Medical expert of the article
New publications
Hysteroscopy for a uterine polyp
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Endoscopic examinations have recently become increasingly popular. And this is not surprising, because they have a great advantage over other diagnostic methods. An endoscope inserted into the cavity of the organs allows you to assess their condition using a three-dimensional image on the monitor screen, identify various neoplasms and, if necessary, even remove them immediately during the diagnostic process. Endoscopic diagnostics are used to examine ENT organs, the gastrointestinal tract, and internal genital organs. In gynecology, hysteroscopy of the uterine polyp has become widespread, during which it is possible to both detect such a neoplasm in a woman's body and successfully remove it or at least take material for histological examination in order to exclude or confirm a malignant process.
Etiology and clinical picture of uterine polyposis
Polyps, wherever they form, are pathological formations from the body's own tissues. In the uterus, the material for such neoplasms is actively dividing cells of the mucous and muscular layer of the uterus. Normally, the growth and reproduction of uterine cells is under the control of the endocrine and immune systems, so malfunctions in the glands responsible for hormonal balance, as well as decreased immunity can be considered a risk factor for the onset of pathological changes in the cells of the uterine mucosa.
Frankly speaking, scientists cannot name the exact reasons that lead to the formation of polyps in the uterus. In addition to hormonal imbalance and decreased immunity, they suspect that inflammatory processes in the gynecological sphere and mechanical damage, which are usually associated with sexual violence or the use of additional means to obtain pleasure, are involved in the appearance of benign formations. But situations with tissue ruptures during childbirth, as well as the consequences of surgical intervention, for example, during abortions and diagnostic curettage, cannot be ruled out.
The uterus in women is called that because it is the main organ of the female reproductive system, in which new life matures over the course of nine months. This pear-shaped organ, located between the bladder and the large intestine, has a complex structure. It is divided into a body with a bottom at the point of attachment of the fallopian tubes, a cervix and an isthmus (a centimeter-long section between the body of the uterus and its cervix). Inside the cervix there is a narrow (only 2-3 mm) cervical canal, covered with glandular tissue, which opens into the vaginal cavity.
The walls of the uterus are considered to be three-layered. The outer layer or perimetrium, which protects the uterus from the outside, consists of connective tissue and is not visible with a hysteroscope. Its disruption is associated with organ perforation. The inner layer of the uterine wall (myometrium) is elastic muscle tissue, which also consists of three layers: superficial, vascular and internal.
And finally, the inner layer of the uterine wall is the endometrium. This is a two-layer mucous membrane of the organ, the basal layer of which (adjacent to the myometrium) remains unchanged, and the functional glandular layer is constantly renewed. As a result of such renewals, the thickness of the endometrium changes depending on the phase of the menstrual cycle. Before menstruation, there is a gradual proliferation of mucous tissues, after which they peel off and come out in the form of menstrual bleeding. Then, the process of regeneration of the inner layer of the endometrium is observed.
All these are physiologically determined processes that occur month after month in the female body. But sometimes in some area of the uterine endometrium, in the cervical canal or at its exit, the process of cell growth gets out of control and unusual growths of a round or oval shape (sometimes with small bulges) are formed, which are connected to the mucous membrane by means of a stalk.
Polyps are usually found in a single specimen. Their sizes may vary, which determines the severity of the pathology symptoms. Small polyps inside the uterus are most often found by chance during an ultrasound examination, because they do not manifest themselves in any way.
Larger or multiple small (in this case they speak of polyposis) formations in the body of the uterus cannot but affect the contractile ability of the organ and the processes occurring inside it. They interfere with the natural renewal of the endometrium and can cause unpleasant and dangerous symptoms in the form of:
- uterine bleeding outside of menstruation,
- the appearance of bloody, brownish or pink discharge not associated with menstruation,
- increased and painful menstrual bleeding,
- "causeless" pain in the lumbar region,
- an unpleasant pulling sensation and pain in the lower abdomen,
- discomfort and pain during intercourse.
Depending on the tissues of which the polyp body is formed, neoplasms are divided into: glandular, glandular-fibrous and fibrous, which are considered not dangerous in terms of degeneration, but can bring a lot of unpleasant symptoms, up to problems with conceiving a child. Such polyps in most cases have a light shade (almost white, beige, light pink), which is what stands out against the background of bright pink mucous. Their size, depending on the tissues of which the polyp consists, ranges from 1.5 to 6 cm. They can be located on a stalk or have a base of a smaller diameter than the body of the growth itself.
The most dangerous are adenomatous polyps, which, although small (up to 1.5 cm), are still associated with a precancerous condition due to the high risk of malignancy of growth cells and significant penetration into deep tissue layers. These are neoplasms with an uneven surface and a grayish tint.
Hysteroscopy is a method of simultaneously confirming the presence of a uterine polyp and removing it. Moreover, the polyp itself (or several neoplasms) can be located both in the cavity of the uterine body and in the cervical canal.
A third of women who have been diagnosed with polyps in the cervix also have them on the endometrium of the organ. Despite their small size (up to 1 cm), cervical polyps carry more serious complications, such as infertility and problematic pregnancy. Therefore, the treatment of polyps in the uterus, which consists of removing neoplasms using various methods, including hysteroscopy, is especially important for women who dream of having their own child. And what is very important, polyps should be removed before pregnancy occurs. After conception, such operations are no longer performed at any stage.
Indications for the procedure
Hysteroscopy of the uterus is a diagnostic examination that a gynecologist prescribes to a woman if there is a suspicion of the development of certain female pathologies, for example, the formation of a polyp, which, although not considered a malignant neoplasm, can significantly worsen the patient's quality of life. In addition, some types of such growths are prone to malignization, which means they may well lead to the development of uterine cancer.
If uterine polyposis is suspected, hysteroscopy is performed both as a diagnostic and as a therapeutic procedure, allowing for the safest and most effective elimination of pathological tissue growths in the organ.
However, hysteroscopy may be prescribed not only for uterine polyps. As a control diagnostic examination, it is prescribed after surgical interventions in the gynecological field (for example, diagnostic curettage, operations on the uterus and ovaries, etc.).
As for diagnostic curettage, which was very popular earlier, but is now being performed less and less due to the lack of visual control over the procedure and a large number of possible complications, hysteroscopy helps to identify and correct the shortcomings of this method. Ideally, endometrial curettage should be performed under the control of an endoscope (in our case, a hysteroscope).
Hyteroscopic diagnostics is often prescribed to monitor the effectiveness of hormonal therapy, as well as to identify pathological causes of infertility (stenosis or blockage of the fallopian tubes, developmental abnormalities of the uterus and ovaries, etc.).
As a therapeutic and diagnostic procedure, hysteroscopy of the uterus can be prescribed in the following cases:
- if bleeding occurs between periods or during menopause, or if there are menstrual cycle irregularities
- if there is a suspicion of various defects in the development and structure of the organ,
- in case of premature spontaneous termination of pregnancy,
- in a situation where various complications arise after childbirth,
- if symptoms indicate the presence of foreign substances in the uterus; foreign bodies may include:
- intrauterine contraceptive devices that tend to adhere to uterine tissue or cause perforation of the walls,
- small fragments of bone tissue that can damage the integrity of the uterine walls,
- fragments of the placenta and fertilized egg remaining after childbirth or abortion,
- ligatures that have an irritating effect on the endometrium.
- if there is reason to suspect a breach in the integrity of the uterine walls ( perforation or puncture),
Hysteroscopy of the uterus is a very useful diagnostic procedure when there is a suspicion of damage to various internal layers of the organ wall (muscular and mucous layer). This refers to inflammatory processes, mechanical damage or pathological proliferation of internal tissues of the uterus (dysplasia).
If you look more closely, you can see that polyps on the uterine mucosa are one of the variants of dysplasia, because they are also formed from the body's own tissues. Let's try to clarify the situation with what polyps are, what types they are, what are the dangers and what symptoms can cause the doctor to suspect uterine polyposis.
Preparation
Since hysteroscopy of a uterine polyp involves not only diagnostic but also therapeutic manipulations, which are equivalent to surgical intervention, such treatment cannot be carried out without special preparation, especially when it involves the use of anesthesia.
First, the patient must be examined by a gynecologist, who makes a preliminary diagnosis. Examination on a chair with mirrors cannot give a complete picture of what is happening inside the cervical canal and uterus. At first, the doctor relies on the changes that are noticeable during a regular gynecological examination on the chair, anamnestic information and the patient's complaints, if any.
If the doctor suspects the presence of polyps in the uterus and offers the woman such a study as hysteroscopy, which in most cases ends with surgery, he must inform the patient about all the nuances of this procedure: how hysteroscopy of the uterine polyp is performed, how to prepare for the procedure, what methods of anesthesia exist, predicted results and all possible risks. If the woman gives her consent to manipulations with a hysteroscope, she is prescribed a comprehensive examination.
Numerous tests prior to hysteroscopy of the uterus aimed at confirming and removing a polyp (or polyps) include:
- collection of material and a general blood test, which will help to clarify whether there is an acute inflammatory process in the body, most often associated with the activation of an infectious factor,
- conducting a blood clotting test ( coagulogram ),
- blood biochemistry (detailed analysis),
- a blood sugar test to rule out severe forms of diabetes, in which any wounds heal very poorly, including postoperative ones,
- collection of material and conducting a general urine analysis, indicating the state of the genitourinary system.
All these tests are necessary to prevent various complications during and after surgery, but they do not provide sufficient information to confirm the diagnosis. Instrumental studies help to clarify the diagnosis:
- Ultrasound of the abdominal cavity and pelvic organs,
- transvaginal ultrasound, which is similar to an endoscopic examination, but without subsequent surgery (it helps not only to detect polyps, assess their size and structure, but also to identify a possible pregnancy in its early stages, since surgery in this case becomes impossible).
In principle, a clear picture of polyps in the uterus can be seen after an ultrasound diagnosis. But it is not enough to simply detect a polyp. The problem of polyps in the uterus cannot be solved with medications. And hormonal therapy, prescribed in severe cases of polyposis, is considered an auxiliary method. And the main method is still the removal of polyps by all possible methods (hysteroscopies, surgical curettage, laser removal, cryodestruction, exposure to electric current or radio waves).
But the hysteroscopy procedure also has certain contraindications that require a more thorough examination of the patient. Therefore, an additional examination of the woman is carried out on a gynecological chair, during which the doctor palpates the abdominal area from the outside and inside through the vagina, which makes it possible to identify anomalies for which the operation is contraindicated. During manipulations on the chair, the gynecologist takes smears of microflora from the vagina, since intracavitary operations are not performed if there is a bacterial or fungal infection in the lesion.
The condition of the lungs and respiratory system can be judged by the chest X-ray, and possible heart pathologies can be determined by the electrocardiogram (ECG). This information is especially important for effective and safe anesthesia.
Some diagnostic procedures require additional preparation. So, in order for smears for microflora to give real results, doctors do not recommend douching, using any vaginal tablets, including contraceptives, or having sexual intercourse for a week before the analysis. It is necessary to inform the doctor about any medications taken, as well as about intolerance to various types of anesthetics.
Determining the date of the operation is also very important. The fact is that the uterine endometrium is constantly changing. It is recommended to remove polyps on the days when the thickness of the uterine mucosa is minimal and neoplasms are clearly visible both in the body and in the area of the leg. Surgical interventions are not usually performed during menstruation, but the minimum thickness of the endometrium is observed for another 3-5 days after the end of critical days. It is on these days that it is recommended to perform hysteroscopy. In extreme cases, it will be necessary to fit into the first 10 days of the initial phase of the menstrual cycle.
Preparation for the examination on the eve of the procedure involves refraining from eating for 6-8 hours before the examination. This also applies to drinking water and other liquids. In addition, immediately before the hysteroscopy, it is necessary to empty the bladder.
Technique uterine polyp removal
Hysteroscopy can be performed for diagnostic and therapeutic purposes. When polyps in the uterus have been detected using other types of examinations, diagnostics using a hysteroscope no longer plays a decisive role, it only allows you to more accurately determine the size and location of the neoplasms in order to develop the most effective tactics for their removal.
Hysteroscopy of the uterine polyp as a treatment procedure usually follows immediately after the diagnostic assessment of the tissue condition and is an operation on the uterus, which in most cases does not require the removal of the reproductive organ itself. Such a need arises if adenomatous neoplasms were detected in the uterus, and histological examination (biopsy) confirmed the fact of the degeneration of polyp cells into malignant ones. In this case, removal of the uterus is aimed at preventing the spread of tumor metastases throughout the body.
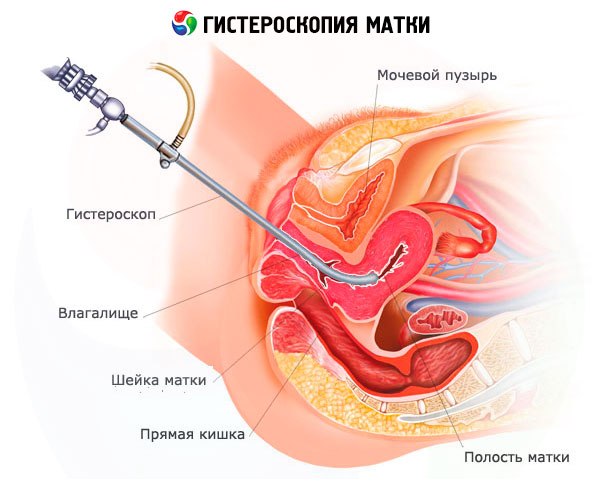
Diagnostic and therapeutic procedures are performed using a hysteroscope, which resembles a probe with a camera at the end and taps, through which a composition is introduced and removed into the cavity, helping to expand the cavity and smooth out its borders. This can be liquid or gas.
Hysteroscopes can have different sizes. The surgical device is larger than the diagnostic one, and it is also equipped with a channel through which additional instruments that may be needed during treatment (catheters, scissors, laser conductors, loop electrode, curette, etc.) are delivered to the surgical site. At the end of the probe, in addition to a microcamera that displays the image on the computer screen, there is a light source.
Hysteroscopy of endometrial and cervical polyps is performed in the operating room of a gynecological hospital, in specially equipped rooms of perinatal centers and gynecological clinics, and less often in outpatient settings (office hysteroscopy). The operation to remove a polyp can be classified as a simple intervention if we are talking about small polyps. Single small polyps can be removed on an outpatient basis.
Removal of large growths is considered a complex operation that requires not only special equipment, but also considerable experience and knowledge of the surgeon. In severe cases, hysteroscopic removal of polyps in the uterus is performed after a course of hormonal therapy.
But whatever the operation to remove polyps in the uterus, it is performed under general or regional anesthesia. Anesthesia for hysteroscopy of the uterus and removal of polyps is selected individually, taking into account the characteristics of the patient's body and the complexity of the operation.
Local anesthesia, which is performed by injecting the uterus with lidocaine or other anesthetics, is indicated mainly during diagnostic procedures. Treatment of the entrance to the uterus with anesthetics is also performed in cases of small single polyps or the impossibility of general anesthesia.
However, in the vast majority of cases, preference is given to general anesthesia. In this case, anesthetics are administered intravenously or through a laryngeal mask (inhalation anesthesia). Inhalation anesthesia is considered a safer method of anesthesia, since it causes fewer side effects in the form of dizziness, nausea, and myalgia. And the general condition of the patient after such anesthesia is better than after intravenous infusion of anesthetics.
A more modern method of anesthesia is regional anesthesia. The anesthetic is injected into the spine as close to the spinal cord as possible. As a result, the patient temporarily loses sensitivity in the lower part of the body, while remaining fully conscious.
This method completely eliminates the occurrence of unpleasant symptoms characteristic of general anesthesia, but it is more difficult to perform and also requires additional time and professionalism of the anesthesiologist.
The use of general and regional anesthesia requires the presence of an anesthesiologist next to the patient not only during the operation. Within 24 hours after the procedure, the specialist doctor must monitor the patient's condition and leave his post only if the vital signs are satisfactory.
The second stage after anesthesia can be considered manipulations to expand the uterine cavity. First, using a special instrument, the diameter of the cervical canal is increased so that the hysteroscope tube can be freely inserted into the uterine cavity. Then, using a tap, the cavity is filled with gas or liquid.
The gaseous filler is usually carbon dioxide, which is supplied to the uterine cavity using a special device called a hysteroflator. In this case, it is necessary to control the rate of gas supply and its pressure inside the uterus, since high rates can cause cardiac dysfunction, rupture of pulmonary vessels and air entering the blood, which can even lead to death.
Liquid filler may include dextran (rarely used due to the increased risk of anaphylaxis and high cost of the product), distilled water, solutions of sodium chloride, glucose, glycine, Ringer's solution. In this case, the volume and pressure of the supplied liquid must be monitored during the operation.
One of the disadvantages of liquid hysteroscopy is the heavy load on the vessels. Plus, there is a risk of infectious complications. However, in most cases, liquids are chosen as a means of filling the uterine cavity during surgical operations, while diagnostics can also be carried out using carbon dioxide.
It is important to understand that the fluid in the uterine cavity is not stagnant. It washes the organ and must flow out freely. That is, the inflow and outflow of fluid must be constant. The latter is achieved using a Hegar dilator, which increases the free space of the cervical canal (this is also very convenient when removing large polyps that have to be extracted through a narrow space inside the cervical canal). During gas hysteroscopy, the gas is drained using a special tap, after which the uterine cavity is washed with an antiseptic solution.
The device is inserted into the uterus slowly and very carefully. First, the doctor examines the cavity of the organ and the mucous membrane of the cervical canal, noting the location of the polyps, their size and structure. If the polyps are to be removed at another time, the doctor simply takes the material for biopsy using additional instruments that the doctor controls with a hysteroscope. In the case of a planned operation and in the case when it is possible to excise pathological growths immediately after diagnosis, the removed polyp serves as the material for histological examination.
Removal of a polyp during hysteroscopy of the uterus can be performed in various ways. Mechanical removal of neoplasms involves the use of surgical instruments (forceps and scissors), which are fed to the site of the operation using a hysteroscope.
Hysteroscopy of cervical polyps is facilitated by the fact that such neoplasms are small in size and are located on a thin stalk. Removal of such polyps can be performed even under local anesthesia. Usually, the growth is first rotated several times relative to the stalk (unscrewed), after which it falls off and is extracted using hysteroscope instruments. The place where the polyp is attached to the mucous membrane is additionally scraped using a special loop (curette).
If special equipment is available, excision of the polyp stalk and cleaning of its location can be carried out using electric current or laser.
Removal of endometrial polyps of the uterus in case of small neoplasms located on a thin stalk can be performed by the same methods as polyps in the cervical canal. If we are talking about large growths, then after unscrewing them, the stalk is excised using a resectoscope or plastic scissors (polypectomy).
If the polyps have an irregular shape (for example, they lack a stalk, like parietal polyps) or their location in the mouth of the fallopian tubes complicates the usual method of performing surgery by unscrewing the growth, excision of such growths can be carried out immediately with a resectoscope. But if such an opportunity exists, it is better to resort to safer methods of electrosurgery or laser removal of the neoplasm with subsequent cauterization of the location of the polyp, which is possible in both cases.
In electrosurgery, cauterization of tissue at the site of polyp removal is called electrocoagulation. The laser simultaneously excises tissue and seals the vessels, which prevents bleeding.
In general, the operation to remove polyps in the uterus using a hysteroscope does not take much time. A single polyp in the cervix is usually removed in no more than 15-20 minutes. In more severe cases, it takes a little more than half an hour to remove polyps.
Repeat hysteroscopy
Repeated hysteroscopy of the uterus is a common procedure after removal of polyps localized in the endometrium of the organ. It is performed to monitor the results of treatment. But in some cases, repeated hysteroscopy is prescribed some time after mechanical removal of polyps, because these neoplasms are prone to relapse.
And although the recurrence of polyps in the same place or nearby is not considered a very frequent complication (according to various sources, from 3 to 10% of cases of removal of polyps in the uterus), this fact cannot be ignored. Most often, in case of recurrent polyps, they resort to laser removal, since it gives more lasting results, because the laser is able to penetrate into the deep layers of tissue. However, the process of polyp formation does not stop in all cases. Relapses may not be isolated, which already indicates serious problems in the body that require special treatment, for example, hormonal therapy.
In this case, hormonal treatment is performed first, and then hysteroscopy of the uterine polyp with subsequent cauterization of the endometrial tissue. Hormonal therapy is sometimes replaced by diagnostic curettage, which has fewer complications than hormonal therapy, after all, the uterine mucosa is characterized by rapid tissue recovery, which cannot be said about the body after exposure to hormones.
Contraindications to the procedure
Like any surgical intervention, removal of uterine polyps is not prescribed to all patients. Some contraindications can be considered absolute, and then you have to look for other methods of combating uterine polyposis. Other restrictions can be dealt with by conducting effective treatment of the identified pathology or by waiting the necessary time.
Absolute contraindications to hysteroscopy of uterine polyps include:
- Pathological changes in the endometrium of the uterus that are not amenable to treatment (the presence of coarse, inelastic scar tissue due to tissue damage during childbirth or cervical stenosis, when access to the organ and the possibility of its expansion are limited).
- Severe pathologies of various organs and systems in the decompensation stage (complicated arterial hypertension, excessively high blood glucose levels, leading to severe diabetes mellitus, etc.).
- Oncological pathologies of the uterus. If malignization of cells of a polyp located in the cervix is detected, its removal by hysteroscopy is a certain danger, because with the flow of fluid, malignant cells can spread not only throughout the entire organ, but also beyond its limits, for example, into the abdominal cavity.
- A blood clotting disorder that is associated with a high risk of bleeding and significant blood loss during surgical procedures.
Relative contraindications include:
- Pregnancy. Any manipulations in the cervix area are fraught with an increase in its tone and the risk of premature birth and miscarriage, not to mention the introduction into the uterine cavity, where the child is growing and developing at this time. The possibility of removing polyps in the uterus using a hysteroscope after delivery is discussed.
- Menstruation. Despite the fact that during menstrual bleeding the thickness of the endometrium is small, which makes it possible to easily detect and remove polyps, there are certain limitations in the visualization of the operation, so the procedure is prescribed when menstrual flow becomes scanty or absent altogether (from day 5 to day 10 of the menstrual cycle).
- Uterine bleeding caused by tissue hyperplasia or any other pathology. Again, the reason is the limited visibility of the manipulations performed and the inability to qualitatively assess the result of the operation. In this case, hysteroscopy of polyps is performed after the bleeding has stopped. Additionally, it may be necessary to wash the uterus with sterile solutions so that blood clots do not distort the real picture of events.
- Inflammatory pathologies of gynecological organs in the acute stage. Most often, such pathologies are associated with a violation of the vaginal microflora (dysbiosis) and the activation of a bacterial, viral or fungal infection. It is clear that surgical intervention will contribute to the complication of the situation and the spread of pathogenic microflora throughout the body (generalization of the process). First, effective treatment of the pathology is carried out and only after the infection is defeated, can we talk about surgery.
- Systemic infections, including acute respiratory viral infections, flu, tonsillitis and other respiratory infectious and inflammatory diseases. There is nothing to say about this. Intervention is possible only after an effective course of treatment for the underlying disease.
- Relapses of various pathologies of organs and body systems (exacerbation of peptic ulcer, gastritis, bronchial asthma, etc.) due to a large load on the body. The operation can be performed upon reaching the stage of stable remission.
Surgery to remove uterine polyps is not performed in patients who are in serious condition due to somatic pathologies. First, the patient's condition must be stabilized, and then a possible operation can be discussed.
Consequences after the procedure
The consequences of any operation are directly related to the level of professionalism of the medical staff involved in the procedure. For example, an anesthesiologist must not only determine the safe administration of anesthesia and effective drugs, but also correctly calculate the dose of drugs, which will help avoid many complications during and after the operation.
The surgeon's accuracy will help prevent the development of inflammation after accidental damage to the healthy uterine mucosa or perforation of the organ. Preparation and disinfection of instruments by junior medical staff. Antimicrobial measures by the surgeon and his assistants will help avoid infection of wounds after removal of polyps, which significantly slows down the process of recovery and restoration of the endometrium.
The only consequences of uterine polyp hysteroscopy that cannot be ruled out are considered to be slight discomfort and mild pain in the lower abdomen for several days after the operation. After all, there was an intervention in the organ's work and damage to its tissues, so there is nothing surprising or dangerous in such symptoms. If a woman has a hard time with pain, it can be relieved with rectal suppositories with an analgesic effect, but this is usually not necessary.
Scanty spotting or bloody discharge from the genitals after hysteroscopy of the uterine polyp is also considered normal. This symptom can be observed for 2-3 weeks after the procedure. However, if the discharge increases and is accompanied by noticeable pain, there is every reason to consult your doctor.
Another suspicious symptom indicating possible complications is an increase in body temperature. In principle, with uterine polyposis after surgery, an inflammatory process is observed in the endometrium, not associated with pathogenic microflora. Body temperature may increase slightly, but will return to normal in 2-3 days. If there is a strong increase in body temperature or subfebrile temperature lasts for 5 or more days, this already indicates that the inflammatory process has dragged on, and most likely it is associated with an infection.
In this case, doctors prescribe antibacterial drugs (injections or tablets). Additionally, anti-intoxication agents and hormonal therapy may be prescribed. Hysteroscopy in combination with curettage of the uterine cavity is quite often practiced.
 [ 10 ]
[ 10 ]
Complications after the procedure
Despite the advancement of the hysteroscopy method for uterine polyps, the operation does not always proceed without complications. Too many factors influence the outcome of the operation and the safety of its implementation. So complications can appear not only in the postoperative period (for example, in the form of inflammation), but also during medical manipulations.
Hysteroscopic removal of polyps in the cervix and its body in the vast majority of cases is performed under general or local anesthesia. Regardless of the type of anesthesia, there is always a risk of developing allergic reactions, including severe ones (Quincke's edema, anaphylactic reactions). To avoid such complications, anesthetic tolerance tests must be performed before the operation. The anesthesiologist must clarify the presence of pathologies of the respiratory and cardiovascular systems in order to correctly calculate the dose of drugs and the time of their action.
Since the polyp excision surgery is performed using fluids to expand the uterus, it is very important to control their volume and pressure, which will help to avoid complications such as high blood pressure, pulmonary edema, anaphylactic reactions. In patients with diabetes, the use of glucose solution is not recommended.
Other unpleasant things may happen during the operation. For example, perforation of the uterine wall due to the surgeon's carelessness or weakness of the membrane itself. In addition to the uterus, other organs located nearby may also be damaged. Uterine bleeding during the procedure may also result from perforation of the uterine wall and damage to the myometrium vessels.
Now a little about the troubles that can await a woman a few minutes, days or weeks after the operation. Firstly, this is inflammation of the endometrium ( endometritis ), caused by an infectious factor, for which antibiotic therapy is mandatory.
Secondly, bleeding, which may appear after the operation. In connection with this symptom, hemostatic agents are prescribed and the causes of bleeding are identified using the same hysteroscopy. In some cases, the bleeding is not so great, but is accompanied by cervical stenosis, which makes it difficult to remove blood, and stagnation inside the organ is fraught with inflammatory processes. Regular antispasmodics will help to relax the muscles of the cervix a little.
Thirdly, with polyposis of the uterus and large polyps, severe damage to the endometrium is observed, which can become inflamed even in the absence of infections. And inflammation is fraught with the development of adhesions in the organ. For women during menopause, this complication will only bring slight discomfort (the stomach may pull a little), but for patients of childbearing age, this can threaten infertility.
Removal of a polyp containing malignant cells that were not detected during histological examination is also dangerous. Incomplete removal of a polyp threatens the spread of the malignant process deeper or to nearby tissues.
And, of course, with any method of removing polyps, there is always a certain probability of their relapse, which does not mean giving up the fight against the disease. You should always remember the danger of degeneration of polyp cells.
 [ 11 ]
[ 11 ]
Care after the procedure
Depending on the method of performing surgical intervention on the uterus, the severity of the pathology and the type of surgery (urgent or planned), the postoperative period after removing a polyp using hysteroscopy of the uterus will proceed differently. If the operation was planned in advance, i.e. all necessary studies were carried out, and there were no complications, the patient will be able to leave the clinic the next day or after the anesthesia wears off. But this does not mean that she will be able to return to her normal life, because failure to comply with certain requirements can lead to various complications.
So, what recommendations can you hear after a hysteroscopy of a uterine polyp:
- If the doctor deems it necessary, he can prescribe anti-inflammatory and antibacterial therapy, which should not be refused under any circumstances.
- The patient may also be prescribed hormonal therapy when it comes to large areas of damage or the presence of adhesions. Such treatment will help the uterine mucosa to recover faster without complications of the adhesion process and relapses of polyposis.
- Hormonal therapy can also be prescribed for hormonal imbalance, which is the reason for the polyp. The treatment regimen may include both regular hormones and hormonal contraceptives. You will have to take them despite the risk of gaining weight.
- If the operation was performed without a preliminary full examination of the patient and the material for histology was not taken in advance, the removed polyp will serve as a biopsy. The biopsy results come in a few days. It is imperative to take them and save them for the future. If the analysis confirms oncology (uterine cancer), an additional operation will be urgently scheduled, the purpose of which will be the removal of the uterus.
- Now, regarding sexual activity. It is worth limiting it for some time. How long you need to abstain from traditional sex (one week or a month) will be determined by your doctor. But you should remember that premature start of active sexual activity is fraught with various complications, including bleeding and infection of the body.
- For 2-3 weeks, the doctor will advise you to refrain from hot procedures (solarium, bath, sauna, hot foot baths) in order to avoid provoking bleeding.
- As for douching, in this case it is not relevant and even dangerous. Firstly, the uterus is capable of cleaning itself without our help. Secondly, douching without need only contributes to the washing out of beneficial microflora from the vagina and weakening of local immunity. Thirdly, the lack of sterility of the devices and utensils used can lead to infection of the body from the outside. The doctor himself will say when this treatment and preventive procedure will be necessary.
- You should also not use vaginal tablets, suppositories or hygienic tampons for at least 2 weeks before the repeated hysteroscopic examination. Based on the results of the biopsy and assessment of the condition of the endometrium, the doctor may cancel some restrictions or prescribe additional procedures.
As for menstruation, you can expect it to appear on the same days as before the operation. However, in some cases there was a slight shift in the menstrual cycle (menstruation began earlier or later than expected, but not more than a week), which is not considered a pathology. Unusually heavy discharge, as well as an increase in the duration of menstruation during the recovery period, can also be considered normal. Later, everything will get better without outside interference.
Another thing is if heavy periods start to resemble bleeding. In this case, it is better to rush to the doctor, because it is very difficult to independently distinguish the border between the norm and pathology.
Now the question that interests many young women: when can pregnancy occur after hysteroscopy of the uterus? Let's be honest, everything is strictly individual. It is clear that in the first month, when sexual contacts are limited, pregnancy is out of the question. But in the following months, such an outcome is not excluded, because hysteroscopy of the uterine polyp does not affect the ability to conceive in any way. Moreover, many women were able to get pregnant in the first six months, and all thanks to hysteroscopy.
But there is one nuance here. Early pregnancy can end very badly, because the uterine mucosa needs time to fully recover, and this is at least three months.
How to prevent unwanted pregnancy? With the help of hormonal contraception, which should be prescribed by the attending physician for a period of 3 or 4 months. There is no need to be afraid of this, because the cancellation of such drugs only increases the chances of conceiving a child due to the rebound effect. So getting rid of polyps plus increasing the chances of pregnancy due to hormonal therapy becomes a real opportunity for a woman to become a mother in the near future, something she could only dream of before the operation.
 [ 12 ]
[ 12 ]
Feedback on the procedure
Despite possible complications and risks, most reviews of the hysteroscopies procedure for uterine polyps are positive. Some women note that after reading negative reviews about the operation, they were more afraid than they should have been. In the vast majority of cases, the operation was successful, painless and without dangerous consequences.
Many were initially scared by the need for general anesthesia. Not even the anesthesia itself and the associated risk of allergic reactions and overdose, but the process of recovery from it, accompanied by dizziness, nausea, vomiting, headaches and muscle pain, aching in the lower back. In fact, the operation did not last long, so almost no one had complications from anesthesia, except for particularly sensitive patients.
Even those who had polyps removed under local anesthesia did not complain of pain or discomfort during the operation. Postoperative symptoms in the form of scanty discharge from the genitals, minor nagging pain and discomfort in the lower abdomen, and a short-term increase in temperature did not bother women much and passed without consequences.
Control hysteroscopic examination showed few complications. And relapses of polyps, according to reviews, can be considered isolated complications not related to the procedure itself. After all, subsequent treatment with hormonal agents and drugs that increase general and local immunity led to stabilization of the condition and polyps did not appear again after removal.
Many women are simply happy with the opportunity to become a mother. In most cases, pregnancy was diagnosed after 5 months or more. But some were lucky enough to get a positive pregnancy test result even earlier than this (after 3-4 months, as soon as the endometrium has fully recovered).
But before the operation, many women did not even hope for such a miracle, considering themselves incapable of reproducing a new life. And the fact that the operation was not complicated, went without complications and was relatively inexpensive, only increases the joy of those who still talk to their tummy, and those who have already seen the heir with their own eyes and were able to put him to their breast.
It is clear that no procedure, much less a full-fledged surgical intervention, can do without negative reviews. But such reviews speak to a greater extent not about the weak effectiveness of treatment, but about the lack of professionalism and carelessness of specific doctors and anesthesiologists working in individual clinics. It is with them that women associate complications that arise during or after surgery. No one writes about non-compliance with the requirements of postoperative care, but this could also have affected the outcome of treatment.
Hysteroscopy of a uterine polyp is a procedure that combines 2 types of manipulations: diagnostic and therapeutic, which is very convenient for urgent operations. If the research protocol and the operation technique are followed, the removal of polyps is considered quite safe and does not cause much discomfort, especially since the intervention on the organs is not carried out blindly. The doctor can control any movement of the instruments and situations that arise during the procedure, which means that poor-quality removal of polyps is practically excluded, especially if a laser is involved. We can confidently say that this method has a future and development prospects, despite the fact that getting rid of polyps using this technique has already become an ordinary medical procedure.

