Medical expert of the article
New publications
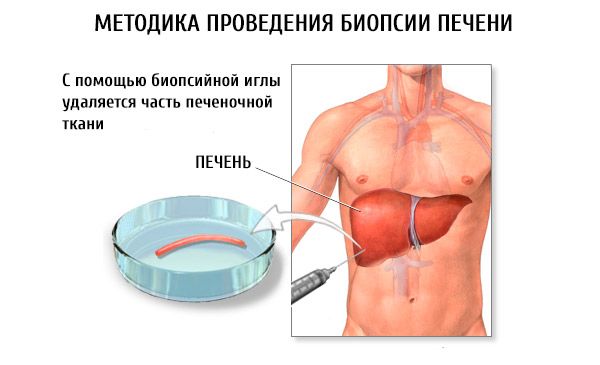
Liver biopsy
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Liver biopsy provides histologic and other information that is not available by other means. Although only a small piece of tissue is examined in a biopsy, the sample is usually representative, even in focal lesions. Ultrasound- or CT-guided biopsy is more effective. For example, in metastases, the sensitivity of ultrasound-guided biopsy is 66%. Biopsy is especially valuable for the diagnosis of tuberculosis or other granulomatous infiltrates and in assessing the condition and viability of the graft (ischemia, rejection, biliary tract disease, viral hepatitis) after liver transplantation. Serial biopsies, usually performed over several years, may be necessary to monitor disease progression.
Macroscopic and histopathological examinations are most often definitive. In some cases, cytological analysis, frozen section examination, and cultures may be required. The biopsy can be used to determine the metal content - copper in case of suspected Wilson's disease and iron in case of hemochromatosis.
Indications for liver biopsy
- Unexplained changes in liver enzyme levels
- Alcoholic liver disease or non-alcoholic steatosis (diagnosis and staging)
- Chronic hepatitis (diagnosis and staging)
- Suspected rejection after liver transplantation that cannot be diagnosed by less invasive methods
- Hepatosplenomegaly of unknown etiology
- Unexplained intrahepatic cholestasis
- Suspected malignancy (focal lesions)
- Unexplained changes in liver enzyme levels
- Unexplained systemic manifestations of the disease, such as fever of unknown etiology, inflammatory or granulomatous diseases (cultures of material obtained by biopsy)
The effectiveness of diagnostic biopsy is limited by the following factors:
- sample collection error;
- random errors or doubts in cases of cholestasis and
- the need for a qualified pathologist (many pathologists do not have experience working with fine-needle biopsy samples).
Liver biopsy can be performed percutaneously at the patient's bedside or under ultrasound guidance. The latter option is preferable, as it is less likely to cause complications and allows visualization of the liver and targeted focal lesions.
Contraindications to liver biopsy
Absolute contraindications include inability to keep the patient still and hold their breath during the procedure, risk of bleeding (INR > 1.2 despite vitamin K, bleeding time > 10 min), and severe thrombocytopenia (< 50,000/mL). Relative contraindications include severe anemia, peritonitis, significant ascites, high-grade biliary obstruction, and subdiaphragmatic or right-sided infected pleural effusion or effusion. However, percutaneous liver biopsy is reasonably safe when performed in an outpatient setting. The mortality rate is 0.01%. Major complications (eg, intra-abdominal hemorrhage, biliary peritonitis, liver rupture) occur in approximately 2% of cases. Complications usually become apparent within 3–4 hours; this is the recommended period for patient observation.
Transjugular hepatic vein catheterization with biopsy is used in patients with severe coagulopathy. The procedure involves cannulation of the right internal jugular vein and passage of a catheter through the inferior vena cava into the hepatic vein. A thin needle is advanced through the hepatic vein into the liver tissue. Successful biopsy is achieved in over 95% of cases, with a low complication rate of 0.2%, bleeding from the puncture site of the liver capsule.


 [
[