New publications
Analysis reveals new evidence of a global surge in group A streptococcus infections
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Group A streptococcus (Strep A) is a common type of bacteria that typically causes throat infections and scarlet fever. Although most infections are mild, in rare cases Strep A can cause invasive infections that can be fatal.
Between 2022 and 2023, health services around the world recorded a surge in severe invasive Strep A infections after pandemic restrictions were lifted. A new study by scientists at Imperial College London and Public Health England has confirmed that a variant of the bacterium called M1UK played a key role in the increase.
M1 strains are known to cause more invasive infections than other Strep A types. Although the variant was first identified and sequenced in the UK, M1UK has recently been linked to increased severe infections in Europe, Australia, North America and Japan following the lifting of pandemic restrictions. It has also been detected in South America, New Zealand and Taiwan.
Low levels of Strep A infections during the pandemic likely left the population, particularly children, particularly vulnerable to these infections, contributing to the surge in cases in many countries.
In a new study of the genetics of M1UK, published in the journal Nature Communications, scientists present new data on when the variant first emerged and how it compares to other strains.
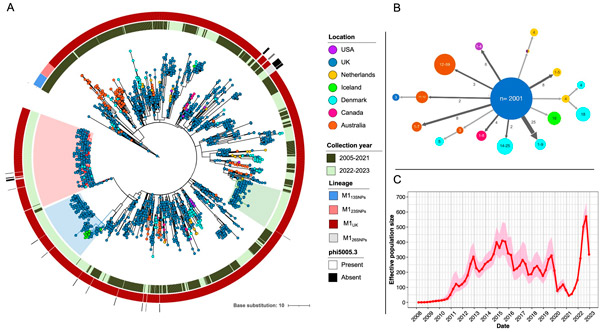
Global distribution and potential introduction events of M1UK and intermediate populations. A Phylogenetic tree of 2,364 M1UK and intermediate strains collected worldwide from March 2005 to July 2023. B Simplified transmission tree generated with PastML showing the location of the ancestral epidemic origin of M1UK lineages and intermediate populations. C Estimated effective population size (Ne) of M1UK in the UK over time. Nature Communications (2024). DOI: 10.1038/s41467-024-47929-7
Using genetic sequencing of patient samples combined with computer modeling, they found that M1UK likely emerged around 2008 and began to increase gradually from 2010 onwards.
Compared with earlier M1 strains, which have remained relatively unchanged over the past 40 years, M1UK produces more of the toxins that cause scarlet fever.
Professor Shiranee Sriskandan, from Imperial College London’s Department of Infectious Diseases, who led the study with colleagues from the UKHSA, said: “Bacteria evolve over time and because Strep A is a strictly human pathogen, it acquires genetic changes as it spreads through the population. Most variants come and go over time, but M1UK now appears to be well established in the UK and other countries. Whether this will remain the case in the long term is unknown.”
Genetic history
Using a search of global genomic databases, the team showed that when M1UK was first detected in the UK in 2019, only two M1UK strains could be identified from genomic sequences outside the UK. But subsequent analysis from other countries, examining changing trends in Strep A infections (including invasive infections), shows that M1UK is now present in more than 10 countries worldwide and has in some cases become the dominant strain post-pandemic.
The analysis also highlights a bottleneck effect, with Strep A infections declining during the COVID-19 pandemic, coinciding with widespread social distancing measures and lockdowns. But after this period, M1UK spread rapidly in the UK, with a marked increase in scarlet fever and invasive Strep A infections in 2022.
According to the researchers, while reduced transmission of Strep A during the pandemic may have led to weakened immunity in the population, their work highlights genetic features of M1UK that indicate a survival advantage over other strains, allowing it to spread more easily and potentially cause more severe disease. It is possible that increased population immunity to the M1UK strain could allow other types of strains to emerge.
Professor Sriskandan, also clinical director of the Centre for the Biology of Bacterial Resistance, added: “While we now know that the M1UK variant was responsible for the significant increase in cases last winter, this occurred at an unusual time of year, coinciding with respiratory viruses and winter stress, which all impacted on severity. Ultimately, the spikes we are seeing at different times around the world are likely to be due to reduced immunity to certain respiratory pathogens, particularly Strep A. Vaccines could help prevent this, and we really need a vaccine against Strep A. These latest findings from our study have been made possible by close collaboration between infectious disease researchers at Imperial College and the UK Health Protection Agency’s world-leading molecular surveillance system.”
