Medical expert of the article
New publications
Malignant melanoma of the skin
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
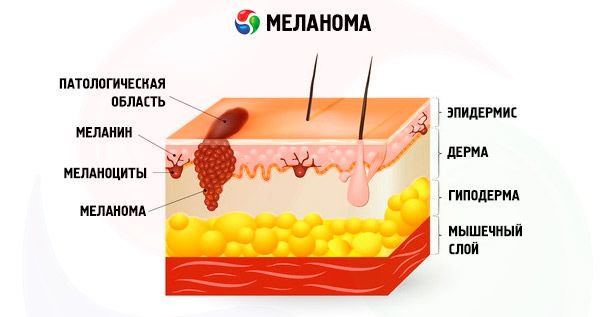
Malignant melanoma of the skin (syn.: melanoblastoma, melanocarcinoma, melanosarcoma) is a highly malignant tumor consisting of atypical melanocytes.
A genetic predisposition to the development of melanoma has been noted - at least 10% of all cases of melanoma are familial.
Causes skin melanomas
The genetic defect is currently unknown, but many patients in such families have been found to have deletions of the 9p21 region. The risk of developing melanoma is increased in people with multiple (more than 50) common melanocytic nevi; with congenital nevi, especially giant ones; with multiple dysplastic nevi. One of the most important provoking factors is the negative effect of solar radiation on the skin. Great importance is attached to the total dose of solar radiation received in the first 5 years of life and the presence of a history of sunburn in childhood. The relative risk of developing melanoma is associated with skin phototype. The risk group mainly includes white-skinned people with blond or red hair, blue eyes and numerous freckles, who tan poorly and easily get sunburned.
Malignant melanoma of the skin mainly develops in adults, but cases of congenital melanoma and its occurrence in childhood have been described; it can occur on any area of the skin, including the nail bed.
Symptoms skin melanomas
The tumor is asymmetrical, initially flat, slightly raised, less often dome-shaped, heavily and unevenly pigmented. with the exception of amelanotic forms. Sometimes it reaches very large sizes, the surface becomes uneven as it grows, becomes covered with crusts, is easily injured, bleeds. Pigmentation increases, the color becomes almost black with a bluish tint. With spontaneous focal regression of the tumor, areas of depigmentation are revealed. Ulceration and disintegration of the tumor may occur. Small, pigmented daughter elements appear around it.
The most common type is superficial spreading melanoma, which is characterized by fairly long-standing spots or plaques of brown color with pinkish-gray and black inclusions, localized most often on the skin of the back, especially in men, and in women - mainly on the lower extremities. An amorphous variant is possible.
Lentigo melanoma is usually localized on the face, neck, back of the extremities, develops in old age against the background of long-standing malignant lentigo (precancerous melanosis of Dubreuil). With the onset of invasive growth, elevated areas or individual nodules appear within the unevenly pigmented spot. An apigmented variant is possible. Lentiginous melanoma of acral localization and melanoma of the mucous membranes have a similar histological picture and differ in characteristic localization - on the mucous membranes, on the skin of the palms, soles, in the area of the nail bed.
Nodular melanoma protrudes above the skin surface as an exophytic, often symmetrical, dark brown or black formation or as a polyp on a stalk. The surface is initially smooth, shiny, and may be warty. The tumor quickly increases in size and often ulcerates. It is localized mainly on the back, head, neck, but may also be in other areas. An apigmented variant is possible. When nodular melanoma is detected, the possibility of metastasis from another primary site should be kept in mind.
Desmoplastic neurotropic melanoma occurs mainly in the head and neck area, usually has the appearance of a non-pigmented, compacted plaque at the base or a dense tumor-like formation, sometimes against the background of malignant lentigo. It is characterized by a high risk of recurrence.
Malignant blue nevus is a malignant cellular blue nevus and is characterized by an aggressive course, although cases with late metastasis have been described. Sometimes it occurs against the background of Oga nevus. It is observed mainly in middle-aged and elderly people, mainly on the skin of the face and scalp, chest, buttocks.
Where does it hurt?
Stages
According to histological studies, no more than 35% of melanomas develop in the area of melanocytic nevi. The rest develop de novo on unchanged skin.
The clinical and morphological classification of melanoma is based on the definition of the horizontal and vertical growth phases proposed by WH Clark et al. (1986). In the horizontal growth phase, lateral spread of a flat pigmented area is determined due to intraepidermal proliferation of atypical melanocytes. The intraepidermal component of the tumor (to a greater extent its architectonics and growth pattern, to a lesser extent - cytological features) is different in superficially spreading, lentigo melanoma and lentiginous melanoma of acral localization. The horizontal growth phase precedes the vertical one, with the exception of nodular melanoma and some other rare types of melanoma.
As the tumor progresses, the basal membrane of the epidermis is destroyed and the invasive stage begins. However, the invasion of the papillary layer of the dermis by single melanocytes or groups of cells does not mean that the tumor has entered the vertical growth phase, i.e. has acquired the ability to metastasize. The vertical tumor growth phase reflects tumor progression and is not synonymous with the anatomical level of invasion. It assumes the presence of a volumetric formation in the dermis (tumorigenic phase) and usually corresponds to at least level III of melanoma invasion according to Clark:
- Level I - melanoma cells are found only in the epidermis (melanoma in situ);
- Level II - melanoma cells are located in the papillary layer of the dermis, but do not fill it completely and do not stretch it with their mass;
- Level III - a tumor node is determined that completely fills the papillary layer of the dermis up to its border with the reticular layer, increasing its volume;
- Level IV – melanoma cells infiltrating the reticular layer of the dermis are identified;
- Level V - subcutaneous tissue invasion.
DE Elder and GF Murphy (1994) subdivide all forms of malignant melanoma of the skin based on clinical and morphological features into those with a horizontal growth phase (superficial spreading melanoma; lentigo melanoma; lentiginous melanoma of the acral localization and mucous membranes; unclassified types) and those without it (nodular melanoma; desmoplastic and neurotropic melanoma; melanoma with a minimal degree of malignancy; malignant blue nevus; unclassified vertical growth phase).
 [ 13 ]
[ 13 ]
Forms
Superficially spreading melanoma is characterized by the proliferation of a large number of individual melanocytes or their "nests" throughout the entire thickness of the epidermis. Melanocytes with light abundant cytoplasm containing finely dispersed (dust-like) melanin and dark, atypical nuclei resemble Paget cells. Later, the epithelium of the skin appendages may be involved. The invasive component is characterized by the presence of fairly large polymorphic cells of cubic or polygonal shape, resembling epithelial cells, sometimes elongated, spindle-shaped. There are also balloon-shaped, signet-ring-shaped, nevus-shaped cells - small, round or oval, with hyperchromic nuclei, a narrow rim of cytoplasm in which the pigment is not visible. In all cases, pronounced polymorphism of cellular elements is noted, mitoses are characteristic, including pathological ones.
In lentigo melanoma, the intraepidermal component is characterized by lentiginous proliferation of atypical melanocytes of polygonal outlines, often with very large nuclei, usually located within the basal layer, sometimes in the form of "nests". Migration into the overlying layers of the epidermis is weakly expressed; melanocytes resembling Paget's cells are practically not encountered. Early damage to the epithelium of the superficial areas of the skin appendages, especially hair follicles, is characteristic. Atrophy of the epidermis is often observed in this form. The invasive component is often represented by spindle-shaped cells; giant multinucleated cells are encountered. Solar elastosis is usually expressed in the upper areas of the surrounding dermis.
Nodular melanoma is a special form of melanoma, which is spoken of when only a vertical growth phase is detected in a histological specimen with intact epidermis and papillary dermis. It is assumed that nodular melanoma thus arises in the dermis de novo, and at present there is no data for the pre-existence of a rapid horizontal phase with subsequent regression of the intraepidermal component, although such a theory is considered by some authors. Most often, the tumor is formed by round or polygonal epithelioid cells. It is necessary to differentiate from metastatic melanoma.
Acral lentiginous melanoma is characterized by lentiginous proliferation of atypical melanocytes. Migration into the overlying layers of the epidermis is poorly expressed, melanocytes resembling Paget's cells are practically not found.
The epidermis is characterized by pronounced acanthosis, which has a characteristic sparsely looped structure. The invasion depth is significant with seemingly minor damage to the epidermis.
Desmoplastic melanoma is usually non-pigmented and consists of bundles of elongated cells resembling fibroblasts, separated by layers of connective tissue. Pleomorphism of cellular elements is usually weakly expressed, mitoses are few. Areas with pronounced differentiation towards Schwann cells and indistinguishable from schwannoma are determined. Focal accumulations of lymphocytes and plasma cells are noted, neurotropism is possible. The tumor is characterized by a significant depth of invasion.
Malignant blue nevus is characterized by the presence in the neoplasm, which has the structure of a cellular blue nevus, of a poorly delimited area of increased cellularity with signs of malignancy, such as pronounced polymorphism of nuclei, atypical mitoses, foci of necrosis and deep infiltrative growth. Unlike other forms of melanoma, within the tumor there are pigmented, elongated cells with long processes and there is no border activity of melanocytes. To confirm the diagnosis, an immunohistochemical reaction with antiserum to the PCNA antigen, a marker of proliferative activity, is sometimes used.
In addition to the listed features of various forms of melanoma, the large size of the tumor, the presence of multiple, including atypical, mitoses, the presence of areas of spontaneous necrosis with ulceration, and pronounced atypism and polymorphism of cellular elements indicate a malignant process.
Melanoma is more characterized by invasion of the stroma by layers and nests of cells, which seem to move towards the surrounding tissues, squeezing and destroying adjacent structures of the dermis during their growth.
The so-called minimal deviation melanoma, a rare histological type of melanoma with a more favorable clinical course and prognosis (minimal deviation melanoma), presents considerable difficulties for differential diagnosis. This group includes melanomas resembling Spitz nevus, small-cell nevoid melanomas, and some halo nevi.
Melanoma with minimal signs of malignancy is characterized by the presence in the dermis of a tumor formed by a more or less monomorphic population of melanocytes with mild atypism and low mitotic activity. The cells can be either epithelioid or spindle-shaped. Lentiginous proliferation of atypical melanocytes is sometimes observed in the epidermis, but the horizontal growth phase is absent.
In cases of amelanotic melanoma, the melanocytic nature of the tumor can be identified by melanin staining using the Masso-Fontan method, identification of premelanosomes in cells using electron microscopy, staining for S-100, MMB-45 and NKI/C-3 antigens using immunomorphological methods. Desmoplastic neurotropic melanoma is characterized by a negative reaction to the detection of the HMB-45 antigen.
The results of immunomorphological studies with markers of p53, PCNA, Ki-67 (MIB-1) antigens in relation to melanocytic skin tumors are not the same in different conditions, in general, poorly reproducible and inconsistent.
What do need to examine?
How to examine?
What tests are needed?
Who to contact?
More information of the treatment
Drugs
Forecast
The prognosis of skin melanoma is based on the level of invasion of the skin layers, the thickness of the invasion in millimeters according to Breslow, the mitotic index, as well as the features of the histological structure and the degree of mononuclear infiltration of tumor elements.

