Medical expert of the article
New publications
Candida fungi (candida) are the causative agents of candidiasis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Fungi of the genus Candida (Candida) cause superficial, invasive and other forms of candidiasis (candidomycosis). There are about 200 species of fungi of the genus Candida. Taxonomic relationships within the genus have not been sufficiently studied. Some representatives of the genus are deuteromycetes; sexual reproduction of which has not been established. Teleomorphic genera have also been identified, including representatives with sexual reproduction: Clavispora, Debaryomyces, Kluyveromyces and Fichia.
Clinically significant species are Candida albicans, C. tropicalis, C. catenulara, C. cijferrii, C. guilliermondii, C. haemulonii, C. kefyr (formerly C. pseudotropicaiis), C. krusei, C. lipolytica, C. lusitaniae, C. norvegensis, C. parapsilosis, C. pulherrima, C. rugnsa, C. utilis, C. viswanathii, C. zeylanoides, and C. glahrata. C. albicans is the most important species in the development of candidiasis, followed by C. glabrata, C. tropicali, and C. parapsilosis.
Morphology and physiology of candida
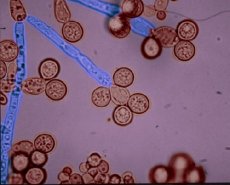
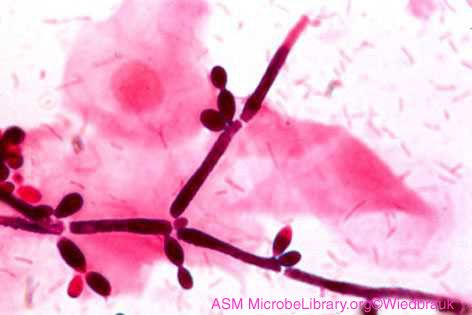
Fungi of the genus Candida consist of oval budding yeast cells (4-8 µm) pseudohyphae and septate hyphae. Candida albicans is characterized by the formation of a growth tube from a blastospore (bud) when placed in serum. In addition, Candida albicans forms chlamydospores - thick-walled, double-contoured large oval spores. On simple nutrient media at 25-27 °C, they form yeast and pseudohyphal cells. Colonies are convex, shiny, creamy, opaque with various honey fungi. In tissues, candida grows in the form of yeast and pseudohyphae.
Pathogenesis and symptoms of candidiasis
Candidiasis development is promoted by incorrect prescription of antibiotics, metabolic and hormonal disorders, immunodeficiencies, increased skin moisture, damage to the skin and mucous membranes. Candidiasis is most often caused by Candida albicans, which produces proteases and ingegrin-like molecules for adhesion to extracellular proteins and other virulence factors. Candida can cause visceral candidiasis of various organs, systemic (disseminated or candylasepticemia) candidiasis, superficial candidiasis of the mucous membranes, skin and nails, chronic (granulomatous) candidiasis, allergy to Candida antigens. Visceral candidiasis is accompanied by inflammatory lesions of certain organs and tissues (esophageal candidiasis, candidal gastritis, respiratory candidiasis, candidiasis of the urinary system). An important sign of disseminated candidiasis is fungal endophthalmitis (exudative change in the yellow-white color of the vascular membrane of the eye).
With oral candidiasis, an acute form of the disease (the so-called thrush) develops on the mucous membranes with the appearance of a white cheesy coating, atrophy or hypertrophy, hyperkeratosis of the papillae of the tongue may develop. With vaginal candidiasis (vulvovaginitis), white cheesy discharge, edema and erythema of the mucous membranes appear. Skin lesions often develop in newborns; small nodules, papules and pustules are observed on the trunk and buttocks. Candida allergy of the gastrointestinal tract, allergic damage to the organs of vision with the development of itching of the eyelids, blepharoconjunctivitis are possible.
Immunity
Cellular immunity prevails. Mononuclear phagocytes and neutrophils that capture fungal elements participate in the body's defense against Candida. DTH develops, granulomas with epithelioid and giant cells are formed.
Epidemiology of candidiasis
Candida is part of the normal microflora of mammals and humans. They live on plants, fruits, and being part of the normal microflora, they can invade tissue (endogenous infection) and cause candidiasis in people with weakened immune defenses. Less often, the pathogen is transmitted to children at birth, during breastfeeding. When transmitted sexually, urogenital candidiasis may develop.
Microbiological diagnostics of candidiasis
Smears from clinical material reveal pseudomycelium (cells connected by constrictions), mycelium with septa and budding blastospores. Sowings from the patient are carried out on Sabouraud agar, wort agar, etc. Colonies of C. albicans are whitish-cream, convex, round. Fungi are differentiated by morphological, biochemical and physiological properties. Candida species differ when growing on glucose potato agar by the type of filamentation: the location of glomeruli - clusters of small round yeast-like cells around the pseudomycelium. Blastspores of Candida albicans are characterized by the formation of germ tubes when cultivated in liquid media with serum or plasma (2-3 hours at 37 °C). In addition, chlamydospores are detected in Candida albicans: the sowing area on rice agar is covered with a sterile cover glass and after incubation (at 25 °C for 2-5 days) it is examined microscopically. Saccharomyces, unlike Candida spp., are true yeasts and form ascospores located inside the cells, stained using a modified Ziehl-Neelsen method; saccharomyces usually do not form pseudomycelium. The presence of candidemia is established by a positive blood culture with the isolation of Candida spp. Candidal urinary infection is established by detecting more than 105 colonies of Candida spp. in 1 ml of urine. Serological diagnostics (agglutination reaction, RSC, RP, ELISA), antibodies to Candida albicans in the blood and a skin allergy test with Candida allergen can also be performed. Candida albicans antigen detection is also used.
Treatment of candidiasis
Treatment of candidiasis is based on the use of such drugs as: nystatin, levorin (for the treatment of local superficial mycoses, such as oropharyngeal), clotrimazole, ketoconazole, caspofungin, itraconazole, fluconazole (not effective against C. krusei and many strains of C. glabrata).


 [
[