Medical expert of the article
New publications
Inflammation of the cervix (cervicitis)
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
One of the most common diseases of the female genital organs is inflammation of the cervix or cervicitis (from the Latin cervix uteri - cervix). This pathology is classified as class XIV (diseases of the genitourinary system) and has a code according to ICD 10 - N72, inflammatory disease of the cervix. To identify the infection that caused this disease, a code for bacterial, viral and other infectious agents (B95-B97) is added.
An increasing number of women of childbearing age are faced with this diagnosis, and inflammation of the cervix, moving to the uterus and appendages, can cause irreversible consequences.
Causes cervical inflammation
First of all, the causes of inflammation of the cervix are associated with the activation of such persistent opportunistic bacteria as Staphylococcus spp. and Streptococcus spp. Microorganisms go on the attack when the system of innate and adaptive cellular immunity of the mucous tissues of the cervix fails. The local immune system - due to the presence of T-lymphocytes and immunologically active cells secreting immunoglobulins IgA, IgG, IgM in the epithelium of the cervical canal, is the "first line of defense" against foreign antigens.
At the same time, as it turned out, the expression of the secretory component of the mucous membrane of the cervical canal is regulated and controlled by sex hormones - 17β-estradiol and progesterone - and changes with their release from the ovaries during the menstrual cycle. So fluctuations in hormone synthesis create certain conditions under which inflammation of the cervix can develop during pregnancy or in the period preceding menopause.
This also concerns resistance to sexually transmitted infections. In many cases, the pathogenesis of inflammatory processes of the mucous membrane of the cervical canal (endocervicitis) is hidden in the defeat of chlamydia (Chlamydia trachomatis), gonococci (Neisseria gonorrhoeae), mycoplasma (Mycoplasma genitalium).
The recognized causes of inflammation of the cervix in the area of the exocervix of its vaginal part in gynecology - affecting the flat and columnar epithelium of exocervicitis - include Trichomonas vaginalis, the genital herpes virus Herpes simplex type II, human papillomavirus (HPV), fungal infection Candida, actinobacteria Gardnerella vaginalis, and Treponema pallidum (the causative agent of syphilis).
Inflammation of the cervix can result from trauma and subsequent infection, as often happens when inflammation of the cervix is diagnosed after childbirth or after a surgical abortion.
Gynecologists note the negative role of contraception with the help of IUDs and chemical contraceptives (spermicides) in the development of cervicitis. Constant vaginal douching leads to disruption of the vaginal microbiocenosis, against the background of which inflammation of the vagina and cervix very often occurs, since the same bacteria and viruses are involved in infection with colpitis (vaginitis) as with cervicitis.
Symptoms cervical inflammation
With a mild form of inflammation of the cervix, many women do not even notice the signs of pathology. However, the first signs of inflammation can appear immediately after the end of the next menstruation.
The key symptoms of cervical inflammation are expressed as:
- pain in the lower abdomen during coitus and painful postcoital sensations in the vagina;
- vaginal pruritis (itching);
- genital irritation;
- mucous-bloody vaginal discharge of varying intensity;
- bleeding between periods;
- burning during urination and increased frequency of urination (since the inflammatory process can lead to urethritis).
According to experts, the temperature during inflammation of the cervix remains normal. But complications of cervicitis, when the inflammation spreads to the uterus, fallopian tubes or ovaries, causing inflammatory diseases of the pelvic organs, give not only increased pain in the lower abdominal cavity, but also subfebrile body temperature.
In almost two thirds of cases of latent cervicitis, chronic inflammation of the cervix inevitably develops - asymptomatic or having similar signs. A complication of such inflammation is often erosion of the cervix.
The type of infectious agent determines the type of discharge during inflammation of the cervix: when affected by chlamydia, it is mucous with an admixture of pus; with trichomonas etiology of inflammation, it is yellow or slightly greenish with foam and an unpleasant odor; a fungal infection produces a cheesy discharge. And purulent inflammation of the cervix with greenish vaginal discharge is most often observed with gonococcal infection.
Chronic inflammation of the cervix during pregnancy has particularly dangerous negative consequences. This includes termination of pregnancy, premature birth, antenatal infection of the fetus, and septic complications in women in labor. And chronic inflammation of the cervix, caused by papillomavirus infection, threatens oncology.
Where does it hurt?
Diagnostics cervical inflammation
Diagnosis of cervical inflammation begins with a gynecological examination of the cervix and assessment of its condition.
Laboratory tests require blood tests - general and biochemical, as well as enzyme immunoassay for the presence of antibodies to Chlamydia trachomatis and the herpes virus.
Also, a scraping from the mucous membrane of the cervix and a smear from the cervical canal for bacterial microflora (including DNA of trichomonads and gonococci) are required; a Pap smear (Pap test) for the presence of the human papillomavirus (HPV).
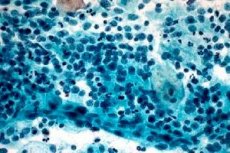
The result of these morphological studies of the biomaterial from the site of the pathological process is a cytogram of cervical inflammation - a detailed description of the state of the cells of the endo- and exocervix indicating all detected infectious agents and pathological changes at the cellular level. In clinical gynecology, this diagnostic method, based on bacterioscopy, is considered the most informative and accurate.
Instrumental diagnostics are performed using colposcopy, which allows for multiple magnification to visualize structural changes in the mucous membranes of the cervix and vagina affected by infection. In the case of chronic inflammation of the cervical canal mucosa and a positive Pap smear, a biopsy is performed during colposcopy.
How to examine?
What tests are needed?
Differential diagnosis
Differential diagnostics is extremely important in cervicitis, since only the correct determination of the causative agent of inflammation can give a positive result of the disease treatment. Cervicitis is also differentiated from cervical cancer and other benign processes in this area.
Who to contact?
Treatment cervical inflammation
The prescribed treatment for cervical inflammation necessarily takes into account the type of infection. The main drugs in cases of staphylococcal and streptococcal inflammation, inflammation due to infection with gonococci, chlamydia or trichomonas are antibacterial.
An antibiotic for inflammation of the cervix is prescribed taking into account the susceptibility of a specific microorganism to drugs of this pharmacological group. Thus, for gonorrheal, staphylococcal and streptococcal cervicitis, the beta-lactam antibiotic Ceftriaxone is effective, which is administered intramuscularly (0.5-1 ml once a day).
As noted in the instructions, its side effects may include nausea, diarrhea, allergic skin reactions, candidiasis and deterioration of kidney function. Intestinal microflora is also affected. The drug is not used in the first trimester of pregnancy.
The main antibiotics for chlamydial inflammation of the cervix are Azithromycin, Doxycycline and Ofloxacin, which are taken orally. For example, Ofloxacin is recommended to be taken one tablet (0.2 g) twice a day for 7-10 days. In addition to the side effects typical of most antibiotics, the use of this drug in the treatment of inflammation of the cervix can cause increased sensitivity to UV radiation.
Treatment of inflammation of the cervix caused by trichomonas requires the use of Metronidazole (Trichopolum, Efloran, Novonidazole and other synonyms) in tablets of 0.25 g. The drug is prescribed one tablet twice a day (during meals), the duration of administration is from 5 to 8 days. In addition, it is necessary to simultaneously use Metronidazole vaginal suppositories for 10 days (two suppositories per day). Side effects of this drug include nausea, vomiting, dryness and a metallic taste in the mouth, problems with the intestines and urination, dizziness, weakness, sleep disorders, etc. And contraindications include pregnancy, epilepsy, kidney or liver failure.
For inflammation caused by the herpes virus, a 5-day course of treatment with Acyclovir tablets (Zovirax, Geviran, Valtrex) is prescribed: one tablet (200 mg) every 4 hours during the day (with a glass of water). Taking this drug can cause hives, swelling, nausea, vomiting, increased bilirubin levels in the blood, abdominal pain, sleep disturbances, convulsions, etc.
Surgical treatment - in the form of coagulation of the affected tissue using electrocoagulation, cryotherapy or laser therapy - for this disease is carried out only if drug therapy is ineffective and areas of erosion appear on the mucous membranes of the cervix.
Local treatment of cervical inflammation
In gynecology, vaginal tablets and suppositories are widely used for inflammation of the cervix.
In addition to the already mentioned Metronidazole vaginal suppositories, doctors recommend Trichomonacid, Gainomax, Ginalgin, etc. for trichomonas inflammation. Suppositories for candidal inflammation are Ginezol, Neo-Penotran (Metromicon-neo), Zalain. For non-specific infections, a 3-5-day course of treatment with antibiotic suppositories Clindacin (Dalacin) helps.
Antiseptic vaginal suppositories Hexicon are often prescribed for inflammation of the cervix (another trade name is Chlorhexidine). One suppository should be inserted twice a day, the course of treatment can last up to three weeks. This remedy is allowed to be used by pregnant women.
Terzhinan vaginal tablets for inflammation of the cervix act in a complex manner, since they contain an antibiotic (Neomycin), an imidazole derivative Ternidazole active against trichomonads, a polyene antibiotic Nystatin (destroying yeast-like fungi), and Prednisolone, which relieves local inflammation. It is recommended to insert one tablet into the vagina once a day (preferably at night). After insertion, a slight burning sensation may be felt, and irritation may occur. The drug is not used in the first three months of pregnancy.
In case of chlamydial inflammation, the cervix is treated with a 2% solution of silver nitrate, 1% alcohol or 2% oil solution of Chlorophyllipt (based on eucalyptus leaf extract) or a solution of Malavit (from medicinal plants with the addition of mumiyo).
Also used is such a method of local therapy as douching for inflammation of the cervix. Gynecologists strongly recommend carrying out this procedure at home, observing all the rules of antisepsis and not relying on the fact that this method can replace systemic treatment of infections.
Among the douching agents, 0.01% antiseptic solution Miramistin is noted for inflammation of the cervix caused by streptococci and staphylococci, gonococci, chlamydia and trichomonas. A tampon soaked in this solution should also be inserted into the vagina every day.
Folk remedies
In the presence of such serious pathogens of the inflammatory process in the cervical tissues, the decision to use folk remedies should be discussed with your doctor, who is unlikely to approve of this idea.
However, herbal treatment for cervical inflammation is still practiced. It mainly includes vaginal douching with decoctions of medicinal plants.
Some “folk recipes” posted on the Internet have no relation to this pathology in their composition.
The most correct medicinal herbal collection recommended by professional herbalists is as follows. You need to take: calendula flowers, chamomile flowers and St. John's wort (5 tablespoons of dry raw materials of each plant), as well as half as much licorice root, plantain leaves and knotweed (snakeweed) grass. Mix all the herbs, and to prepare the decoction, take a heaping tablespoon of this mixture per 250 ml of water. The grass is poured with boiling water, infused in a closed container for about 40 minutes, then brought to a boil and cooked for 5 minutes.
After the decoction has cooled to +37°C, it must be strained and used as directed – once a day (no more than 10 days in a row).
More information of the treatment
Prevention
Prevention in the form of "latex-protected" sex should protect against STDs and prevent any other infectious agent from getting in. However, opportunistic microflora is present in the vagina, and there may also be dormant herpesvirus or HPV... And only a strong immune system prevents them from manifesting themselves. Therefore, all doctors advocate strengthening the immune system or, at least, advise making efforts so that the body's defenses do not weaken due to unhealthy habits, lack of adequate nutrition and vitamins.
Forecast
According to gynecologists, every woman should undergo regular check-ups (once every six months). This will help to detect inflammation in time and cure it faster.
Moreover, if cervical inflammation is not treated, the prognosis is very disappointing: the inflammation can spread higher and affect the uterine mucosa, fallopian tubes and ovaries, which can cause fertility problems.


 [
[