Medical expert of the article
New publications
Cocci in a smear: treatment
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
In modern medicine, there is an increasing need to conduct smears and bacteriological studies. This is explained by the fact that the share of diseases of bacterial etiology is sharply increasing. But often, even having determined the species composition and quantity of microflora, this is not enough to make a diagnosis and select treatment. Difficulties arise due to the fact that along with pathogenic flora, there is also normal microflora in the human body, which provides protection for the body. One example is cocci in a smear, which are found in the tests of every healthy person.
Cocci in a smear in women
Vaginal microbiocenosis is very important for a woman's health. It contains approximately 10% of the microflora of the entire female body and plays a leading role in maintaining health. Its importance lies in the fact that it determines the health of not only the woman, but also the newborn child. Violation of normal vaginal microflora entails not only an increase in gynecological diseases, but also an increase in neonatal and pediatric morbidity and mortality.
The basis of a woman's microflora is formed by anaerobic microorganisms. These are mainly lactobacilli, bifidobacteria and propionobacteria. Also included in this group are eubacteria, clostridia, bacteroids, peptococci. Together, they form an obligate microflora, which provides reliable protection of the woman's urogenital tract from the introduction of pathogenic microflora (they provide colonization resistance of the mucous membrane).
In addition to the obligate microflora, there is also indigenous or facultative microflora, which is represented by opportunistic forms of microorganisms. Quite a large percentage here is given to cocci. Streptococci, staphylococci, enterococci, aerococci and other microorganisms predominate. This means that under normal physiological conditions of the body, their number is insignificant and does not exceed 3-4%. This flora, along with the obligate flora, provides reliable protection against pathogens, stimulates the immune system. But with a decrease in immunity and the development of an inflammatory process, as well as with a decrease in the activity of the obligate flora, the opportunistic flora begins to grow actively, filling all the free space of the mucous membrane, integuments. In this case, they act as pathogens of infectious diseases.
Diseases are determined by which microorganism has become sharply predominant and quantitatively exceeded the norm. With the prevalence of cocci, severe infectious and inflammatory diseases of internal organs begin to develop: bacterial vaginosis, genitourinary infections, pyelonephritis, salpingitis, chorioamnionitis.
Cocci cause postoperative complications, postpartum fever, and other complications, neonatal infections, sepsis, peritonitis. Cocci are one of the most dangerous forms of hospital-acquired infection, which is not treatable and has an extremely high degree of resistance to drugs and disinfectants.
The composition of the microflora is relatively constant, formed evolutionarily. But under the influence of various factors, changes may occur in it. The composition and quantity of microflora can be affected by the anatomical structure, features of the hormonal background, specifics of blood and lymph circulation. As a result of taking certain medications, including antibiotics, serious changes may occur.
The formation of a woman's microbiocenosis begins at the moment of birth. Already during the first day of life, the initially sterile vagina is colonized by maternal microflora. This is why it is so important for a woman to maintain the health and normal microecological state of her reproductive organs. The flora that is formed is mainly dominated by lactobacilli and bifidobacteria. Then the number of these microorganisms decreases, and until puberty it is in a state of equilibrium with other microorganisms, or coccal forms of bacteria begin to actively multiply and predominate. This significantly increases the risk of contracting urogenital infections through everyday life.
After the girl reaches puberty, there is a surge in estrogen activity, resulting in an increase in the epithelial layer and the amount of glycogen. From this moment on, the leading position is again occupied by lactic acid flora, which provides colonization resistance and protection of the woman's body from pathogens.
When there are disturbances in the body, dysbacteriosis develops, in which opportunistic flora begins to prevail over obligate flora, which causes infectious diseases and inflammatory processes. Particularly negative conditions and a high risk of dysbacteriosis develop during menstruation, when hormonal levels change, the amount of glycogen decreases sharply and, accordingly, optimal conditions for the development of opportunistic microflora and the suppression of obligate flora develop. Microflora also changes during pregnancy, during the postmenopausal period, since intensive hormonal changes occur in the body.
Cocci in a smear during pregnancy
In the body of a pregnant woman, optimal conditions are created for the development of obligate microflora. This occurs due to the active "estrogen explosion", which promotes the development of microorganisms of the lactobacilli and bifidobacteria groups. It is interesting that the normalization of microflora occurs not only in the vaginal biotope, but also in all others, especially in the intestines, oral cavity, skin. It is for this reason that the structure of hair, skin, and nails improve in a healthy woman during pregnancy. Maintaining optimal microflora is necessary to protect the child by preventing the development of intrauterine infections, as well as infection during passage through the birth canal. Termination of pregnancy sharply reduces the colonization resistance of the mucous membrane, so pathogenic microflora actively develops. This leads to the development of infectious and inflammatory processes.
The protective properties and colonization resistance of microflora decrease sharply during childbirth, as well as in the early postpartum period. At this time, the protective properties are minimal, so the woman is most at risk of developing an infection. Particularly dangerous during this period are hospital strains of microorganisms, which quite quickly infect a weakened organism, cause severe pathologies, and are practically not amenable to treatment with antibiotics, antibacterial drugs. Very often leads to bacteremia, sepsis, and can even have a fatal outcome. Restoration of normal microflora occurs by the end of the 5-6 week of the postpartum period.
Cocci in a smear in men
In men, propionic acid bacteria and bifidobacteria normally predominate, which form obligate microflora. It provides colonization resistance of mucous membranes and prevents the development of pathogenic flora. The body also contains indigenous microflora, which is represented by opportunistic forms. They can be activated and colonize the mucous membrane with reduced immunity and insufficient activity of obligate microflora.
Indigenous microflora is represented mainly by coccal forms. Among them, streptococci, staphylococci, and enterococci predominate. Normally, the indicators should not exceed 10 3 CFU/ml. If the amount of indigenous microflora goes beyond this indicator, a bacterial infection may develop, which depends on the type of microorganism. Coccal forms can provoke various infectious, inflammatory, purulent-septic infections, and even sepsis, which often ends in death.
 [ 12 ]
[ 12 ]
Cocci in a smear in a child
Cocci in a smear in fairly large quantities can be found in various biotopes of a newborn, and this is the norm. This is due to the fact that in the first day of life, all the cavity organs of a child remain relatively open. All of them, including the large and small intestines, contain a high amount of oxygen. This creates optimal conditions for the accumulation of aerobic microflora. This is also facilitated by the immaturity of the immune system. It must be remembered that aerobic flora is conditionally pathogenic, which means that at this time the child is most susceptible to the risk of developing pathogenic microflora, which can lead to an infectious process and sepsis.
The first 7-10 days after birth can be characterized as a period of transient dysbiosis, during which active development of aerobic microflora occurs, as well as intensive colonization of the skin and mucous membranes. At this time, protective mechanisms are also formed, which are strengthened by mother's milk. More favorable conditions for the development of anaerobic flora are gradually formed.
Gradually, anaerobic microflora begins to form. This leads to a decrease in its oxidation-reduction potential. By the end of the first week of life, the acidity of gastric juice increases significantly, the synthesis of autoantibodies and immune complexes increases. Later, pre-epithelial biofilms are formed, which are the main reservoir of human autoflora. The duration of the process of pre-epithelial biofilm formation has not been precisely determined. This process is slow and depends on many factors, primarily the health of the mother, the quality of her breast milk, and the ecology of the external environment.
It is known that in a newborn, the prevalence of physiological microflora in the large intestine, primarily bifidobacteria, begins to be noted before the end of the early neonatal period, that is, approximately on the 7th day after birth. But at present, fairly high concentrations of accompanying microflora are recorded over several months and even 2-3 years of a child's life.
In parallel with the formation of intestinal microflora, the microflora of the epithelium and skin is also formed. The trigger for its formation is breastfeeding in the early period. First of all, the child receives lactobacilli. Their populations quite quickly form a biotope, gradually reducing the amount of oxygen. These conditions are more suitable for bifidobacteria and propionic acid bacteria, which begin to grow. This is the second layer of microflora.
It is followed by the third layer, which is formed by lactobacilli. They stimulate cell wall receptors, activate pre-epithelial microflora, resulting in the formation of a matrix of biological structure, which contains mucin and other active enzymes, exopolysaccharides. Optimal conditions for symbiotic microflora are formed.
In the composition of the microflora of a healthy child, the level of opportunistic pathogenic forms, which are represented mainly by coccal forms, does not exceed 5%. The inclusion of a small number of pathogens in the composition of the child's microbiota is inevitable, due to their high content in the environment. But the physiological flora dominates, which prevents the development of pathology.
Consequences and complications
The prevalence of cocci in the smear leads to the development of an infectious process. Various diseases of internal organs, skin, inflammatory, purulent-infectious processes occur. The most dangerous conditions are peritonitis, bacteremia, sepsis, which are life-threatening conditions and can end in death.
Serious consequences include various postoperative complications, postpartum infections, infection of the newborn, catheter-associated infections, and wound infections. Particularly dangerous are hospital strains of cocci that have acquired multiple resistance and are practically untreatable.
 [ 13 ], [ 14 ], [ 15 ], [ 16 ]
[ 13 ], [ 14 ], [ 15 ], [ 16 ]
Why are cocci in a smear dangerous?
Normally, cocci are always found in a smear, since they are representatives of normal human microflora. If the indicators do not exceed the norm, cocci do not pose a danger, on the contrary, they perform a protective function in the body, preventing infection with other pathogenic microorganisms. The danger arises when their number exceeds the norm - becomes more than 103 CFU / ml. In this case, various infectious, purulent, inflammatory diseases occur.
The most dangerous complication of coccal infection is sepsis, in which the infection from the focus penetrates into the blood, and with the blood flow is carried throughout the body, infecting other organs, forming new foci. Sepsis requires urgent measures, immediate antibacterial therapy, otherwise a fatal outcome is possible.
No less dangerous are such conditions as bacteremia, septicemia, in which there is a small and moderate amount of cocci in the blood and other normally sterile fluids. The danger is that at this stage the disease progresses very quickly and in a few hours can turn into sepsis and end in death.
Can cocci be transmitted to a partner?
If one of the partners has an increased cocci count and an active inflammatory process, pathogenic microflora can be transmitted to the partner. Whether or not a disease will develop as a result depends on the state of the immune system and the general endurance of the body. If the immune system is normal and the general condition of the body is satisfactory, most likely there will be no disease. This is due to the fact that the partner's own microflora has a fairly high colonization resistance, which will not allow foreign microflora to penetrate the biotope.
If the immunity is lowered, the body is weakened, a bacterial infection may well develop, since the protective activity and colonization resistance of one's own microflora are at a very low level. This will allow foreign microflora to penetrate the biotope, as a result of which symptoms of the disease may appear.
Differential diagnostics
Implies the need to clearly differentiate the pathogen: to prove that the cause of the disease is precisely the high concentration of cocci. For this, a regular smear or a complete bacteriological study is carried out.
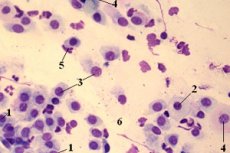
This will require biological material from the biotope being studied. Thus, in case of respiratory diseases, a smear is usually taken from the nose and throat, in case of urogenital infections - a smear from the vagina or urethra, etc. Then the smear is applied to a glass slide, dried over a burner, or fixed by chemical methods and examined by microscopy.
If necessary, additional staining is performed, which allows for a clear differentiation of various structures. To identify cocci, the Gram staining method is most often used. In this case, the cocci acquire a bright purple color and are clearly visible in the field of view under a microscope. Their morphology and main characteristics can be studied.
Often, in order to obtain more detailed information about the culture isolated during microscopy, bacteriological seeding is performed. For this, the resulting culture is sown on an artificial nutrient medium and incubated under optimal conditions for 3-5 days. After this, the culture is removed, reseeded in order to isolate a pure culture (pathogen), and incubated again. Then the grown colonies are analyzed, and qualitative and quantitative analysis is performed. Using a number of biochemical and immunological methods, the culture is identified using Bergey's identifier. Then the concentration of cells in 1 milliliter of suspension is determined using any convenient method. Most often, the serial dilution method or turbidity standard is used.
If the smear is good, can there be an infection?
Any good smear always contains the entire set of microorganisms that are characteristic of a given biotope. The quantity must correspond to the norm. That is, the analysis results will indicate a list of representatives of normal microflora and their quantity. A good smear means that obligate microflora prevails over opportunistic microflora, and any other microorganisms are absent.
Single microorganisms are allowed as representatives of transient (accidentally introduced) microflora. This means that there is no infection, since colonization resistance and immune mechanisms are at a high enough level to resist infection.
Treatment
If cocci are found in the smear, within the normal range, treatment is not required. If their number significantly exceeds the norm, antibiotic therapy may be required. Homeopathic, folk remedies, and herbal medicine are also used. When choosing a treatment method, you should consult a doctor and rely on the test results. With a moderate number of cocci and severe dysbiosis, it is advisable to use probiotics or prebiotics.
Medicines
When treating cocci, it is necessary to observe the basic precaution - to start treatment only after a preliminary consultation with a doctor. The doctor is also insured - he must prescribe treatment only on the basis of test results.
If antibiotic therapy is assumed, it is advisable to conduct an antibiotic sensitivity test and use it to select the most effective drug and its optimal dosage. The consequences and side effects of improper medication intake can be disastrous - worsening of the situation, development of serious dysbacteriosis affecting deep microbiocenoses, development of bacterial infection. It is better to start treatment with probiotics, which act gently, normalizing the microecological state of the body.
For the treatment and prevention of intestinal dysbacteriosis, coccal infection, it is recommended to take Bifilact-Extra 1 capsule per day. The capsule contains bifidobacteria and lactobacilli, as well as auxiliary substances.
For intestinal infections, diarrhea, flatulence, and also as part of complex therapy in the treatment of acute inflammatory and allergic diseases, use Bifi-Form, 1 capsule.
For the treatment and prevention of vaginal dysbacteriosis and other diseases of the female genitourinary system, bifolak is used in the form of suppositories. It is used at night, intravaginally, 1 suppository.
Emulact ointment is used externally for various skin diseases. Contains a stabilized culture of lactobacilli. It is used for dermatitis, any other skin diseases, dysbiosis. Apply a thin layer to clean skin.
Antibiotics for cocci in smear
Antibiotics are widely used to treat cocci, especially if their concentration is high enough. Ciprofloxacin has proven itself to be effective today - 500 mg once a day for three days. It quickly eliminates all symptoms of bacterial infection and normalizes the level of cocci. Other antibiotics act in a similar way: amoxiclav, amoxicillin, azithromycin, azitrok, penicillin.
An Indian company offers a new drug that combines an antibiotic and a probiotic. The antibiotic kills pathogenic microflora, the probiotic immediately restores normal flora, which is also damaged. The composition includes 250 mg of amoxicillin and cloxacillin, as well as 60 million microbial bodies of lactobacilli. It is taken for diseases of bacterial etiology of any localization.
Candles from cocci in smear
If the pathology is not systemic, i.e. does not affect the entire body, taking antibiotics orally is not recommended. It is better to use suppositories. They allow you to quickly and effectively eliminate the pathology locally. At the same time, the risk of side effects and overdose is reduced to a minimum. Suppositories should be prescribed only by a doctor. Depending on the pathology, they are used rectally or intravaginally. Usually, the course of treatment is from 3 to 14 days. Antibiotics or probiotics are most often used.
 [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ]
[ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ]
Folk remedies
Aloe juice is widely used to treat coccal infection. To do this, take 2-3 juicy fleshy leaves, squeeze out the juice, and apply internally or locally, depending on the localization of the pathology. Take internally in pure form, 1 tablespoon, or dilute in a glass of warm water.
Honey has also been used against infections at all times. It has an antiseptic effect. For respiratory diseases, honey is added to tea or herbal infusions, compresses and lotions are made from honey. It is used for massages and wraps. Using honey in its pure form, a tablespoon in the morning and evening, will help eliminate the infection.
Mumiyo is good for external and internal infections. It should be diluted in a liter of water and drunk in a glass in the morning, before you get out of bed. After drinking, you need to lie down for another 40 minutes, only then can you get up.
 [ 32 ], [ 33 ], [ 34 ], [ 35 ]
[ 32 ], [ 33 ], [ 34 ], [ 35 ]
Herbal treatment
The most famous herb that has anti-infective and anti-inflammatory effects is chamomile. It is used as a decoction or infusion. The difference is that the infusion is prepared with alcohol or vodka, it is more concentrated and rich, contains more active components, so its dosage is required lower than for a decoction. The infusion is infused longer - up to 7 days, while the decoction is ready in 1-2 hours. You need to drink the infusion by the tablespoon, while the decoction - up to a glass per day. The infusion can be stored for up to a year, the decoction - no more than a day.
Calendula has an antiseptic effect. It is used as a decoction: a tablespoon of the herb per glass of boiling water. Infuse for 30 minutes and drink during the day. The result is usually noticeable within 1-2 days.
Fennel decoction has proven itself to be effective against intestinal infections. To prepare it, pour a glass of water over a third of a teaspoon of the seed and drink a third of a glass three times a day.
Homeopathy
It is important to take precautions - do not take any medicine without first consulting a doctor. Homeopathic medicines have side effects only if the medicine is taken incorrectly or in case of overdose. Usually, the condition worsens.
Vitaflor is a biologically active supplement, which is represented by two strains of lactobacilli. It is used for dysbacteriosis, with a lack of lactobacilli and a predominance of cocci, 1 capsule per day.
Vitasporin is a spore probiotic, which includes a complex of bacillary forms of microorganisms. It is used for staphylococcal and other coccal infections, 1 capsule per day.
Gastrofarm is a probiotic containing the main representatives of normal intestinal microflora. It is used for infections and dysbacteriosis. Take one tablet per day.
Enterol is used for acute and chronic diarrhea, enteritis. It is available in sachets. Take one sachet 2-3 times a day. Contains lyophilized saccharomyces.
Prevention
Microbiocenosis disorders have serious consequences for the population. It should be taken into account that most women in labor, even with a normal pregnancy and childbirth, have deviations in the microbiocenosis, expressed to a greater or lesser extent. This inevitably affects the health of the newborn. Therefore, the widespread disbiosis among the population in recent years is largely associated with primary microecological defects that arose during the formation of microbial ecosystems in newborns. Defective biofilms and microbial associations are initially formed in the body, which are unable to perform physiological functions.
Analysis of the patterns of primary formation and further functioning of microbial biocenoses of the child's body leads to the conclusion that it is necessary to implement and carry out special measures to prevent dysbacteriosis. First of all, the solution is seen in the elimination of those factors that contribute to the development of pathology. It has been established that primary disorders lie primarily in the obstetric and gynecological chain. It is necessary to increase the effectiveness of therapeutic and preventive measures to prevent pathological changes in the endomicroecology of pregnant women, women in labor, and women in labor.
It is also important to maintain the culture of communication between mother and child: timely attachment to the breast, breastfeeding, correct and constant contact between mother and child. In third place is compliance with sanitary and hygienic norms and requirements.
It is also necessary to ensure adequate correction of existing dysbiotic disorders, apply rational treatment regimens, use preliminary preparation of pregnant women, targeted colonization of biotopes of children at risk, reduce the use of antibiotics and other antibacterial drugs, and, if necessary, use probiotics and prebiotics.
Forecast
If cocci are detected in a smear in a timely manner, or rather their high concentration, measures can be taken to prevent the development of a bacterial infection. Complex treatment is required, selected by a doctor based on the test results. If the increased number of cocci is ignored, the prognosis may be unfavorable. A bacterial infection may develop, which tends to progress, up to sepsis with a fatal outcome.

