, which will prevent the spread of infection during surgery and the generalization of the inflammatory process.
In patients with an increased risk of bleeding, the date of surgery may be postponed for 1-3 months, during which a course of treatment with corticosteroids (Finacetride, Dutasteride, etc.) is carried out, which is necessary to reduce the blood filling of the prostate vessels. This should reduce the likelihood of such a complication as bleeding during surgery.
As for the preparation for the surgery itself, the patient is warned in advance that 1.5-2 weeks before the scheduled date of the surgery, he must stop taking any medications, especially anticoagulants, which make the blood less viscous and can provoke bleeding during resection. If a person cannot refuse medications (there are vital drugs for various diseases, the interruption of which is unacceptable), he must notify the doctor about this.
The evening before the operation, you need to perform hygiene procedures, do a cleansing enema and prepare (shave) the pubic area. Dinner the day before the operation should be early and not heavy. After 12 o'clock at night, you will have to limit your food and drink intake, which is due to the need to use anesthesia.
Before the introduction of invasive techniques, a course of antibiotic therapy is prescribed to everyone as a preventive measure against infectious contamination. Immediately before the operation, premedication is carried out, i.e. the introduction of sedatives to prevent somatovegetative reactions.
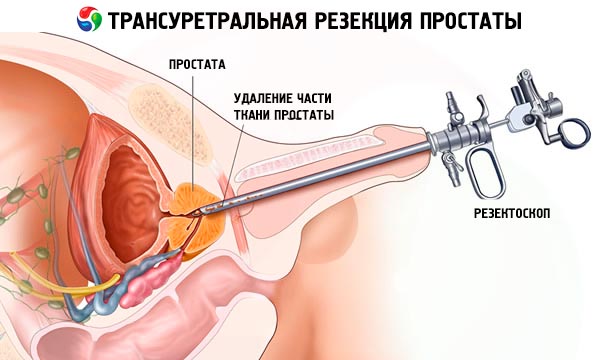
Technique Transurethral resection of the prostate.
Since the prostate is an internal male sexual organ and access to it is limited, the patient and doctor are faced with the question of choosing a surgical method. Previously, all surgeries were performed using the suprapubic method (transvesical adenomectomy), which was carried out almost by touch. Prostate resection surgery is a fairly popular method for solving the problem of an enlarged prostate gland, and surgeons at one time practiced removing the organ or its individual parts through an incision on the anterior abdominal wall under general anesthesia, after which the wound was sutured without coagulating the blood vessels.
It is clear that such surgical intervention implied a long rehabilitation period and had a negative impact on the man's sexual functions. In addition, there was always a risk of postoperative bleeding.
Gradually, with the development of medicine, preference began to be given to transurethral resection of the prostate (TURP) and the laparoscopic method, which are classified as minimally invasive and have fewer side effects compared to surgical prostatectomy.
The laparoscopic method is an innovative one. It was first discussed in 2002. In theory, it is the same surgical operation, but it is performed without large incisions on the body. Three or four punctures (no more than 10 mm) are made on the abdominal wall in front, through which surgical instruments, a video camera sending an image to a computer monitor, lighting, and air for improved visibility are inserted through trocars. The surgeon controls the instruments remotely, monitoring the progress of the operation on the monitor. The crushed parts of the prostate are removed through a drainage tube inserted into one of the punctures. The duration of the operation is about two and a half hours.
The advantages of the laparoscopic method are:
- the possibility of removing large prostates (more than 120 cm3 ),
- visualization of the surgeon's actions, ensuring a lower risk of damage to healthy tissue and incomplete removal of overgrown tissue,
- low risk of bleeding and complications during surgery,
- relatively low intensity of pain,
- the catheter after laparoscopic surgery is placed for a shorter period of time than after intervention using the suprapubic method,
- rapid return to physical activity (walking is allowed the next day after surgery),
- shorter hospitalization periods compared to the traditional method,
- absence of unsightly large scars,
- low risk of reoperation,
- almost complete disappearance of disease symptoms
- In many cases, it was possible to avoid urinary incontinence after surgery.
Transurethral resection is not a new technique. It has a long history. The prototype of the resectoscope, with which the TUR operation is performed, was invented at the end of the 19th century. We are talking about the Max Nitz cystoscope, with which urological diseases were diagnosed and tissues that prevented normal urine flow were cauterized.
The first resectoscope was invented by Max Stern in 1926. Its highlight was the electric loop, which was later repeatedly improved to accommodate high-frequency current, allowing not only tissue removal but also simultaneous coagulation (sealing) of blood vessels that were beginning to bleed heavily. This significantly reduced the risk of dangerous complications.

Transurthral resection of the prostate is a special type of surgery that leaves no traces on the patient's body, because the procedure of inserting a resectoscope inside does not require making incisions or punctures on the surface of the body. The fact is that access to the prostate is through the urethral canal.
A resectoscope is a tube 7-10 mm in diameter and about 30 cm in length with an optical system (telescope), valves for liquid used to wash the surgical area, and a set of instruments for removing and cauterizing tissue (coagulators, loops, curettes, electric knives). As in the case of laparoscopy, the doctor is able to visualize his actions, rather than cut by touch.
First, a resectoscope (through the urethra) is advanced into the bladder cavity, the organ itself and the area between the bladder and the urethra, where the prostate is located, are examined. Then, the prostate tissue or the adenoma inside it is removed with an electric loop or knife, which work like an excavator, i.e., the organ is removed in parts.
Small parts of the prostate enter the bladder, from where they are washed out with a special instrument. At the end of the operation, the doctor examines the cavity of the bladder and prostate. If there are bleeding vessels, they are sealed with a coagulator. When the doctor is sure that there is no risk of bleeding and all prostate tissue has been removed from the bladder, the resectoscope is removed and a tube with a balloon at the end, called a Foley catheter, is inserted into the urethra instead.
Once the balloon is inside the bladder, fluid is pumped into it, thus tamponading the prostate gland, preventing bleeding and providing rest to the area where the operation was performed. The filled catheter can no longer fall out.
The Foley catheter has not one, but three outlets, two of which provide uninterrupted flushing of the internal tissues of the bladder, and the third is intended for filling and emptying the balloon at the end of the catheter. The duration of bladder flushing depends on the presence of blood in the discharged fluid.
In our country, TUR technology operations have been actively carried out since the seventies of the last century. At first, it was about monopolar transurethral resection. Electrodes were located at both ends of the resection loop. The voltage supplied to them heated the knife to 400 degrees, which made it possible to simultaneously excise tissue and coagulate vessels. The main disadvantage of this method was the danger of current passing through the patient's entire body during the operation. It is clear that such an operation had many contraindications, and first of all, it was prohibited in cardiovascular pathologies.
Later, the technology was revised in favor of a new method - bipolar transurethral resection of the prostate. It is characterized by the location of both the cathode and the anode at one end of the loop, which means that the current passes strictly between them, reducing the risk of burning healthy tissue and other complications and allowing men with heart disease to get rid of the discomfort associated with an enlarged prostate, the most popular and effective non-invasive method.
Advantages of TUR surgery:
- low risk of bleeding, because the vessels are coagulated during the operation,
- minimal tissue trauma and the absence of incisions,
- the ability to control what is happening visually,
- short period of rehabilitation,
- minimum contraindications,
- the ability to simultaneously solve various problems: removal of prostate adenoma, cancer treatment (removal of the prostate gland is performed exclusively in oncology), removal of stones in the bladder, dissection of urethral strictures,
- no traces of surgery,
- the possibility of using gentle anesthesia,
- lower risk of sexual dysfunction than with open surgery,
- effective treatment for recurrent adenoma.
An even more effective and safe modern method of treating male problems is considered to be laser resection of the prostate, which is carried out in a similar way to TUR surgery. The same endoscopic equipment is used, but instead of an electric loop, all manipulations are performed by a focused beam of light (laser).
Using a laser, 4 types of operations can be performed:
- Contact laser (photoselective) vaporization of the prostate gland. This operation is a complete analogue of the usual TUR, but it is performed using a potassium-titanyl-phosphate and lithium-triborate laser. The tissues are removed layer by layer, but are not crushed, but evaporated (dried). In this case, the vessels affected by the laser are coagulated, preventing severe bleeding. This method has a minimum of complications, does not affect erectile function and is suitable for the treatment of prostate cancer at any stage.
The only disadvantages of the method are its high cost, long duration of the procedure (about 2 hours) and the lack of necessary equipment in public hospitals.
- Laser enucleation. This method is considered the newest (a little over 10 years) and the most advanced for organ removal. The operation uses endoscopic equipment and a holmium laser, which cuts the divided lobes of the prostate into parts convenient for extraction, rather than turning them into shavings, as in TUR surgery. The capsule of the prostate gland is not damaged, and the extracted parts of the organ can be used for histological examination.
This is also far from a cheap method of treatment. The operation can last from 1 to 2 hours depending on the size of the organ.
- Laser ablation. The method is similar to the previous one, but the prostate is not completely removed. The overgrown parts of the prostate are necrotized (cauterized) under the influence of the same holmium laser. The dead tissue will subsequently be excreted with urine.
- Interstitial coagulation. The least commonly used method of reducing the size of the prostate using laser-made incisions in the organ. The incisions will have to heal in the future, but the intensity of regenerative processes varies from man to man. This method is not used for large prostates.
A big advantage of any operation performed with a laser is the minimization of the risk of bleeding and infection of the body during the operation, as well as the absence of a negative impact on potency, which is very important in the treatment of young sexually active patients who dream of having heirs.
The doctor's choice of the method of performing the operation is influenced not so much by the patient's desire as by the size of the prostate. Thus, abdominal surgery is performed when the organ is larger than 85 cm 3. Laparoscopy is also possible when the prostate is excessively enlarged (more than 120 cm 3 ). And with the help of laser enucleation, it is possible to remove a prostate that has grown to 200 cm 3.
Among the remaining methods, only bipolar TUR is suitable for removing a large adenoma up to 120 cm 3. Using a monopolar operation, it is possible to remove an organ no larger than 80 cm 3, the same applies to laser vaporization. Laser coagulation is rarely used and only for relatively small prostate glands (30-60 cm 3 ).
Contraindications to the procedure
Prostate resection, like any other serious operation, has its own considerable list of absolute and relative contraindications that can become an obstacle to the operation or postpone it for several days or weeks. So, any surgical interventions are not performed if the patient has an elevated body temperature or blood pressure, or acute infectious (bacterial or viral) diseases. But the operation will be scheduled as soon as the symptoms of the disease go away.
The same applies to smoking and taking medications that affect blood clotting. The operation will be performed 2-3 weeks after the patient smokes his last cigarette or stops taking anticoagulant medications that are prohibited in this case.
As for absolute contraindications, surgical intervention is not performed in oncological diseases, with the exception of prostate cancer at an early stage of development. This is due to the risk of metastasis spreading hematogenously, i.e. through the blood. For laser vaporization, prostate cancer of stages 3 and 4 is not a contraindication, while conventional TUR is performed only at stages 1 and 2 of the disease.
The use of anesthesia may also impose restrictions for patients with problems in the functioning of the heart or respiratory system, especially in the case of insufficiency of the functions of vital organs. The greatest number of contraindications are when using general anesthesia, which is relevant for the traditional method of performing surgery by the suprapubic method and laparoscopy. TUR is performed mainly under spinal anesthesia.
Prostate resection is not performed on patients over 70 years of age, whose body, due to physiological wear and tear, may simply not be able to withstand such a load.
It is also undesirable to perform abdominal surgery on patients with endocrine disorders such as hypothyroidism ( thyrotoxicosis), goiter, diabetes mellitus, obesity (these pathologies are not contraindications for TUR surgery) due to the risk of various postoperative complications. Surgery may be refused to men suffering from severe intestinal pathologies and those who have problems that do not allow the introduction of endoscopic equipment into the urethra (for TUR). It is dangerous to perform operations in the pelvic area and on patients who have varicose veins in the pelvic area.
There is a high risk of severe bleeding in patients with hemophilia, which also becomes an obstacle to organ removal. However, laser vaporization makes it possible to help people with blood clotting disorders, because coagulation of blood vessels occurs immediately at the moment of their damage.
Be that as it may, the decision on the possibility of performing an operation on each specific patient is made by the attending physician, who is responsible for his decision and the life of the person who has entrusted his fate to his hands. Therefore, preference should always be given to professionals who have sufficient knowledge and experience in this area.
Consequences after the procedure
No matter what method is used to perform prostate resection, no doctor can guarantee that the operation will be without negative consequences. Most of them are after traditional abdominal surgery. The fact that it is performed practically by touch requires the surgeon to have a good knowledge of anatomy, a detailed study of ultrasound data, orientation in anatomical structures, and the ability to distinguish healthy tissues from pathologically altered ones without visual control. After all, if the tissues are not completely removed, there is a high risk that they will begin to grow again.
The recovery period after open surgeries is always longer and is accompanied by noticeable pain syndrome, requiring the use of painkillers. If an infection was introduced during the operation (and this cannot be ruled out during open surgeries), an additional course of antibiotic therapy will be required.
A surgical operation in the usual way implies a fairly large incision on the abdominal wall, which will take a long time to heal. If the fresh suture is not processed and manipulated properly, there is again a risk of infection of the wound.
An unpleasant consequence of open surgery is a decrease in sexual desire. The use of other methods reduces the likelihood of such an outcome, so they are considered more preferable for young and middle-aged patients. Complete lack of erection can be observed after prostate removal if the nerve fibers responsible for sexual functions were affected during the operation. This is an irreversible process.
In most cases, the decrease in sexual activity is temporary. After all, any operation, even a virtually painless one, is a trauma to the body, and it needs time to restore some functions. Over time, everything returns to normal, and the man continues to live a full life. If this does not happen for a long time, you will have to undergo additional examinations to identify the causes of the lack of erection.
A fairly common consequence of prostate surgery, more typical for the suprapubic method and TUR operations, is retrograde ejaculation, in which a man experiences an orgasm during an erection, but no semen is ejected. This does not mean that there is no sperm, it is simply ejected in the wrong direction (not into the urethra, but into the bladder). Some sperm may still be released during intercourse, but most of it is found in the urine, which becomes cloudy and whitish.
It should be said that the pathology does not affect the satisfaction from sexual intercourse for both partners, but there may be problems with conceiving a child. Retrograde ejaculation is treated in various ways (drug therapy, reflexology, physical therapy, plastic surgery of the sphincter of the bladder and urethra, etc.). But since the violation of ejaculation does not particularly affect sexual life, and the desire to conceive a child does not arise every day, during these periods you can try to have sexual intercourse with a full bladder, which will not allow sperm to slip past the entrance to the urethra.
With partial removal of prostate tissue, complete recovery does not occur in all cases. The frequency of relapses may vary depending on the method of performing the operation. But even with such effective treatment as laser resection, the probability of relapses is approximately 10%. However, a repeat operation will need to be performed after several years, when the organ tissues grow so much that they begin to squeeze the urethra.
Complications after the procedure
It should be said that even the methods with the least number of side effects, which include laparoscopy of the prostate, as well as complete or partial removal of the prostate gland with a laser, cannot completely prevent such a complication as postoperative bleeding. Even laser exposure, which allows for instant coagulation of vessels during surgery, does not exclude possible hemorrhages in the postoperative period, after necrotic tissues begin to peel off little by little. This is especially dangerous for people with blood clotting disorders.
It is impossible to exclude the appearance of cicatricial connections, adhesions and strictures at the site of the removed prostate and in the urethra. The latter can cause urinary disorders, and the relief for the man will be temporary. Subsequently, new operations will be needed to treat complications. The prevalence of such complications is about 2-5%.
TUR syndrome is considered to be a rather dangerous complication of transurethral surgery. It is associated with the need to wash the area of the operation during surgical intervention. Since at this time there is also damage to the vessels, some of the water can mix with the blood and enter the circulatory system. The smaller the prostate and the shorter the operation time, the lower the risk of such a complication, which can affect visual acuity and cause impaired consciousness. In principle, taking diuretics after surgery helps to forget about such symptoms quite quickly.
Sometimes complications are caused not by the specifics of the operation, but by the surgeon's carelessness or insufficient competence. They are usually inflammatory in nature and are caused by damage to various organs (urethra, bladder, prostate capsule, intestines) during the operation.
Another shameful complication that occurs in 17-83% of men after prostate resection by various methods is urinary incontinence, which is a psychotraumatic circumstance for an adult man. This consequence, associated with a violation of the innervation of the external urethral sphincter, is observed some time after the operation. It can go away on its own (a year after the operation, the number of patients with this complication decreases to 5-23%) or require special treatment.
What causes sphincter dysfunction? During open abdominal surgery, especially if the prostate is completely removed, there is a risk of damage to the nerve fibers responsible for contraction of the sphincter muscles and bladder. And during surgery with transurethral access, the proximal sphincter, which controls the flow of urine into the urethra, is stretched. Still, the surgery can last 1-2 hours, during which a tube will be inserted into the urethra, the diameter of which is large for the inlet from the urethra to the bladder.
Urinary incontinence may be observed in patients after surgery by any method, but the probability of such a complication is lower with laparoscopy. Excess weight and age of the patient can play a major role in the appearance of such a symptom. There is a relationship between the frequency of the symptom and the size of the prostate gland, concomitant pathologies, and episodes of enuresis in the past.
This complication requires special attention. And before taking any steps to eliminate the problem, it is necessary to conduct some diagnostics to exclude the infectious nature of the pathology. Usually the patient takes a urine test and bacterial culture for microflora, fills out a special questionnaire, where he describes all the nuances of enuresis. In some cases, it turns out that urinary incontinence was a consequence of stress, which can include the operation itself.
To determine the degree of enuresis, a Pad test is performed using absorbent pads. The volume of urine lost is measured over an hour. If it is less than 10 g, this indicates a mild degree of incontinence. The amount of urine within 11-50 g indicates a moderate degree, and above 51 g indicates a severe pathology.
A neurological examination, rectal and urodynamic examination, urethrocystoscopy and descending cystourethrography with contrast medium may be required to detect urethral strictures and fistulas.
Treatment of secondary enuresis usually begins six months to a year after surgery, because in most patients the problem goes away on its own during this time due to the body's compensatory capabilities. If normal urination does not return within this time, there is no hope for spontaneous restoration of sphincter function and various treatment methods must be used.
The following stages of treatment for urinary incontinence after prostate resection are distinguished:
- Conservative therapy, which is carried out for a year:
- drug therapy (anticholinergic drugs that normalize the contractile ability of the sphincter),
- therapeutic exercise for training the pelvic floor muscles,
- electrical stimulation of the pelvic floor muscles.
- Surgical treatment is carried out when long-term conservative treatment is ineffective:
- For mild to moderate incontinence, a minimally invasive procedure called a male sling is performed, which involves placing special bands in front of the hanging section of the urethra to provide mechanical compression of the urethra to stop urine loss between urinations.
- Severe enuresis is treated by implanting an artificial urethral sphincter.
- Surgery may also be required to remove scar tissue and adhesions that negatively affect the functioning of the genitourinary system, and this helps restore normal urine flow.
It is clear that urinary incontinence is a very unpleasant condition that occurs after prostate resection surgery and requires quite a lot of time to correct the situation. But this is not a reason to refuse surgical intervention, which allows you to solve the problem of urinary retention in the body and the complications that arise for a long time. It is better to cure enuresis than to suffer with diseased kidneys.
At least, there is always a choice of methods of performing the operation and clinics with personnel of different levels. No one is stopping you from visiting different hospitals and medical centers, talking to doctors, reading reviews on the Internet from people who have already undergone the operation.
Care after the procedure
Prostate resection is an operation that can be performed using various methods. But this does not change the attitude towards it as a surgical intervention, after which the body will need some time to recover, after all, some of its tissues were damaged, and the functions of the genitourinary system may be impaired. This means that the patient is required to be a certain amount of caution and follow the doctor's instructions to avoid dangerous complications.
Regardless of the method of performing the operation, after the procedure of complete or partial removal of the prostate, the patient is inserted into a catheter, which pursues 2 goals: unloading the urinary organs after the operation and cleaning the bladder from the blood accumulating there, particles of necrotic tissue, and possible infection. Inserting a catheter after prostate resection is considered a mandatory procedure. Another thing is that the duration of its presence in the body varies with different methods of surgery.
Patients who had the traditional open surgery will have to put up with the presence of a catheter for the longest time. For 7-10 days, blood may be released from the wound inside the body, which requires constant washing to prevent stagnation and infection of the bladder. During this entire time, the catheter will be in the urethra, removing urine and washing water to the outside.
After laparoscopy of the prostate, the duration of the catheter is shorter - from 2 to 4 days, depending on the intensity of the red coloring of the discharged fluid. If the fluid becomes light pink or does not have an unusual color, the catheter is removed.
In this regard, TUR surgery is even more pleasant, because you usually have to put up with a catheter for no more than 3 days, and after laser treatment with almost instant coagulation of vessels and minimal risk of infection, the tubes can be removed from the urethra after just 24 hours.
After the catheter is removed, the patient can go home, although in some cases this is allowed to be done earlier. While the catheter is in the body and after the tubes are removed from the urethra, the man may feel some discomfort. A foreign body in the urethra can cause painful spasms and false urges to urinate. After its removal, there may be a burning sensation when going to the toilet for a small need, urine sometimes has a pink tint. Such symptoms are not considered pathological and disappear on their own within a week.
After the catheter is removed, men feel noticeable relief. It becomes much more pleasant to urinate, because the liquid begins to flow in a strong stream. But you need to understand that the internal organs cannot fully recover in such a short period, and the bladder needs to learn to work normally again. Therefore, in the first days after the tubes are removed, you do not need to wait for the bladder to fill completely, it is recommended to go to the toilet every half hour, and on the 3rd-5th day at least once every 1 hour, especially since you will have to drink a lot.
The need for a large amount of fluid to enter the body is due to various reasons:
- from midnight on the eve of the operation the patient is not allowed to eat or drink, which means fluid replenishment is required; if the patient feels well, they may be allowed to drink as early as 2 hours after the operation, but not to eat until the next day,
- low fluid intake makes urine more concentrated, which irritates the walls of the bladder and can cause inflammation,
- there is a need for natural rinsing of the bladder cavity after the catheter has been removed, especially if the urine is still pink (necrotic tissue may still be excreted along with the urine for some time after cauterization with a laser or current; their retention in the body is also undesirable).
The patient will have to drink a lot (we are not talking about alcoholic beverages, but about water, tea, compotes), but there will be some restrictions in food. During the recovery period, you will have to give up fatty, spicy, very salty, fried and smoked foods. But boiled and steamed dishes, any low-fat dairy products, still mineral water will only be beneficial.
If the operation was performed using an open method or laparoscopic equipment, wounds from incisions and punctures remain on the body, which require antiseptic treatment with hydrogen peroxide or brilliant green, replacement of dressings and bandages, removal of stitches after the wound has healed well. After an open operation, the patient may stay in the hospital for more than a week, during which time the wound is monitored by medical personnel. After the time spent in the hospital, you will have to monitor the healing wound yourself. If severe pain is observed, the doctor prescribes painkillers
During this period, the man will have to limit his physical activity. For several days after the operation, he will not be allowed to get out of bed or strain his pelvic muscles too much. In principle, limiting physical activity (for 1.5 months, you cannot play sports, move actively, lift weights, or have sex) is relevant for all types of surgery. But after laparoscopy, the patient can get out of bed after 1-2 days, and after non-invasive methods, even on the same day or the next day after the operation.
To prevent infectious complications, patients are prescribed broad-spectrum antibiotic therapy in the postoperative period. The duration of antibiotic therapy is 1-2 weeks. After laser treatment, which minimizes the risk of infection, antibiotics are not required, but doctors prefer to play it safe. In addition, antibiotic therapy reduces the risk of developing inflammatory processes, which are very inopportune in the recovery period.
To reduce the load on the pelvic floor muscles and prevent bleeding, patients will need to monitor their bowel movements, avoiding constipation. Those who have digestive problems may need to take laxatives, which should be prescribed by the attending physician. In general, taking any medications for several days after surgery should be agreed upon with the attending physician, especially if we are talking about drugs that affect blood characteristics.
In the first days after the operation, it is not recommended to make sudden movements, jump out of bed, or squat. But hypodynamia will also not contribute to the restoration of organ functions. After leaving the hospital, patients are recommended daily walks in the fresh air, moderate physical activity, and special exercises to restore the tone of the urinary organs.
A common complication after prostate resection surgery is urinary incontinence. To restore the contractile ability of the urethral sphincter, it must be trained using special exercises. It may even be necessary to undergo a specialized course of treatment or resort to surgery to eliminate the consequences.
In order for recovery to be faster and more effective, men will need to adhere to a healthy lifestyle. For many, this is a great chance to give up bad habits and start a new life.
Feedback on the operation
Men, with their inherent pride and restraint, do not particularly like to talk about their problems, especially when it comes to sexual function and the delicate issue of urination. For this reason, they are not in a hurry to share their grief with a doctor until the problem reaches a scale requiring surgical intervention. This is also why there are few reviews of prostate resection surgery on the Internet. Who would want to tell the whole world that they have such a delicate problem that can affect their sex life?!
However, sometimes you can find posts where men share the results of their friends' treatment. And former patients of the urologist aged 65-75, who have nothing to be ashamed of, can tell you something about the effectiveness of surgical treatment.
It should be said right away that both of them speak enthusiastically about the surgical method of treatment, considering it the most radical method of treating the problem. Despite possible complications and nuances of the operation, men exhausted by the disease are ready to do anything to get rid of pain and problems with urination. Even such a complication as urinary incontinence hardly stops anyone.
The largest number of positive reviews is about laser treatment (laser vaporization), because it shows a minimal risk of complications such as bleeding and decreased erectile function, which is important for young men. And urinary incontinence in this case is rare. With laser enucleation, the risk of complications in the form of urinary incontinence, erectile dysfunction, retrograde ejaculation and minor bleeding is somewhat higher and is close to TUR surgery using an electric loop.
Speaking about the high cost of TUR surgeries and laser treatment, many former patients claim that drug therapy over several years drained even more money from their pockets, despite the fact that the result was negative.
Reviews of patients and their friends are confirmed by the opinion of doctors who note an improvement in the outflow of urine and the general condition of patients after any of the operations for the treatment of the prostate gland. In principle, if all the necessary studies are carried out and contraindications are taken into account, men tolerate the operation well, no matter what method it was performed. Another matter is the duration of the recovery period, possible complications and cosmetic marks on the body.
The most budgetary operation is considered to be the suprapubic operation by the open method, but it also gives the maximum number of complications and relapses, has a large number of contraindications, and recovery after it takes several months (up to six months), while after other operations a man completely returns to normal life after 1.5 months. Despite the cheapness, few men decide to risk their erectile function, which often remains impaired after open surgery.
There are few side effects after laparoscopic surgery. Urinary incontinence usually recovers on its own within six months, erectile dysfunction may be observed temporarily, severe bleeding is extremely rare.
TUR surgery, like laser treatment, shows the best long-term results, although the probability of urinary incontinence after urethral access still remains high. However, there are far fewer reviews of complications on the Internet than thanks to doctors for a good effect after surgery, which indicates the high efficiency of the method. In the end, much depends on the patient's age (the older the patient, the more difficult it is to restore the sphincter tone), the timeliness of seeking help (the size of the prostate increases gradually, and the larger it is, the longer the operation will be and the higher the risk of complications), the characteristics of the man's body and existing pathologies.
Prostate resection is considered a precise anatomical operation and requires high competence of the doctor in this field. But even knowledge of medicine, anatomy and surgery will not help if the doctor does not know how to properly handle the instruments necessary to perform a particular type of operation. In order for the result to be worthy, and the number of complications to be minimal, it is necessary to take a responsible approach to the choice of the clinic and the surgeon who will perform the operation, because men's health and self-perception as a man in the future depend on this. Risk is a noble cause, but not when it comes to a person's life and health.


 [
[