Medical expert of the article
New publications
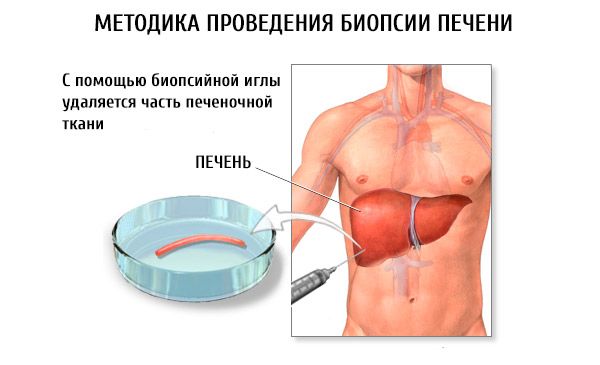
Puncture biopsy of the liver
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Indications for liver biopsy
Puncture biopsy is used mainly when chronic hepatitis or liver cirrhosis is suspected, and in some cases for differential diagnosis of diseases in which the liver is involved in the pathological process (lipoidosis, fatty hepatosis, glycogenosis, etc.), and in cases of jaundice and hepatomegaly of unclear etiology.
Indications for liver biopsy are as follows:
- identification of pathology that caused changes in functional liver tests;
- the need to clarify the diagnosis and determine the prognosis for chronic hepatitis;
- confirmation of the presence and prognosis of the course of alcoholic liver disease;
- diagnostics of systemic diseases in which the liver is involved in the pathological process;
- assessment of the severity and nature (type) of drug-induced liver damage;
- confirmation of multiorgan infiltrative tumor pathology (lymphoma, leukemia);
- screening of relatives of patients with systemic diseases;
- obtaining tissue for culture;
- diagnostics of Wilson-Konovalov disease, hemochromatosis, autoimmune hepatitis, chronic viral hepatitis and assessment of the effectiveness of therapy;
- elimination of transplant rejection reaction;
- exclusion of reinfection or organ ischemia after liver transplantation.
In order to avoid severe consequences caused by parenchymatous bleeding, it is advisable to perform puncture biopsy in a surgical department. After puncture biopsy of the liver, the occurrence of biliary peritonitis, purulent complications (abscess, phlegmon) and even pneumothorax has been described. The development of pleurisy, perihepatitis, the formation of intrahepatic hematomas, hemobilia, the formation of arteriovenous fistula, accidental puncture of the kidney or colon, as well as infectious complications occurring in the form of transient bacteremia, rarely - sepsis have also been described. In general, complications during biopsy in children are more common than in adults, reaching 4.5%. Mortality during puncture biopsy ranges from 0.009 to 0.17%.
How is a liver biopsy performed?
There are percutaneous liver puncture and targeted, laparoscopically or ultrasound-guided liver punctures. Laparoscopically or ultrasound-guided liver punctures are most effective for focal liver lesions. In case of diffuse changes in organ tissue, a "blind" biopsy can be used, and although the location of liver tissue cannot be determined, a high percentage of positive results is achieved, and the simplicity of its implementation makes it accessible to any hepatology department.
In cases of coagulation disorders, massive ascites, small liver size or lack of patient contact, as well as in cases of fulminant liver failure, transjugular liver biopsy is used using a Trucut needle placed in a catheter inserted through the jugular vein into the hepatic vein.
Among the puncture needle systems, the most widely used are the Menghini needle and the Trucut needle (a modification of the Silverman needle). A number of other systems are also used.
A liver puncture biopsy is performed with the patient lying on his back. The skin at the puncture site (usually the ninth and tenth intercostal space on the right between the anterior and middle axillary lines) is treated with an antiseptic solution. After this, a 2% solution of novocaine is used to locally anesthetize the skin, subcutaneous fat, and liver capsule.
The puncture is made with a stylet, inserting it to a depth of 2-4 mm. Then a Menghini puncture needle (a shortened needle is used in pediatric practice) is inserted through the stylet, connected to a 10-gram syringe containing 4-6 ml of isotonic sodium chloride solution. The needle is advanced to the liver capsule and 2 ml of isotonic sodium chloride solution is released to push pieces of fatty tissue out of the needle. The needle is inserted into the liver parenchyma and pieces of organ tissue are aspirated using the syringe plunger. After the manipulation is completed, a sterile adhesive bandage is applied and an ice pack is placed on the puncture site. The patient remains in bed for 24 hours.
It is inappropriate to perform a liver puncture in case of congestive jaundice, pustular rashes on the skin (especially at the site of the intended puncture). A liver puncture biopsy should not be performed against the background of an acute respiratory disease, tonsillitis, or other acute infections.
A tissue column obtained during a liver biopsy can be used to judge changes in the entire organ, especially in diffuse processes (viral hepatitis, steatosis, reticulosis, cirrhosis, etc.). However, a biopsy does not always allow for the diagnosis of focal liver lesions (granuloma, tumor, abscess, etc.). The absence of portal tracts in the biopsy and the small size of the tissue sample can also be the reason for the uninformativeness of a biopsy.
A tissue column height of 1-4 cm and a weight of 10-50 mg are considered sufficient. The tissue sample is usually fixed in 10% formalin in isotonic sodium chloride. The preparations are stained with hematoxylin and eosin, the PAS reaction is performed for the presence of connective tissue, etc. In addition, tissue columns obtained from paraffin blocks can be subjected to retrospective examination. For adequate interpretation of the results, the tissue sample must be at least 2 cm long and contain four portal tracts.
Contraindications to liver biopsy
With adequate liver biopsy technique and strict consideration of all contraindications, the number of complications during this manipulation is relatively small. The most dangerous of them include: bleeding, development of pleural shock, damage to adjacent organs, infection of the pleural or abdominal cavity. It should be remembered that often after liver biopsy, patients experience pain at the puncture site, in the epigastric region, right shoulder and right supraclavicular region. As a rule, these symptoms are not dangerous and go away on their own after some time.
Contraindications to liver biopsy are as follows.
Absolute:
- severe coagulopathy - prothrombin time greater than 3 s or prothrombin index 70% or less;
- the number of platelets in peripheral blood is 60x10 9 /l or less;
- increased bleeding time;
- suspected liver echinococcosis;
- suspected liver hemangioma;
- the patient's refusal to undergo this manipulation.
Relative:
- pronounced ascites;
- right-sided pleurisy;
- cholangitis;
- biliary obstruction of any etiology.


 [
[