Medical expert of the article
New publications
Streptococci in smear in women, pregnancy, men and children
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
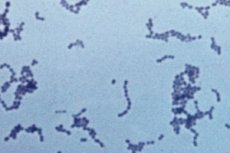
Streptococci are gram-negative microorganisms that are the causative agents of many purulent-infectious and inflammatory diseases. Streptococcus is almost always detected in a smear, but this does not mean that the person is sick. Everything depends on its concentration. If the amount of this microorganism exceeds the conditionally acceptable norms, the disease develops. A disease caused by streptococcal infection, according to ICD-10, belongs to the group of purulent and necrotic diseases.
Reasons for the appearance of streptococcus in a smear
Streptococcus appears in the smear due to the fact that it is a representative of opportunistic microflora. This means that it is a representative of the normal microflora of the body, which provides the protective properties of the body, provides colonization resistance of the mucous membranes, that is, prevents their colonization by pathogenic microorganisms. But under certain conditions, for example, with a decrease in immunity, a violation of the normal state of the mucous membranes, a violation of the normal ratio of microorganisms occurs. In this case, the concentration of streptococcus increases sharply, as a result of which it colonizes the mucous membranes of its biotope, and can even spread to other biotopes. As a result, the disease develops and progresses. This is an endogenous path of infection development.
But there is also an exogenous path of disease development, in which streptococcus enters from the external environment and then multiplies in the biotopes of the human body. How much the disease will progress depends on the state of the body. Here, the colonization resistance of the microflora, that is, the normal composition of the microflora, in which "there is no room" for foreign microorganisms, plays an important role.
In a normal state of microflora, it prevents the penetration of pathogenic microorganisms and does not allow the disease to develop. When penetrating from the external environment, it most often penetrates from carriers, which are people who are sick or have recovered from streptococcal infection.
Streptococcus, which persists in the external environment, can also be a source. Hospital strains of resistant streptococcus, which develop in the hospital environment, pose a particular danger in this regard. It has repeatedly undergone mutations under the influence of disinfectants and antiseptics. Therefore, it causes the most dangerous diseases that cannot be treated with standard antibiotics.
Norm of streptococci in smear
A smear normally contains up to 10 3 CFU/ml. This means that 1 milliliter of fluid contains no more than 10 to the third power, i.e. no more than 1000 colonies of microorganisms. If the number of streptococci exceeds these indicators, the disease develops.
Streptococci 10 to the 3rd - 10 to the 6th power in a smear
This means a degree that shows a quantitative measurement, the content of a certain number of colonies of microorganisms in 1 ml of the material being studied. In this case, the norm is considered to be the indicator of 10 3, which means that 1 ml of suspension contains 1000 colonies of streptococcus. Below this indicator is the norm, the indicator itself 10 to the power of 3 is considered a borderline state, from which the development of the disease begins. Above this indicator, a disease of streptococcal etiology certainly develops.
Risk factors
People with reduced immunity and impaired microflora are at risk for developing streptococcal infection. A significant risk factor is the entry of various toxic substances and radioactive components into the body, which undermine the body's defense mechanisms.
People who have recently undergone surgery, organ and tissue transplants, people suffering from chronic diseases, immunodeficiency, anemia, metabolic disorders, and vitamin deficiencies are at risk. Even poor nutrition, a sedentary lifestyle, frequent stress, exhaustion, and starvation can cause infection.
The risk group also includes people who often suffer from colds and other diseases, those who have built-in pacemakers, catheters (catheter-associated infection develops), prostheses, temporary and permanent transplants. The risk group includes people who are forced to stay in hospital or inpatient settings for a long period of time. They are exposed to hospital-acquired (hospital strains) microorganisms. Employees of medical institutions who, due to their job responsibilities, must come into contact with infectious patients are also at risk, and are exposed to hospital strains.
Symptoms
The main symptoms of streptococcal infection are the development of an inflammatory process in the affected area, as well as the progression of the infection. Then everything depends on which strain caused the development of the pathology, what is its concentration, and also on what biotope the infection has penetrated. Usually, the primary source of infection through which the infection enters the body is the upper respiratory tract and skin. When penetrating through the skin, a sequence of events develops - first, a superficial rash appears, redness and irritation of the skin. As the infection progresses and spreads, dermatitis (infectious inflammation of the skin - dermis) develops, then fasciitis can develop, in which the skin, fascia, ligaments are involved in the inflammatory process.
Myositis is an inflammatory process that develops with the involvement of the muscular layer in the inflammatory process. With deep penetration of the infection into the body, erysipelas may develop (erysipelas of the skin, muscular layers and bones, which is accompanied by suppuration, anaerobic processes, constant progression, involvement of new foci of inflammation).
Erysipelas is often accompanied by tissue necrosis (death). Therefore, to stop further spread of the infection, amputation of the organ (limb) is often required, which prevents further progression of the disease and avoids sepsis. The final stage is sepsis (blood poisoning), which can end in death.
When the infection penetrates through the respiratory tract, it mainly develops scarlet fever, follicular or lacunar tonsillitis, pneumonia, bronchitis, meningitis, osteomyelitis, septic arthritis,
The harbingers of the development of any infectious pathology are a feeling of weakness, increased fatigue, excessive sweating, rapid heartbeat that occurs when walking, minor physical and emotional stress. Then there is a burning sensation in the chest, pressure in the sternum, shortness of breath, shortness of breath. At this time, you can take preventive measures that will prevent the development of pathology. If such measures are not taken, the disease continues to progress, the temperature rises, fever, chills, headache appear, appetite decreases. In some cases, nausea and diarrhea occur. Further symptoms depend on the form and severity of the disease.
Streptococcus in a smear in men and women
Streptococcus in a urethral smear may indicate the development of a purulent-inflammatory or infectious disease in the urogenital tract. Thus, it may indicate the development of cystitis, pyelonephritis, urethritis, dysbacteriosis, and other forms of the disease.
The infection can enter the body endogenously (for example, if there is a chronic source of infection in the body) or exogenously (from the external environment, through contact with an infection carrier). Hospital strains, which can be contracted in a hospital setting, are particularly dangerous. Catheter-associated infections, which occur with prolonged use of a catheter, are also dangerous.
If the amount of streptococcus in a smear in women exceeds the permissible norm, treatment is required. If the content of this microorganism is equal to or below the norm, there is no need to worry. Only a doctor can prescribe treatment. Since self-medication can be dangerous to health, and even life. Incorrect treatment can disrupt the normal microbiocenosis, as a result of which other biotopes can be disrupted.
Streptococcus in a smear during pregnancy is a bad sign, since streptococcus can have a negative impact on the course of pregnancy. It often causes spontaneous abortions, miscarriages, premature births. It carries a risk for both the woman and the child. The danger is the risk of developing gestosis, infectious diseases, severe damage to the kidneys and liver, which entails miscarriage. Timely treatment of streptococcus will help avoid infection of the child during childbirth.
The most dangerous is considered to be intrauterine infection of the child, which may result in severe complications, underdevelopment of internal organs, various physical defects, deformities. If there is a smear, the doctor selects treatment from among those drugs that are approved for use during pregnancy. Treatment is carried out if the risk to the mother and child exceeds the harm from the effects of drugs. Self-medication is strictly contraindicated.
Streptococci in a child's smear
Detection of streptococcus in smears of newborns and premature babies is an alarming sign indicating that the child's immunity is not coping (and newborns retain their mother's immunity). Antibiotic therapy may be required to prevent such a severe condition as postpartum and neonatal sepsis, which ends in death. The main pathogen in neonatal infection is beta-streptococcus, which affects the skin and urogenital tract. Most often, it enters the newborn's body during childbirth. In 70% of cases, the source of infection is the mother.
Streptococcus is especially dangerous for newborns and young children, since their immunity is weakened and the microflora is at the stage of formation and development. The mortality rate is very high - from 25 to 75%.
In older children (over 3 years old), streptococcus most often causes severe diseases of the respiratory tract, genitourinary tract, gastrointestinal tract. When it gets into the blood, a secondary source of infection can develop. In 40% of cases, a skin infection occurs, in 30% - pneumonia. It should be taken into account that it often happens that the clinical picture is present, but the pathogen cannot be isolated. Possible complications are persistence, abnormal reaction, acute glomerulonephritis. The most dangerous are bacteremia, sepsis, infectious toxic shock.
Streptococcus in a smear from the throat, pharynx, nose
It is found in various respiratory diseases. The degree of colonization of microorganisms depends on the severity of the disease. It may indicate the development of infectious and inflammatory diseases such as pneumonia, bronchitis, tracheitis, tracheobronchitis. Requires antibiotic therapy. In this case, only a doctor can select the optimal treatment regimen. It is necessary to treat streptococcal infection, since it is dangerous due to complications. The most dangerous consequence of streptococcal infection is infectious toxic shock, sepsis. It can also cause the development of osteomyelitis, meningitis, and other life-threatening diseases.
Streptococcus is often found in a nasal smear. It is caused by the development of a purulent-infectious, inflammatory process in the throat, nasopharynx, and pharynx. It causes various invasive diseases. One of the most common causes of sinusitis.
Treatment is drug-based, antibiotic therapy is used. In the absence of adequate treatment, the infection spreads to other biotopes, including the entire nasopharynx, pharynx. Upper and lower respiratory tract. Dangerous complications include the penetration of infection up the ascending respiratory tract, its penetration into the brain, which is accompanied by inflammation of the myelin membranes of the brain, the development of meningitis. Complications such as acute rheumatoid fever, glomerulonephritis, complications in the kidneys, and the cardiovascular system are also dangerous.
If a high concentration of streptococcus is detected in a smear, it is necessary to contact a doctor as soon as possible and undergo treatment to prevent the disease from becoming chronic or to prevent its further spread and progression. Antibiotic therapy is most often used. It is necessary to strictly follow the doctor's recommendations, since if the treatment is incorrect, the therapy may not only be ineffective, but also the microorganisms will become resistant.
Streptococcus in a gynecological smear
Indicates the development of dysbacteriosis, in which the normal state of the microflora is disrupted. Usually, the number of representatives of the normal microflora is sharply reduced, while the number of pathogenic and opportunistic microflora increases. This leads to the development of inflammatory processes.
In female reproductive organs, streptococcus causes vaginitis, colpitis, vulvovaginitis. It can negatively affect the menstrual cycle, disrupting its regularity and duration. Reduces fertility, the ability to conceive and bear a child. It can also be transmitted from mother to child during childbirth.
- Streptococcus in vaginal smear
Normally, vaginal microflora contains a certain amount of opportunistic microflora, the number of which should not exceed the norm. At the same time, if the amount of normal microflora decreases, pathogenic microflora begins to grow, including streptococcus. It can also penetrate the body from the external environment. High adaptation of microorganisms to the vaginal microbiocenosis is noted, since staphylococcus easily penetrates the mucous membrane, using pathogenicity factors, as well as invasion factors.
The main invasive factors of streptococcus are capsules, antigen M and T, teichoic acids, which are part of the cell wall and provide adhesion factors. With the help of M-protein, intracellular invasion of the pathogen is carried out. Mandatory treatment is required, since streptococcus without treatment can develop into a chronic infection, which is much more difficult to treat with antibiotics and other available means. Approximately 30% of cases of chronic streptococcal infection treatment is ineffective due to the fact that the chronic infection is resistant.
- Streptococcus galactiae in a smear from the cervical canal
Leads to the development of an inflammatory process in the vagina, ovaries, disrupts the normal functioning of the fallopian tubes. Often leads to infertility, miscarriage. During childbirth, it can lead to infection of the child.
Hemolytic and non-hemolytic streptococci in smear
Hemolytic streptococcus is a form of streptococcus that causes lysis of blood components (hemolysis). Most often, hemolysis of erythrocytes occurs, which leads to a violation of the ratio between the number of erythrocytes and hemoglobin, promotes the release of free hemoglobin into the blood. Leads to the development of anemia. Often isolated in meningitis, endocarditis, sepsis. Isolation is carried out on blood agar, as a result of which the agar is destroyed. The source is a sick person, a carrier. The route of transmission is aerogenic, contact.
Non-hemolytic streptococcus is a type that does not cause hemolysis of blood. This form becomes the basis of infectious diseases, including diseases of the respiratory system, urogenital tract. It is treated with antibiotic therapy.
Streptococcus faecalis in smear
It is transmitted orally and faecally. It is excreted from the intestines of an infected person, enters the body through the oral cavity with food, dirty hands. It causes mainly diseases of the digestive tract, poisoning, kidney disease, liver, genitourinary tract. It often causes poisoning (internal intoxication, autointoxication). This leads to the fact that the infection and bacterial toxins quickly spread through the blood, forming new foci of infection. Another danger is that rapid colonization occurs, the infection quickly spreads throughout the body, and leads to the development of bacteremia, sepsis. It can cause severe poisoning, accompanied by intoxication, the development of dehydration, and disturbances in water-salt balance.
Streptococcus anginosus in a smear
It is a cluster of representatives of the genus streptococcus, which are the causative agent of tonsillitis. Most often, they cause the development of lacunar and lipofollicular tonsillitis, in which there is an accumulation of purulent mass in follicles or lacunae. It is accompanied by an intense inflammatory and infectious process.
First, adhesion (attachment) of the microorganism to the walls and mucous membranes of the throat and respiratory tract occurs. Then it multiplies, colonizes the respiratory tract, throat. This is accompanied by an inflammatory process, the peak of which occurs approximately on the 2-3 day. With follicular tonsillitis, follicles develop.
Approximately on the 3rd-4th day, the integrity of the follicles is compromised, and their contents fill the lacunae, forming a plaque. Lacunar tonsillitis develops. In addition, streptococcus in the process of its vital activity is capable of producing erythrocyte toxin, which causes intoxication of the body, spasm of the respiratory tract.
Requires treatment with antibiotics. Only a doctor can select a treatment regimen, since it is based on the results of laboratory tests. Before starting therapy, it is advisable to conduct an antibiotic sensitivity test, with the help of which you can select the optimal dosage of the drug, as well as select the drug that will be effective. This is due to the fact that streptococci can be resistant to many antibiotics. In addition, many of them have multiple resistance.
Epidermal streptococcus in smear
Indicates the development of skin diseases. May cause bacterial rash, skin dermatitis, and other skin and venereal diseases. Also often leads to the development of inflammation of the subcutaneous fat (cellulite). Can affect deeper layers of the skin, and even the muscle layer, causing the development of bursitis, fasciitis, myositis. With deep penetration, the toxin may enter the blood, resulting in bacteremia and sepsis. Capable of producing toxins that cause intoxication of the body. If left untreated, they can cause infectious toxic shock, sepsis (blood poisoning).
One of the most dangerous complications is erysipelas, which is a chronic recurrent disease that is accompanied by the development of fever and intoxication.
In this case, the inflammation focus and the area of skin infection are clearly limited. This is preceded by skin sensitization, damage to the integrity of the skin. Most often it develops in elderly people, in people with impaired blood and lymph flow, in people with reduced immunity.
It is severe, with severe intoxication and progression of the inflammatory process. Erosions and ulcers develop. The eroded area is populated by other microflora, in particular, anaerobic, which leads to progression of the infection. It often ends with amputation of the affected area, limb in order to prevent progression of the disease.
Streptococci viridans in smear
A representative of the normal microflora of the urogenital tract. Colonizes the female genital tract, and is found in smaller quantities in the male genitourinary system. An opportunistic microorganism, which, in conditions of reduced immunity and dysbacteriosis, primarily causes vaginitis, vulvovaginitis, colpitis, and other diseases of the female genitourinary system. As the disease progresses, the infection rises along the ascending genitourinary tract, which can result in cystitis, pyelonephritis, nephritis, and other diseases of the kidneys and bladder. Often, as a result of the progression of the infectious process and excessive proliferation of streptococci, new foci of infection develop. The most dangerous complication is sepsis.
Staphylococci and streptococci in a smear
Both microorganisms are representatives of normal human microflora and are characterized by the ability to cause disease if their numbers exceed the maximum permissible norms. It is worth noting that they normally live in many human biotopes and are factors of colonization resistance, that is, they provide resistance to pathogenic microorganisms.
They can cause diseases of the upper tract, or diseases of the genitourinary system, intestinal disorders. The most dangerous complication of both forms is sepsis and bacteremia. Both produce pathogenic factors, various types of bacterial toxins that can cause infectious toxic shock. Antibiotics are used for treatment.
Leptotrix and streptococci in smear
They are a biofilm complex that includes leptospira and streptococci. Both representatives are gram-negative microorganisms (they do not stain purple using the Gram method in laboratory diagnostics). They form a biofilm, which acts as an additional virulence factor. It provides reliable protection for microorganisms and the matrix that it contains from the effects of the external environment for the cell, other harmful factors such as antibiotics and antibacterial drugs. Biofilm makes antibiotics less effective or completely ineffective because they are either destroyed in the biofilm or are unable to penetrate it. The microorganism complex is also capable of synthesizing various substances that increase the resistance of microorganisms. They cause various inflammations of the skin. They cause intoxication.
Consequences and complications
As a result of the development of a bacterial infection, including streptococcal, various complications arise. First of all, persistence is dangerous, in which active and dormant forms of microorganisms, or their toxins, waste products persist in the blood. In this state, they can cause the development of a new source of infection, and can also cause infection of another person (that is, a person who has had an infectious disease becomes a carrier of bacteria). Many of them cause sore throats, tonsillitis, pharyngitis, sinusitis, and even diseases of the lower respiratory tract - pneumonia, bronchitis, sometimes even pleurisy. In case of a severe disease, which is accompanied by signs of intoxication, it is necessary to do a bacteriological blood culture.
If more than 8-14% bacteremia is detected in the blood, we can talk about the likelihood of developing toxic shock, which is represented by an acute complex of symptoms, intoxication, and often ends in death.
When it gets into the blood, it can become a secondary source of infection. In 40% of cases, it causes severe blood infections, including sepsis. In 30%, secondary pneumonia occurs, which is difficult to treat and often ends in pulmonary edema or pulmonary failure. A common complication is nephritis, glomerulonephritis, and other severe kidney damage, which can end in the development of renal failure. All this can cause a violation of homeostasis, edema, a violation of the excretory function, ultimately progressing to renal failure. Also, the consequence can be hypersensitization, increased sensitivity of the body, autoimmune and allergic reactions, and other abnormal reactions of the immune system.
Viridans and epidermal staphylococci often cause inflammatory diseases of the digestive and respiratory tract, can provoke endocarditis, meningitis, sepsis. The danger for women is that microorganisms can colonize the birth canal and reproductive organs, becoming a source of infection for a sexual partner.
The greatest danger is the inability to conceive a child, infertility, and the development of severe gynecological diseases. During pregnancy, they cause miscarriages, abortions, premature births, and can also provoke intrauterine infection of the fetus, which ends in stillbirth, intrauterine death of the child. Children are often born with congenital defects, malformations, and anomalies. Death can occur from infectious toxic shock, high bacteremia, sepsis.
Treatment
The main treatment for bacterial infections is antibiotic therapy. Antibiotics are prescribed that target gram-negative microorganisms. Broad-spectrum antibiotics that are active against various types of microorganisms, including gram-positive, gram-negative, aerobic, anaerobic forms, and even some types of fungal infections, may also be suitable. Read this article for more information on how to treat streptococcus if it is detected in a smear.
Prevention
It is important to limit the sources of infection: timely sanitize the oral cavity, promptly treat infectious diseases, preventing their transition to a chronic form. If possible, it is necessary to eliminate all sources of infection, cure the chronic. Prevention is also based on timely diagnosis of existing diseases, timely adoption of measures for their treatment. It is important to identify any pathology at an early stage of its formation and take the necessary measures. This will prevent the progression of the disease.
Good prevention includes massage, proper nutrition, taking necessary vitamins, and preventive vaccinations. During epidemics, avoid crowded places, take individual preventive measures, exercise, and strengthen the body.
It is necessary to do physical exercises, eat right and follow a daily routine. To avoid the development of epidermal forms of infection, clothing should be natural, should not irritate the skin and cause excessive compression and squeezing of the skin. It is necessary to consume a sufficient amount of vitamins and liquids.
Forecast
If the streptococcus in the smear significantly exceeds the normal values, it is necessary to take measures to normalize this indicator. With proper and timely treatment, the prognosis is favorable - streptococcal infection can be successfully cured. In the absence of treatment, various complications may arise - from prolonged and severe inflammatory and infectious processes to bacteremia and sepsis.


 [
[