Medical expert of the article
New publications
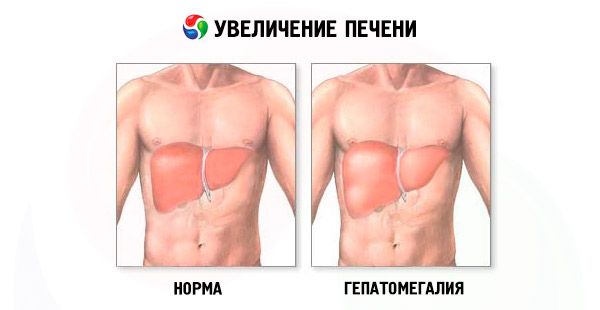
Liver enlargement
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Liver enlargement - hepatomegaly - is observed in cases where the size of this vital organ exceeds natural, anatomically determined parameters. As doctors emphasize, this pathology cannot be considered a separate liver disease, since it is a symptom characteristic of many diseases, including those affecting other organs and systems of the human body.
The danger of an enlarged liver lies in the complications of liver failure and other pathological conditions that disrupt the normal functioning of this organ and create many serious health problems.
Therefore, it is worth discussing such a common pathology as liver enlargement in more detail.
Causes of liver enlargement
Perhaps the list below, including the causes of liver enlargement, is incomplete, but it should make you realize the true scale of its pathogenesis and get an answer to the question - is liver enlargement dangerous?
So, an enlarged liver in an adult can be a consequence of:
- excessive alcohol consumption;
- cirrhosis of the liver;
- taking large doses of certain medications, vitamin complexes and dietary supplements;
- infectious diseases (malaria, tularemia, etc.);
- lesions caused by hepatitis viruses A, B, C;
- infectious lesions caused by enteroviruses, pathogens of intestinal infections, leptospirosis, Epstein-Barr virus (mononucleosis);
- toxic damage to the parenchyma by industrial or plant poisons;
- fatty hepatosis (fatty degeneration or steatosis of the liver);
- disorders of copper metabolism in the liver (hepatolenticular degeneration or Wilson's disease);
- disorders of iron metabolism in the liver (hemochromatosis);
- inflammation of the intrahepatic bile ducts (cholangitis);
- genetically determined systemic diseases (amyloidosis, hyperlipoproteinemia, glucosylceramide lipidosis, generalized glycogenosis, etc.);
- obliterating endarteritis of the liver veins;
- liver cancer (hepatocarcinoma, epithelioma or metastatic cancer);
- leukemia;
- diffuse non-Hodgkin's lymphoma;
- formation of multiple cysts (polycystic disease).
As a rule, an increase in the liver lobe is observed, and an increase in the right lobe of the liver (which has a higher functional load in the work of the organ) is diagnosed more often than an increase in the left lobe of the liver. However, this is also not good, since the left lobe is so close to the pancreas that it is possible that this gland is creating the problem.
Simultaneous enlargement of the liver and pancreas is possible with inflammation of the pancreas (pancreatitis). Inflammation is accompanied by intoxication, and the liver is responsible for removing toxins from the blood. If pancreatitis takes particularly severe forms, the liver may not cope with its task and increases in size.
Diffuse enlargement of the liver is a clearly non-localized change in the size of its lobules, consisting of hepatocytes (liver cells). For one of the above reasons, hepatocytes begin to die, and glandular tissue gives way to fibrous tissue. The latter continues to grow, thereby enlarging (and deforming) individual areas of the organ, squeezing the hepatic veins and creating the prerequisites for inflammation and edema of the parenchyma.
Symptoms of an Enlarged Liver
A person may not feel a minor pathology - an increase in the liver by 1 cm or an increase in the liver by 2 cm. But the process of changing the natural size of the liver sooner or later begins to manifest itself in more obvious clinical symptoms.
The most typical symptoms of liver enlargement are: weakness and rapid fatigue, which patients feel even without intense exercise; unpleasant sensations (heaviness and discomfort) in the abdominal cavity; bouts of nausea; weight loss. Heartburn, halitosis (constant bad breath), itchy skin and dyspepsia may also occur.
Enlargement of the liver with hepatitis is accompanied not only by general malaise, but also by yellowing of the skin and sclera, fever, aches in all joints, and a nagging pain in the right hypochondrium.
Liver enlargement in cirrhosis occurs against the background of the same complex of symptoms, to which are added such signs of this disease: abdominal pain and its enlargement, a quickly occurring feeling of satiety when eating, increased sleepiness during the day and insomnia at night, nosebleeds and bleeding gums, weight loss, hair loss, decreased ability to remember information. In addition to liver enlargement in cirrhosis (first both lobes, and then to a greater extent the left), the size of the spleen in half of patients also increases, and doctors determine hepatosplenomegaly - an enlargement of the liver and spleen.
In the clinical manifestation of the defeat of the body by the human immunodeficiency virus, liver enlargement in HIV is diagnosed at stage 2B - in acute HIV infection without secondary diseases. In addition to liver and spleen enlargement at this stage, fever, skin rash and rashes on the mucous membranes of the mouth and pharynx, enlarged lymph nodes, and dyspepsia are noted.
Fatty hepatosis with liver enlargement
According to the latest WHO data, 25% of adult Europeans and up to 10% of children and adolescents suffer from fatty hepatosis (or steatosis). In Europe, "fatty liver" develops in 90% of alcohol abusers and 94% of obese people. Regardless of the underlying cause of the pathology, fatty hepatosis with liver enlargement progresses to cirrhosis in 10-12% of patients over eight years. And with concomitant inflammation of liver tissue - to hepatocellular carcinoma.
In addition to alcohol intoxication of the liver and obesity, this disease is associated with impaired glucose tolerance in type II diabetes mellitus and abnormal cholesterol and other fat metabolism (dyslipidemia). From a pathophysiological point of view, fatty hepatosis with or without liver enlargement develops due to damage to fatty acid metabolism, which can be caused by an imbalance between energy intake and expenditure. As a result, abnormal accumulation of lipids, in particular triglycerides, occurs in liver tissue.
Under the pressure of accumulated fat and formed fatty infiltrates, parenchyma cells lose viability, the size of the liver increases, and the normal functioning of the organ is disrupted.
In the early stages, fatty hepatosis may not have obvious symptoms, but over time, patients complain of nausea and increased gas formation in the intestines, as well as heaviness or pain in the right hypochondrium.
Enlarged liver in heart failure
The functional interaction of all body systems is so close that an enlarged liver in heart failure is an indicator of a decrease in blood ejection by the right ventricle of the heart and a consequence of circulatory disorders.
In this case, blood circulation in the liver vessels slows down, venous congestion (hemodynamic dysfunction) occurs, and the liver swells, increasing in size. Since heart failure is most often chronic, prolonged oxygen deficiency inevitably leads to the death of some liver cells. In their place, connective tissue cells grow, forming entire areas that disrupt the functioning of the liver. These zones increase in size and become denser, and along with this, the liver enlarges (most often its left lobe).
In clinical hepatology, this is called hepatocellular necrosis and is diagnosed as cardiac cirrhosis or cardiac fibrosis. And cardiologists in such cases diagnose cardiogenic ischemic hepatitis, which is essentially an enlarged liver due to heart failure.
Enlarged liver in a child
There are many reasons for an enlarged liver in a child. These may include syphilis or tuberculosis, generalized cytomegalovirus or toxoplasmosis, congenital hepatitis or bile duct anomalies.
With such pathogenesis, not only moderate liver enlargement, but also severe liver enlargement with significant compaction of the parenchyma can be established already by the end of the first year of the child’s life.
Enlargement of the liver and spleen in infants – the so-called hepatosplenomegaly or hepatosplenomegaly – is the result of a congenitally elevated level of immunoglobulins in the blood (hypergammaglobulinemia). This pathology, in addition to the enlargement of these organs, is manifested by a delay in the child's overall development, poor appetite, and very pale skin. Enlargement of the liver and spleen (with icteric symptoms) occurs in newborns with congenital aplastic anemia, which occurs due to the destruction of red blood cells, as well as due to extramedullary hematopoiesis – when red blood cells are formed not in the bone marrow, but directly in the liver and spleen.
Fatty hepatosis with liver enlargement in children develops in almost half of cases due to a significant excess of age-related body weight. Although this pathology can occur with some chronic gastrointestinal diseases, after long-term use of non-steroidal anti-inflammatory drugs, antibacterial or hormonal therapy.
Where does it hurt?
What's bothering you?
Diagnosis of liver enlargement
Diagnosis of liver enlargement begins with a physical examination of the patient and palpation of the internal organs of the abdominal cavity to the right of the midline of the abdomen - in the epigastric region.
During a medical examination, the doctor may detect a significant enlargement of the liver. What does this mean? This means that the liver protrudes from under the edge of the costal arch much more than the anatomical norm (in an adult of average height, this is no more than 1.5 cm), and is palpated significantly below the edge of the ribs. Then an enlargement of the liver by 3 cm, an enlargement of the liver by 5 cm, or an enlargement of the liver by 6 cm is stated. But the final "verdict" is made only after a comprehensive examination of the patient, primarily using ultrasound.
An enlarged liver on ultrasound confirms that there is, for example, "an enlarged liver of a homogeneous hyperechoic structure with a shift toward the stomach, the contours are unclear" or that "diffuse hyperechogenicity of the liver and unclear vascular pattern and liver borders are revealed." By the way, in an adult, a healthy liver has the following parameters (on ultrasound): the anteroposterior size of the right lobe is up to 12.5 cm, the left lobe is up to 7 cm.
In addition to ultrasound examination, the following are used to diagnose liver enlargement:
- blood test for viral hepatitis (serum markers of viruses);
- biochemical blood test (for amylase and liver enzymes, bilirubin, prothrombin time, etc.);
- urine analysis for bilirubin;
- laboratory studies of the functional reserves of the liver (using biochemical and immunological tests);
- radiography;
- hepatoscintigraphy (radioisotope scanning of the liver);
- CT or MRI of the abdominal cavity;
- precision puncture biopsy (if necessary to obtain a sample of liver tissue for cancer testing).
Enlargement of the liver lymph nodes during ultrasound examination is noted by hepatologists in all types of liver cirrhosis, viral hepatitis, tuberculosis of the lymph nodes, lymphogranulomatosis, sarcoidosis, Gaucher's disease, drug-induced lymphadenopathy, HIV infection, and pancreatic cancer.
 [ 17 ]
[ 17 ]
What do need to examine?
Who to contact?
Treatment of liver enlargement
Treatment of liver enlargement is the treatment of a symptom, but, by and large, complex therapy of a specific disease that has led to pathological changes in this organ is needed.
Drug therapy for hypertrophied liver should be supported by proper nutrition, diet, and vitamin intake. According to experts, in some diseases accompanied by liver enlargement, damaged parenchyma and normal organ size can be restored.
To regenerate liver cells, ensure their normal functioning and protect them from negative impacts, hepatoprotective drugs are used - special medications for liver enlargement.
The medicinal product Gepabene is a hepatoprotector of plant origin (synonyms - Karsil, Levasil, Legalon, Silegon, Silebor, Simepar, Geparsil, Hepatofalk-Planta). The active substances of the drug are obtained from extracts of medicinal fumitory (protipine) and fruits of spotted milk thistle (silymarin and silibinin). They stimulate the synthesis of proteins and phospholipids in damaged liver cells, inhibit the formation of fibrous tissue and accelerate the process of parenchyma restoration.
This medicine is prescribed for toxic hepatitis, chronic inflammatory liver diseases, disorders of its metabolism and functions with liver enlargement of various etiologies. It is recommended to take one capsule three times a day (during meals). The minimum course of treatment is three months. Contraindications for this drug include acute forms of inflammation of the liver and bile ducts, age under 18 years. For hemorrhoids and varicose veins, Gepabene is used with caution. During pregnancy and lactation, the drug is used only as prescribed by a doctor and under his supervision. Possible side effects include laxative and diuretic effects, as well as the appearance of a skin rash. Taking Gepabene is incompatible with alcohol consumption.
The therapeutic effect of Essentiale (Essentiale Forte) is based on the action of phospholipids (complex fat-containing compounds), which are similar in structure to natural phospholipids found in human tissue cells, ensuring their division and restoration in case of damage. Phospholipids block the growth of fibrous tissue cells, due to which this drug reduces the risk of liver cirrhosis. Essentiale is prescribed for liver steatosis, hepatitis, liver cirrhosis and its toxic damage. The standard dose is 1-2 capsules three times a day (during meals). Side effects (such as diarrhea) are rare.
The drug Essliver differs from Essentiale by the presence in its composition - along with phospholipids - of vitamins B1, B2, B5, B6 and B12. And the combined hepatoprotective drug Phosphogliv (in capsules) in addition to phospholipids contains glycyrrhizic acid, which has anti-inflammatory and antioxidant properties. It helps reduce damage to hepatocyte membranes during inflammation and liver enlargement, as well as normalize metabolic processes. The method of administration and dosage of the last two drugs are similar to Essentiale.
Medicines for liver enlargement include a drug based on the artichoke plant - Artichoke extract (synonyms - Hofitol, Cynarix, Artichoke extract). This drug helps to improve the condition of liver cells and normalize their functioning. Doctors recommend taking this drug 1-2 tablets three times a day (before meals). The course of treatment lasts from two weeks to a month, depending on the severity of the disease. Side effects may include heartburn, diarrhea, pain in the stomach. And contraindications to its use are obstruction of the urinary tract and bile ducts, gallstones, as well as severe forms of renal and hepatic insufficiency.
In addition to the fact that medicinal plants are the basis of many hepatoprotective drugs, herbs for liver enlargement are widely used in the form of home-made infusions and decoctions. For this pathology, herbalists advise using dandelion, corn silk, calendula, sandy immortelle, yarrow, peppermint. The standard recipe for water infusion: for 200-250 ml of boiling water, take a tablespoon of dry grass or flowers, brew with boiling water, infuse until cool, filter and take 50 ml 3-4 times a day (25-30 minutes before meals).
Diet for Enlarged Liver
A strictly observed diet for an enlarged liver is the key to successful treatment. With a hypertrophied liver, you must completely avoid eating fatty, fried, smoked and spicy foods, since such food overloads the liver and the entire digestive system.
In addition, the diet for an enlarged liver is incompatible with such foods as legumes, radishes, horseradish, spinach and sorrel; sausages and spicy cheeses; margarine and spreads; white bread and pastries; vinegar, mustard and pepper; confectionery with cream, chocolate and ice cream; carbonated drinks and alcohol.
Everything else (especially vegetables and fruits) can be eaten, at least five times a day, but in small amounts. It is not recommended to eat after 7 p.m. even if the liver is healthy, and it is absolutely forbidden if the liver is enlarged. But a glass of water with a spoonful of natural honey is allowed and necessary.
The daily diet should contain 100 g of animal proteins, about the same amount of vegetable proteins and 50 g of vegetable fats. The volume of carbohydrate food is 450-500 g, while sugar consumption should be reduced to 50-60 g per day, and salt - to 10-12 g. The daily volume of liquid (excluding liquid food) is at least 1.5 liters.
More information of the treatment
Prevention of liver enlargement
The best prevention of liver enlargement caused by excess weight or addiction to alcoholic drinks, you know what. Here, without following the principles of a healthy lifestyle, nothing will work…
Unfortunately, it is impossible to predict how the liver will behave and how much it can increase, for example, with hepatitis, mononucleosis, Wilson's disease, hemochromatosis or cholangitis. But even in such cases, a balanced diet, taking vitamins, physical exercise, hardening and giving up bad habits will help the liver cope with cleansing the blood of toxins, producing bile and enzymes, regulating protein, carbohydrate and fat metabolism in the body. Also, to help the liver with the threat of hepatomegaly, vitamins of group B, vitamin E, zinc (to restore liver tissue) and selenium (to improve overall immunity and reduce the risk of inflammatory liver diseases) are especially needed.
Liver enlargement prognosis
The prognosis for liver enlargement is quite alarming. Since the pronounced signs of this pathology do not appear immediately, treatment in a third of cases begins when the process reaches the "point of no return". And the most likely consequences of liver enlargement are partial or complete loss of its functional capabilities.

