Medical expert of the article
New publications
Lipomatosis of the pancreas
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
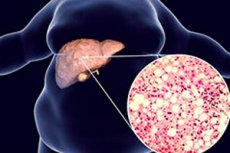
Fatty infiltration, steatosis or lipomatosis of the pancreas is an accumulation of fat (lipids) in its parenchyma.
Diffuse pancreatic changes of the lipomatosis type -- with gradual replacement of parenchymatous tissue by fatty tissue -- are also called fatty dystrophy or nonalcoholic fatty pancreatic disease. Most cases remain asymptomatic, and only some rare extreme degrees of lipomatosis or fat replacement may lead to exocrine pancreatic insufficiency.
The pancreas is both an endocrine and exocrine gland. The exocrine component makes up about 80 percent of the total gland and is mainly composed of two different cell types: acinar cells (mainly secreting digestive enzymes) and ductal cells (mainly secreting fluids and electrolytes). The endocrine component includes the typical islets of Langerhans, which contain several cell types scattered throughout the exocrine tissue. [1]
Lipomatosis and fatty replacement of the pancreas are the most common benign pathologic conditions of the adult pancreas. [2], [3] Classically, the phenomenon causes increasing hypodensity of the pancreas on CT and typical hyperechogenicity on ultrasound (USG) examination.
The accumulation of fat in the pancreas (lipomatosis) and the replacement of different areas of the pancreas with fat (fat replacement) have received various synonyms: pancreatic lipomatosis, fat replacement, fatty infiltration, fatty pancreas, lipomatous pseudohypertrophy, non-alcoholic fatty fiber. Pancreatic disease and pancreatic steatosis. These synonyms are a source of confusion.
Based on various imaging findings, one might be inclined to use the term "lipomatous infiltration" when the glandular islets of the pancreas appear dissociated by adipose tissue or when the density (CT), echogenicity (ultrasound), or signal (MRI) is diffusely modified. When pancreatic islets appear to have disappeared or have been extensively replaced by fat, so-called "fat replacement" may be more likely to be favored.
Similarly, one may be inclined to use the term "lipomatous infiltration" when the process appears reversible, and to reserve the term "fat replacement" for cases demonstrating probable irreversible disappearance of glandular islets. [4]
Epidemiology
Due to the lack of standardized diagnostic parameters, the epidemiology of pancreatic lipomatosis is not clearly defined. According to the results of some studies, this condition is often detected incidentally with a prevalence of up to 35%.
In the presence of general obesity, fatty pancreatic disease is diagnosed in almost 70% of cases. And in obese children, pancreatic lipomatosis is noted in 20% of cases of referral to a doctor.
Causes of the pancreatic lipomatosis.
Pancreatic lipomatosis is a benign disease with no single etiology. [5], [6] The condition is associated with many diseases and conditions. Age and obesity correlate significantly with the degree of fatty infiltration of the pancreas. (GIPJ) [7] As a consequence, fatty infiltration usually correlates directly with the patient's body mass index (BMI). More precisely, there is a better correlation between GIIPF and visceral fat index, which, however, is more difficult to assess than the patient's BMI or weight. In other words, the amount of visceral adipose tissue is a better indicator and predictor of pancreatic GIJI than BMI itself.
Leading causes of pancreatic lipomatosis include:
- Disorder fat metabolism;
- Abdominal type of obesity with accumulation of visceral fat;
- Metabolic Syndrome (affecting the breakdown of pancreatic adipocytes - fat cells); [8]
- Excessive levels of lipids (lipoproteins) in the blood - dyslipidemia or hyperlipidemia;
- Hypercholesterolemia;
- Diabetes; [9]
- Chronic pancreatitis with atrophy of acinar cells;
- Isolated pancreatic islet amyloidosis;
- Pancreatic duct stenosis (congenital, as well as due to the presence of intraductal concretions or tumor); [10]
- Congenital syndromes, such as those associated with a mutation in the carboxyester lipase enzyme gene mODY-diabetes type 8.
- Large fatty infiltration of the pancreas is also the most frequent CT scan picture in adolescents and adults with cystic fibrosis. [11], [12], [13]
And pancreatic lipomatosis in a child may be associated with malnutrition and severe dystrophy (kwashiorkor), with a genetically determined disorder of fat metabolism (Wolman disease), schwachman-Daimond syndrome, Johansson-Blizzard syndrome, hypercorticism in children (Cushing's syndrome), hypothalamic syndrome adolescents during puberty.
Risk factors
Risk factors for fat accumulation in the pancreas include:
- Older age (aging + hormonal changes);
- High-fat diet;
- Obesity with a BMI (body mass index) ≥ 30;
- Insulin resistance;
- Chronic alcohol abuse;
- Hypertension or hyperlipidemia;
- Chronic hepatitis B;
- Reovirus infection and HIV;
- Exposure to toxins.
Pathogenesis
The mechanism of development of fatty infiltration of the pancreas has not been fully investigated. According to experts, the main links in the pathogenesis of this condition are dysfunction of adipose tissue in obesity and redistribution of fat with infiltration of parenchyma with triglycerides, which initially causes hypertrophy and hyperplasia of gland cells.
The main manifestation of adipose tissue dysfunction is increased differentiation of fat cell precursors (preadipocytes) into mature adipocytes, and in the pancreas, lipids are mainly stored in adipocytes. But ectopic fat deposits can also form as fat droplets in the acinar cells (secreting digestive enzymes) of the pancreas, causing them to die with replacement by fat cells, and this is essentially partial atrophy and lipomatosis of the pancreas.
In addition, fat can potentially enter the gland (including the insulin-producing β-cells of the islets of Langerhans) from free fatty acids circulating in the blood, dietary fat intake, and in the process of lipogenesis - the conversion of glycerol and fatty acids into fat.
As studies have shown, an important role in pancreatic steatosis is played not only by excessive fat consumption, but also by elevated blood glucose levels (hyperglycemia). Hyperglycemia slows down the degradation of fatty acids - their mitochondrial oxidation, which causes the accumulation of triglycerides in cells.
Also read - diffuse changes in the pancreas
Symptoms of the pancreatic lipomatosis.
In most cases, the initial lipomatosis of the pancreas - lipomatosis of the 1st degree (with lesions up to 25-30% of the gland) - is asymptomatic, and the first signs of pathology appear when diffuse lipomatosis of the pancreatic parenchyma covers more significant areas of the organ.
Thus, lipomatosis of the pancreas of the 2nd degree is determined when up to 60% of its parenchyma is affected, and then symptoms of pancreatogenic dyspepsia may appear - with discomfort and heaviness in the epigastric region after eating, chronic diarrhea, the presence of fat in the feces (steatorrhea) and weight loss.
When more than 60% of the parenchyma is affected - grade 3 pancreatic lipomatosis - there is marked pancreatic lipomatosis, in which patients experience decreased appetite, increased intestinal gas production and abdominal bloating, nausea and vomiting, may experience pain in the upper abdomen, fever, and increased heart rate. [14]
Liver and pancreatic lipomatosis are often combined: in approximately 50-80% of patients, pancreatic lipomatosis and fatty hepatosis of the liver, i.e. liver steatosis (or fatty dystrophy of the liver) develop almost simultaneously.
There may also be liver enlargement - hepatomegaly and pancreatic lipomatosis. [15]
Only a few case reports indicate a direct link between pancreatic fatty infiltration and exocrine pancreatic insufficiency, and adequate demonstration of this relationship has yet to be established. Further functional studies are needed to establish the exact degree of FI capable of causing symptomatic extrinsic secretory insufficiency.
Complications and consequences
Fatty pancreatic disease can give complications and have negative health consequences.
Answering the question, what is the danger of pancreatic lipomatosis, gastroenterologists and endocrinologists note: pancreatic steatosis not only causes the development of digestive insufficiency syndrome, but also affects insulin secretion. The presence of fatty infiltration of the pancreas >25% increases the likelihood of developing type 2 diabetes and generalized atherosclerosis.
Extensive fatty infiltration of the pancreas can lead to hepatic steatosis the development of nonalcoholic steatohepatitis. [16], [17]
Exocrine dysfunction of the gland can induce the development of chronic pancreatitis. In addition, according to oncologists, patients with pancreatic lipomatosis have an increased risk of malignant tumor formation - pancreatic carcinoma. [18]
Diagnostics of the pancreatic lipomatosis.
The basis for diagnosing this condition is instrumental diagnostics: abdominal ultrasound, transabdominal ultrasound of the pancreas, computer and/or magnetic resonance imaging. Lipomatosis of the pancreas on ultrasound is recognized by diffuse hyperechogenicity of the parenchyma.
The reason for the higher sensitivity of ultrasound to detect irregular cephalic fatty infiltration is thought to be related to the generally higher sensitivity of ultrasound to detect subtle differences in fat in different tissues. This is also a common observation in the liver, in which ultrasound more easily detects a hyperechogenic area of limited steatosis and a hypoechogenic area of steatosis-prone tissue than CT. [19]
During ultrasound, pancreatic lipomatosis appears hyperechogenic rather than hypoechogenic, as is usually seen with lipoma. The reason is that the echogenicity is not determined by the fat itself, but by architectural changes caused by the development of adipocytes within the interdollicular septa. It is the alternation of glandular and fatty boundaries that is responsible for the hyperechogenicity. [20]
On the contrary, the more the pancreas is infiltrated or replaced by fat, the easier it is for CT to diagnose the mass. Thus, CT becomes the method of choice for massive fatty infiltration of the pancreas. [21]
Patients also undergo blood tests (general, for pancreatic enzymes, total cholesterol and glucose levels), urinalysis for pancreatic enzymes, and coprogram.
Differential diagnosis
Differential diagnosis includes pancreatic neoplasms, atrophic gastritis, chronic enteritis and enterocolitis, malabsorption syndrome.
Lipomatous pseudohypertrophy of the pancreas
Lipomatous pseudohypertrophy (LHP) of the pancreas is a special situation of pancreatic lipomatosis that has probably controversially been regarded as a rare, specific, and independent entity. This situation of disproportionate replacement of the entire pancreas by increasing amounts of adipose tissue and subsequent enlargement of the entire gland was first described by Hantelmann in 1931; the disease was later named lipomatous pseudohypertrophy.
The disease is considered very rare and the specific etiology remains unknown. [22] An association with rare pediatric syndromes such as Schwachman-Daimon, Bannayan or Johansson-Blizzard syndrome has been reported. Various possible causes have been postulated, ranging from a congenital anomaly to an acquired condition caused by damage by infectious or toxic agents or by chronic obstruction of the pancreatic ducts causing atrophy and subsequent fat replacement. [23] This latter hypothesis suffers from the fact that the amount of fat is indeed disproportionate and from the demonstration of normal pancreatic ducts in several articles. [24] Moreover, the residual islets of pancreatic tissue appear to be quite preserved or at least intact. An association with chronic hepatitis B and other chronic, neglected liver lesions has also been reported. This situation has been diagnosed in young patients and in other patients without obesity, diabetes mellitus, or pancreatitis. These characteristics probably emphasize the benign course of this particular disease, which, however, may be associated with significant exocrine pancreatic dysfunction.
Treatment of the pancreatic lipomatosis.
Treatment of pancreatic lipomatosis depends on its origin, but there is no specific treatment of this pathology to date. At the same time, recommendations for the treatment of liver steatosis are used: reduction of body weight, exercise, dietary restrictions. [25] So, a diet table 5 is prescribed for lipomatosis of the pancreas; about this diet and its menu in detail in publications:
By correcting the external secretory insufficiency of the pancreas is carried out treatment of digestive failure syndrome, using such drugs of the group of enzyme drugs as Pancreatin, Panzinorm, Creon, mezim, Penzital, digestal and others.
Statins (Simvastatin, etc.) are used to treat dyslipidemia and hypercholesterolemia. The hypolipidemic drug Ezetimibe (Ezetrop, Lipobon) has shown encouraging results in reducing total pancreatic fat and triglyceride levels.
To date, surgical treatment may consist of bariatric surgery - performing laparoscopic sleeve gastrectomy (gastroplasty). Foreign clinical experience shows that after such surgery, most patients experience a reduction in body weight, improvement in lipid profile, reduction in the total volume of the pancreas and its fat content.
Prevention
Making healthy changes in lifestyle and eating habits, as well as regular exercise, can help prevent fatty infiltration of the pancreas.
Forecast
Regarding the quality of life - if lipomatosis of the pancreas is not treated - the prognosis is poor: the patient will continue to lose weight, have digestive problems, and suffer from bouts of malaise. But the life expectancy, in the absence of complications (for example, chronic pancreatitis or pancreatic carcinoma) this disease has little effect.
List of authoritative books and studies related to the study of pancreatic lipomatosis
- "Pancreatic Lipomatosis: An Unusual Cause of Acute Pancreatitis" is an article authored by K. Khan et al, published in Case Reports in Gastrointestinal Medicine in 2016.
- "Pancreatic Lipomatosis: A Comprehensive Review with Illustrative Examples of CT and MR Findings" - article authored by R. N. Oliveira et al, published in the Polish Journal of Radiology in 2017.
- "Lipomatosis of the Pancreas: An Unusual Cause of Acute Pancreatitis" is an article authored by S. Patil et al, published in The Indian Journal of Radiology & Imaging in 2014.
- "Fatty Infiltration of the Pancreas: Evaluation with Multidetector Computed Tomography" is an article authored by L. Bertin et al, published in Diagnostic and Interventional Imaging in 2015.
- "Pancreatic Lipomatosis: An Indicator of Pancreatic Atrophy?". - article authored by A. S. Mazo et al, published in the journal Abdominal Radiology in 2018.
Literature
Saveliev, V. S. Clinical Surgery. In 3 vol. Vol. 1: national manual / Ed. By V. S. Saveliev. С. Savelyev, A. I. Kirienko. - Moscow: GEOTAR-Media, 2008.

