Medical expert of the article
New publications
Streptococcus agalactiae (Streptococcus agalactiae)
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
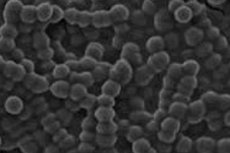
Beta-hemolytic group B streptococcus agalactiae (Streptococcus agalactiae) belongs to the Gram-positive bacteria. The species name is derived from the Greek agalactia - lack of milk, because before this coccus was isolated in humans and recognized as part of their normal microbiota, it was considered only a veterinary pathogen causing mastitis in dairy cows.
In foreign microbiology, the abbreviation for this bacterium is GBS - Group B Streptococcus. [1], [2]
Structure of the streptococcus agalactiae
Immobile, non-spore-forming bacteria of spherical or ovoid shape (0.6-1.2 µm in diameter), Streptococcus agalactiae is a diplococcus, that is, it grows in pairs, assembling in typical for all streptococci chains with colony formation.
These bacteria are Gram-positive, cytochrome- and catalase-negative. First of all, this means the presence of a capsule surrounding the microorganism with an outer cytoplasmic cell wall (membrane), which acts as an exoskeleton and consists of typical peptidoglycan, a number of proteins and various carbohydrate compounds, including teichoic acids.
Peptidoglycan not only protects the cell from host immunity, but is also an antigen, as glycopolymers - polysaccharide antigens of the cell wall - are attached to it. And teichoic acids are important for cell wall integrity and stability of cell morphology.
"Catalase-negative" refers to the absence of the enzyme catalase, an indication that Streptococcus agalactiae belongs to the host-associated facultative anaerobes capable of doing without oxygen depending on the environment. The definition of "cytochrome-negative" reflects the microorganism's inability to use oxygen to produce ATP, so S. Agalactiae, like many other prokaryotes, uses glucose as an energy source, synthesizing adenosine triphosphate by oxidative phosphorylation.
Since bacteria of the Streptococcaceae family have no tricarboxylic acid cycle for the synthesis of amino acids, they obtain them by cleaving peptides formed by amino acids from the tissues of the organism they penetrate. What makes S. Agalactiae "hemolytic" is its ability to cause complete dissolution (lysis) of blood erythrocytes, which is caused by cytotoxins produced by the bacterium: the enzyme β-hemolysin/cytolysin, known as cAMP factor extracellular diffusing protein; the glycopolyene pigment of the cell membrane ornithine-rhamnolipid (also known as grenadene).
Streptococcus agalactiae β-hemolysin/cytolysin is involved in bacterial invasion of host epithelial and endothelial cells, causing inflammatory responses; bacterial toxin factor cAMP binds human immunoglobulia G molecules IgG.
To colonize mucous membranes, this microbe attaches to epithelial cells by adhesion with the help of: adhesins; fibrinogen- and laminin-binding proteins; proteins binding blood plasminogen and extracellular matrix glycoprotein fibronectin, as well as peptidase C5a (surface serine protease). The latter is also a virulence factor of S. Agalactiae, suppressing the activity of host immune cells - phagocytes and neutrophils. [3]
Life cycle of the streptococcus agalactiae
Like other pathogens streptococcal infection, Streptococcus agalactiae, being a commensal bacterium, is able to survive and multiply in various anatomical niches and fluids of the host organism. The bacterium, which lives in the human body with a 5-week life cycle, colonizes the urinary tract, the conductive pathways of the internal female genitalia (in approximately 15-30% of all healthy adult women), the large intestine, and much less frequently the nasopharynx and upper respiratory tract. Many adults are asymptomatic carriers of S. Agalactiae (chronic or transient). [4]
The researchers found that outside the host, this bacterium can survive for many months in rooms where there is dry and a lot of dust... But it is killed by moist heat at t + 55ºC (within half an hour), and at t +120ºC - after 15 minutes. It is also killed by dry heat at constant t +170ºC for one hour.
Streptococcus agalactiae reproduces by the binary division characteristic of unicellular cells: one cell divides into two identical cells with DNA replication.
S. Agalactiae is not a sexually transmitted infection and is not transmitted through water or food. Like many bacteria, this microorganism can be transmitted from one person to another by contact, but since Streptococcus agalactiae is often found in a vaginal swab, infection through sexual contact is also possible.
To a newborn baby, group B streptococci can be transmitted during vaginal delivery - by exposure to fluids and contact with mucous membranes of the birth canal affected by the pathogen. [5]
Symptoms
What causes Streptococcus agalactiae? Group B beta-hemolytic streptococcus is considered one of the major infectious agents capable of causing invasive infections in children and adults.
At least one third of all clinical cases caused by S. Agalactiae occur in newborns in the first 24-48 hours after birth; infants older than two days of age account for 8%. However, 75% of infants exposed to the pathogen have no clinical signs of infection. [6]
Streptococcus agalactiae in newborns is recognized as a key cause:
- Meningitis in newborns (one to three months of age);
- Neonatal pneumonia;
- Septicemia;
- Neonatal sepsis.
The increased risk of giving birth to a baby infected with this coccus is indicated by: premature (18 or more hours before delivery) rupture of the fetal membranes and the discharge of amniotic fluid; premature delivery (before the 37th week of gestation); febrile condition during labor; urinary tract inflammation during pregnancy. [7]
Streptococcus agalactiae in pregnant women can cause: [8]
- Chorioamnionitis (infection of the amniotic fluid);
- Nonspecific bacterial vaginosis;
- Gestational pyelonephritis.
You may also develop postpartum endometritis, pneumonia, postpartum bacteremia, and sepsis.
And Streptococcus agalactiae in the cervical canal of the cervix can provoke inflammation of the cervix (cervicitis). [9]
Streptococcus agalactiae in men can lead to the development of not only asymptomatic inflammatory prostatitis, but also bacterial chronic prostatitis.
Serious invasive infections associated with this type of streptococcus are susceptible to the elderly and people with weakened immune systems, diabetes, cirrhosis and malignant neoplasms. Patients after certain types of surgery are also at risk. GBS infections in adults include:
- Pneumonia;
- Inflammation of the urinary tract - cystitis, urethritis;
- Skin and soft tissue infections (which may manifest as cellulitis, abscesses, foot infections or pressure sores);
- Systemic bacteremia - the presence of bacteria in the systemic bloodstream (with chills, fever and mental disturbances);
- Osteomyelitis;
- Bacterial meningitis;
- Infective endocarditis.
See also - symptoms of strep infection
Diagnostics
Streptococcus agalactiae can only be detected by appropriate laboratory bacteriologic tests. Read more in the publications:
- Flora smear
- Femofluoroscreen analysis in women and men
- Microbiologic and bacterioscopic examination of vaginal discharge
- Antibodies to streptococci A, B, C, D, F, G in blood
- Microscopic examination of urine sediment
The Christie-Atkins-Munch-Petersen (CAMP) test is also used to identify Streptococcus agalactiae.
In normal streptococci in a smear is found in an amount of up to 10^3 CFU/mL, but separately Streptococcus agalactiae norm in a smear in women is unknown. Although in the case of asymptomatic carrier in men, the number of S. Agalactiae bacteria no more than 10^4 CFU/mL may be considered acceptable.
Streptococcus agalactiae in urine norm is not recorded. And by bacterioscopic examination of urine sediment, agalactia in urine at levels less than 10^4 CFU/mL is defined as asymptomatic bacteriuria, and higher levels of bacteria in urine may cause symptoms of urinary tract infections.
In infants, this infection is diagnosed by analyzing a sample of blood or cerebrospinal fluid.
Treatment
The mainstay of antibiotic therapy for beta-hemolytic group B streptococcus is benzylpenicillin (Penicillin G).
The bacterium is also sensitive to other beta-lactam antibiotics - drugs of the cephalosporin group: ceftriaxone, Ciprofloxacin, Cefuroxime, Cefaxone, cefoctam and others.; carbapenems (Meropenem, etc.), and to vancomycin and gentamicin. Streptococcus agalactiae shows resistance to such antibacterial agents as Erythromycin, Clindamycin, Moxifloxacin (groups of fluoroquinolones).
Beta-lactam antibiotic of penicillin group Bicillin 5 with prolonged action is used (single intravenous injection) in outbreaks of respiratory streptococcal infection.
Also see:
Prevention of the streptococcus agalactiae
There is no vaccine against group B beta-hemolytic streptococcus for humans. To date, the only method to prevent infection in pregnant women is prenatal screening (screening for GBS colonization is used in most developed countries). And as a preventive measure against early and late onset of the disease in newborns, intrapartum antibiotic prophylaxis is carried out: intrauterine administration of antibiotics to pregnant women during labor.
Forecast
A favorable prognosis is possible with timely detection of Streptococcus agalactiae in women planning pregnancy, since the risk of death in infants with neonatal infection is currently estimated at 10-20%; 65% of cases involve the death of premature infants and newborns with a body weight of up to 2500 grams. According to some data, the incidence of neonatal sepsis is 3.5 cases per 10,000 live births.

