Medical expert of the article
New publications
Chorioamnionitis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
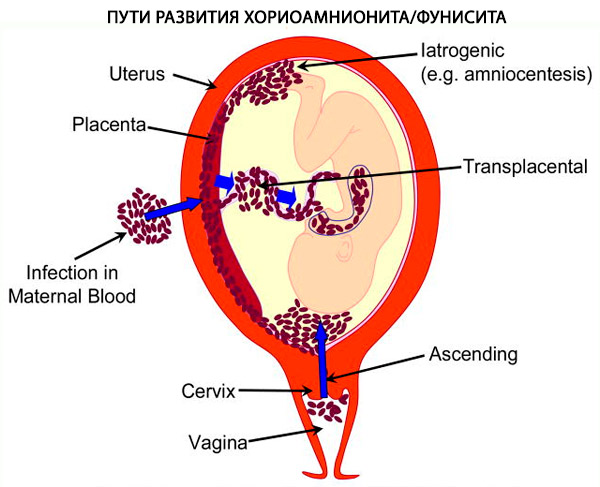
Chorioamnionitis or intra-amniotic infection is an acute inflammation of the membranes and chorion of the placenta, usually caused by an ascending polymicrobial bacterial infection secondary to rupture of the membranes. Chorioamnionitis can occur with intact membranes, and this appears to be particularly true with genital mycoplasmas such as Ureaplasma and Mycoplasma hominis, which are found in the lower genital tract of more than 70% of women. [ 1 ] Only rarely is chorioamnionitis accompanied by hematogenous dissemination, as occurs with Listeria monocytogenes. [ 2 ] When characteristic clinical features are present, the condition is called clinical chorioamnionitis or clinical intra-amniotic infection. Although there is considerable overlap between clinical and histologic chorioamnionitis, the latter is the more common diagnosis based on pathologic findings on microscopic examination of the placenta, which includes clinically asymptomatic (subclinical) chorioamnionitis as well as clinical chorioamnionitis.[ 3 ]
In general, the definition of chorioamnionitis varies depending on the key diagnostic criteria, which may be clinical (presence of typical clinical manifestations), microbiological (microbial culture from appropriately collected amniotic fluid or chorioamnion), or histopathological (microscopic evidence of infection or inflammation on examination of the placenta or chorioamnion).
Epidemiology
Chorioamnionitis occurs in approximately 4% of term deliveries, but is more common in preterm labor and preterm premature rupture of membranes. In women with symptoms of chorioamnionitis, studies show a strong correlation between histologic chorioamnionitis and key clinical symptoms such as fever, uterine tenderness, meconium aspiration syndrome, and foul-smelling vaginal discharge.[4 ],[ 5 ] Histologic chorioamnionitis with vasculitis is associated with a higher incidence of preterm premature rupture of membranes and preterm labor.[ 6 ]
In deliveries at 21–24 weeks of gestation, histological chorioamnionitis is detected in more than 94% of cases. [ 7 ] Chorioamnionitis in preterm labor may result in preterm labor. Studies show that placental inflammation or chorioamnionitis can be detected in approximately 8–50% of preterm deliveries. [ 8 ], [ 9 ] At the gestational age, chorioamnionitis is most likely associated with labor and a history of prolonged rupture of membranes.
Causes chorioamnionitis
The infection may be caused by bacterial, fungal, or viral agents. Bacterial agents of chorioamnionitis may vary depending on geographic location and population. Common bacterial agents found in chorioamnionitis include group B streptococcus, Mycoplasma pneumoniae (30%), [ 10 ] Ureaplasma (47%), Gardnerella vaginalis (25%), Escherichia coli (8%), and Bacteroides (30%). [ 11 ]Candida species have been identified as risk factors for chorioamnionitis leading to preterm labor and adverse fetal outcomes. [ 12 ], [ 13 ]
Studies show that in adolescents with sexually transmitted infections, trichomoniasis is a risk factor for developing chorioamnionitis. Although chorioamnionitis is a risk factor for vertical transmission during pregnancy, maternal HIV status is not a risk factor for developing chorioamnionitis. In one study of 298 women with similar risk factors and demographic characteristics, both groups of women had a high incidence of chorioamnionitis. The higher incidence in each group was strongly associated with the number of vaginal examinations during labor.[ 14 ]
Pathogenesis
Chorioamnionitis is an ascending infection that originates in the lower genitourinary tract and migrates into the amniotic cavity. The infection usually originates from the cervix and vagina. Vertical transmission has been reported with bacterial and viral infections transmitted to the fetus.
Histopathology
Chorioamnionitis is an inflammatory process that ranges from mild to severe. Histopathologic findings consistent with inflammation may also be present in placentas from women with normal pregnancies.[ 15 ]
In chorioamnionitis, the membranes may appear normal or show signs of infection. The fluid may be clear or cloudy. Histological examination reveals neutrophilic infiltration in the decidua and, in more severe cases, microabscesses. A recent study suggests that neutrophils in the amniotic cavity are mostly of fetal origin. In extremely preterm infants, maternal and fetal neutrophils are more frequently present in the amniotic cavity in chorioamnionitis.[ 16 ]
Symptoms chorioamnionitis
Chorioamnionitis presents as a febrile illness associated with elevated white blood cell (WBC) counts, uterine tenderness, abdominal pain, foul odor. vaginal discharge, and fetal and maternal tachycardia. The diagnosis of clinical chorioamnionitis includes a fever of at least 102.5°F (39°C) or 102.5°F (38°C to 102.5°C) for 30 minutes and one of the clinical symptoms. Most women with chorioamnionitis go on to labor or have rupture of membranes.
Complications and consequences
Neonatal complications of chorioamnionitis include preterm birth, cerebral palsy, retinopathy of prematurity, neurologic deficits, respiratory distress syndrome, bronchopulmonary dysplasia of prematurity, neonatal sepsis, and neonatal mortality. Neonatal sepsis is suspected as a complication of chorioamnionitis; however, cultures are negative in >99% of cases. Perinatal listeriosis is associated with significant morbidity. Current antibiotic regimens may not cover listeriosis in chorioamnionitis.
Maternal complications of chorioamnionitis include severe pelvic infections, subcutaneous wound infections, preterm labor, postpartum hemorrhage, operative delivery, and maternal sepsis.
Chorioamnionitis is associated with vertical transmission of HIV during pregnancy.[ 17 ],[ 18 ]
Diagnostics chorioamnionitis
The initial history should include maternal age, gestational age, parity, pregnancy milestones including any complications, rupture or intactness of membranes, presence of meconium, presence or history of sexually transmitted infections, urinary tract infections, and recent illnesses. The physical examination should be thorough and include vital signs and a complete physical examination including the abdomen, vagina, and uterus.
Amniotic fluid testing, usually obtained by amniocentesis, is used to diagnose chorioamnionitis.[ 19 ],[ 20 ],[ 21 ] Amniotic fluid culture is the most reliable test, but its usefulness is limited because culture results may not be available for 3 days.
Who to contact?
Treatment chorioamnionitis
The mainstay of treatment for chorioamnionitis is antibiotic therapy. The most common antibiotics are ampicillin and gentamicin. Alternative antibiotics include clindamycin, cefazolin, and vancomycin in women withpenicillin allergy. After delivery, it is currently recommended to give one additional dose by cesarean section, but not additional antibiotics for vaginal delivery. Depending on the clinical status, additional broad-spectrum antibiotics may be required.[ 22 ]
Forecast
Chorioamnionitis is a risk factor for both the mother and the newborn. Endometritis may occur in one third of women treated for chorioamnionitis and undergoing cesarean section. The incidence of endometritis is similar in vaginal and cesarean deliveries after chorioamnionitis. Recent studies show that postpartum antibiotics do not reduce the risk of endometritis after chorioamnionitis. [ 23 ]
Most women with chorioamnionitis recover and do not require additional antibiotics after delivery.
Sources
- Ohyama M, Itani Y, Yamanaka M, Goto A, Kato K, Ijiri R, Tanaka Y. Re-evaluation of chorioamnionitis and funisitis with a special reference to subacute chorioamnionitis. Hum Pathol. 2002 Feb;33(2):183-90.
- Bennet L, Dhillon S, Lear CA, van den Heuij L, King V, Dean JM, Wassink G, Davidson JO, Gunn AJ. Chronic inflammation and impaired development of the preterm brain. J Reprod Immunol. 2018 Feb;125:45-55.
- Miyano A, Miyamichi T, Nakayama M, Kitajima H, Shimizu A. Differences among acute, subacute, and chronic chorioamnionitis based on levels of inflammation-associated proteins in cord blood. Pediatr Dev Pathol. 1998 Nov-Dec;1(6):513-21.
- Kim CY, Jung E, Kim EN, Kim CJ, Lee JY, Hwang JH, Song WS, Lee BS, Kim EA, Kim KS. Chronic Placental Inflammation as a Risk Factor of Severe Retinopathy of Prematurity. J Pathol Transl Med. 2018 Sep;52(5):290-297.
- Palmsten K, Nelson KK, Laurent LC, Park S, Chambers CD, Parast MM. Subclinical and clinical chorioamnionitis, fetal vasculitis, and risk for preterm birth: A cohort study. Placenta. 2018 Jul;67:54-60.
- Bierstone D, Wagenaar N, Gano DL, Guo T, Georgio G, Groenendaal F, de Vries LS, Varghese J, Glass HC, Chung C, Terry J, Rijpert M, Grunau RE, Synnes A, Barkovich AJ, Ferriero DM, Benders M, Chau V, Miller SP. Association of Histologic Chorioamnionitis With Perinatal Brain Injury and Early Childhood Neurodevelopmental Outcomes Among Preterm Neonates. JAMA Pediatr. 2018 Jun 01;172(6):534-541.
- Garcia-Flores V, Romero R, Miller D, Xu Y, Done B, Veerapaneni C, Leng Y, Arenas-Hernandez M, Khan N, Panaitescu B, Hassan SS, Alvarez-Salas LM, Gomez-Lopez N. Inflammation-Induced Adverse Pregnancy and Neonatal Outcomes Can Be Improved by the Immunomodulatory Peptide Exendin-4. Front Immunol. 2018;9:1291.
- Huber BM, Meyer Sauteur PM, Unger WWJ, Hasters P, Eugster MR, Brandt S, Bloemberg GV, Natalucci G, Berger C. Vertical Transmission of Mycoplasma pneumoniae Infection. Neonatology. 2018;114(4):332-336.
- Rivasi F, Gasser B, Bagni A, Ficarra G, Negro RM, Philippe E. Placental candidiasis: report of four cases, one with villitis. APMIS. 1998 Dec;106(12):1165-9.
- Maki Y, Fujisaki M, Sato Y, Sameshima H. Candida Chorioamnionitis Leads to Preterm Birth and Adverse Fetal-Neonatal Outcome. Infect Dis Obstet Gynecol. 2017;2017:9060138.
- Newman T, Cafardi JM, Warshak CR. Human immunodeficiency virus-associated pulmonary arterial hypertension diagnosed postpartum. Obstet Gynecol. 2015 Jan;125(1):193-195.
- Suzuki S. Association between clinical chorioamnionitis and histological funisitis at term. J Neonatal Perinatal Med. 2019;12(1):37-40.
- Kim B, Oh SY, Kim JS. Placental Lesions in Meconium Aspiration Syndrome. J Pathol Transl Med. 2017 Sep;51(5):488-498.
- Kim CJ, Romero R, Chaemsaithong P, Chaiyasit N, Yoon BH, Kim YM. Acute chorioamnionitis and funisitis: definition, pathologic features, and clinical significance. Am J Obstet Gynecol. 2015 Oct;213(4 Suppl):S29-52.
- Perkins RP, Zhou SM, Butler C, Skipper BJ. Histologic chorioamnionitis in pregnancies of various gestational ages: implications in preterm rupture of membranes. Obstet Gynecol. 1987 Dec;70(6):856-60.
- Conti N, Torricelli M, Voltolini C, Vannuccini S, Clifton VL, Bloise E, Petraglia F. Term histologic chorioamnionitis: a heterogeneous condition. Eur J Obstet Gynecol Reprod Biol. 2015 May;188:34-8.
- Romero R, Kim YM, Pacora P, Kim CJ, Benshalom-Tirosh N, Jaiman S, Bhatti G, Kim JS, Qureshi F, Jacques SM, Jung EJ, Yeo L, Panaitescu B, Maymon E, Hassan SS, Hsu CD, Erez O. The frequency and type of placental histologic lesions in term of pregnancies with normal outcome. J Perinat Med. 2018 Aug 28;46(6):613-630.
- Gomez-Lopez N, Romero R, Xu Y, Leng Y, Garcia-Flores V, Miller D, Jacques SM, Hassan SS, Faro J, Alsamsam A, Alhousseini A, Gomez-Roberts H, Panaitescu B, Yeo L, Maymon E. Are amniotic fluid neutrophils in women with intraamniotic infection and/or inflammation of fetal or origin? Am J Obstet Gynecol. 2017 Dec;217(6):693.e1-693.e16.
- Musilova I, Pliskova L, Gerychova R, Janku P, Simetka O, Matlak P, Jacobsson B, Kacerovsky M. Maternal white blood cell count cannot identify the presence of microbial invasion of the amniotic cavity or intra-amniotic inflammation in women with preterm prelabor rupture of membranes. PLoS One. 2017;12(12):e0189394.
- Saghafi N, Pourali L, Ghazvini K, Maleki A, Ghavidel M, Karbalaeizadeh Babaki M. Cervical bacterial colonization in women with preterm premature rupture of membrane and pregnancy outcomes: A cohort study. Int J Reprod Biomed. 2018 May;16(5):341-348.
- Committee Opinion No. 712: Intrapartum Management of Intraamniotic Infection. Obstet Gynecol. 2017 Aug;130(2):e95-e101.
- Shanks AL, Mehra S, Gross G, Colvin R, Harper LM, Tuuli MG. Treatment Utility of Postpartum Antibiotics in Chorioamnionitis Study. Am J Perinatol. 2016 Jul;33(8):732-7.
- Chi BH, Mudenda V, Levy J, Sinkala M, Goldenberg RL, Stringer JS. Acute and chronic chorioamnionitis and the risk of perinatal human immunodeficiency virus-1 transmission. Am J Obstet Gynecol. 2006 Jan;194(1):174-81.
- Ocheke AN, Agaba PA, Imade GE, Silas OA, Ajetunmobi OI, Echejoh G, Ekere C, Sendht A, Bitrus J, Agaba EI, Sagay AS. Chorioamnionitis in pregnancy: a comparative study of HIV-positive and HIV-negative parturients. Int J STD AIDS. 2016 Mar;27(4):296-304.

