Medical expert of the article
New publications
Uterus
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

The uterus (Greek metra) is an unpaired hollow muscular organ in which the embryo develops and the fetus is carried. The uterus is located in the middle part of the pelvic cavity behind the bladder and in front of the rectum. The uterus is pear-shaped, flattened in the anteroposterior direction. The uterus has a fundus, body and neck.
The fundus of the uterus (fundus uteri) is the upper convex part of the organ, protruding above the line where the fallopian tubes enter the uterus, below is the body of the uterus (corpus uteri), forming the middle (large) part of the organ. Below, the conical body of the uterus passes into a rounded part - the cervix (cervix uteri). The place where the body of the uterus passes into the cervix is narrowed and is called the isthmus of the uterus (isthmus uteri). The lower part of the cervix protrudes into the cavity of the vagina, therefore it is called the vaginal part (portio vaginalis [cervicis]), and the upper part of the cervix, lying above the vagina, is called the supravaginal part of the cervix (portio supravaginal [cervicis]). On the vaginal part, the opening of the uterus (ostium uteri), or cervical os, is visible. This opening leads from the vagina into the cervical canal and continues into its cavity. In women who have not given birth, the opening of the uterus is round or oval, and in women who have given birth, it has the shape of a transverse slit. The opening of the uterus is limited by the anterior lip (labium anterius) and the posterior lip (labium posterius). The posterior lip is thinner.
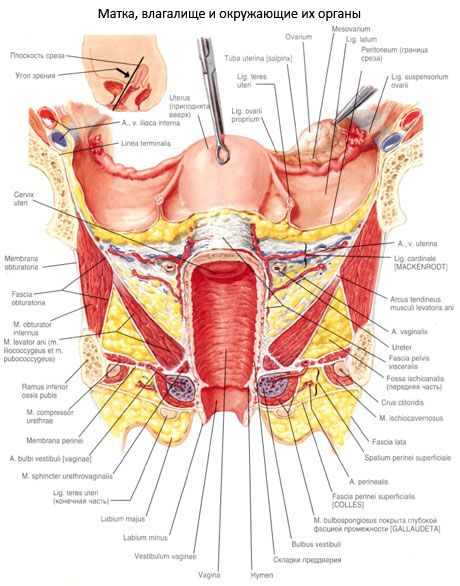
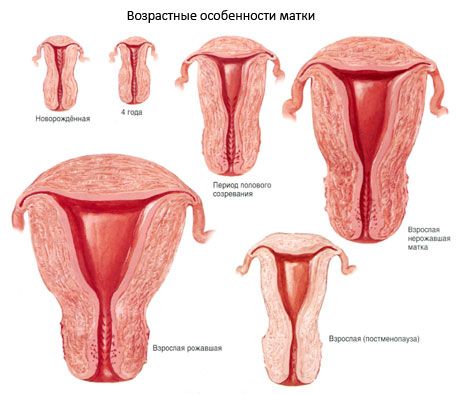
The uterus has anterior and posterior surfaces. The anterior surface of the uterus, facing the urinary bladder, is called the vesical surface (facies vesicalis), and the posterior surface, facing the rectum, is called the rectal surface (facies rectalis). These surfaces of the uterus are separated from each other by the edges of the uterus, right and left (margo uteri dexster et margo uteri sinister). The size and weight of the uterus vary individually. The length of the uterus in an adult woman is on average 7-8 cm, width - 4 cm, thickness 2-3 cm. The weight of the uterus in nulliparous women ranges from 40 to 50 g, and in parous women it reaches 80-90 g.
Structure of the uterus
The wall of the uterus is distinguished by its considerable thickness and limits the narrow cavity of the uterus (cavitas uteri), which has the shape of a triangle in the section in the frontal plane. The base of this triangle faces the fundus of the uterus, and the apex is directed downwards, towards the cervix, where its cavity passes into the cervical canal (canalis cervicis uteri). The latter opens into the cavity of the vagina through the opening of the uterus. The upper angles of the uterine cavity narrow in the form of funnel-shaped depressions into which the uterine openings of the tubes open.

The wall of the uterus consists of three layers. The superficial layer is represented by the serous membrane (tunica serosa), which is also called the perimetrium. This is a sheet of peritoneum covering the uterus from the front and back. The subserous base (tela subserosa) in the form of loose fibrous connective tissue is present only in the area of the cervix and on the sides, where the peritoneum covering the uterus passes into the broad ligaments of the uterus.
The connective tissue on the sides of the uterus with the blood vessels located in it is called the parauterine tissue - parametrium. The middle layer of the uterine wall is the muscular membrane (tunica muscularis), or myometrium (myometrium), the thickest. The myometrium consists of complexly intertwined bundles of smooth muscle tissue, as well as a small number of connective tissue bundles containing elastic fibers. In accordance with the predominant direction of the muscle bundles in the myometrium, three layers are distinguished: internal oblique-longitudinal, middle circular (circular) and external oblique-longitudinal. The most powerful layer is the middle circular layer, which contains a large number of blood, lymphatic vessels and especially large veins, in connection with which this layer is called the vascular layer; the circular layer is most strongly developed in the area of the cervix. The submucosa in the walls of the uterus is absent.
The mucous membrane (tunica mucosa), or endometrium, forms the inner layer of the uterine wall, its thickness reaches 3 mm. The surface of the mucous membrane of the uterus is smooth. Only the cervical canal has one longitudinal fold and smaller palmate folds (plicae palmatae) extending from it in both directions at an acute angle. These folds are located on the anterior and posterior walls of the cervical canal. Touching each other, the palmate folds prevent the contents of the vagina from entering the uterine cavity. The mucous membrane is lined with a single-layer columnar (prismatic) epithelium. It contains simple tubular uterine glands (glandulae utennae).
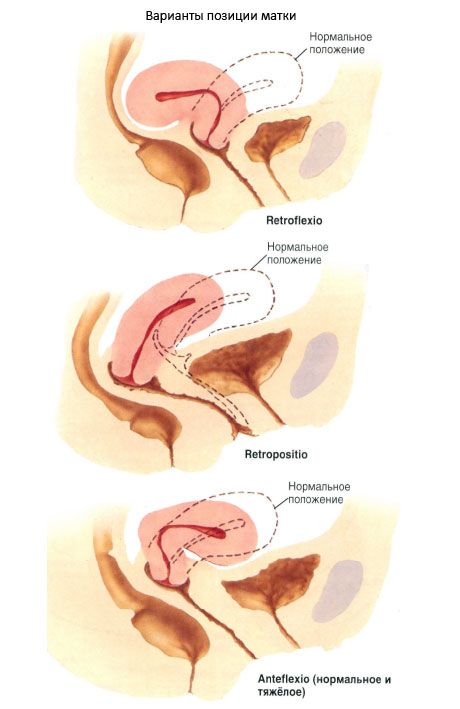
The uterus as an organ is largely mobile. Depending on the condition of the adjacent organs, it can occupy different positions. Normally, the longitudinal axis of the uterus is oriented along the pelvic axis. When the bladder is empty, the fundus of the uterus is directed forward - the uterus is tilted forward (anteversio uteri). When tilted forward, the body of the uterus forms an angle with the cervix that is open to the front - the forward bend of the uterus (anteflexio uteri). When the bladder is full, the fundus of the uterus moves backward and the uterus straightens out slightly. The uterus is slightly tilted to the right (more often) or to the left (lateropositio literi). In rare cases, the uterus is tilted backward (retroversio uteri) or curved backward (retroflexio uteri).
Relationship of the uterus to the peritoneum
Most of the surface of the uterus is covered by the peritoneum (except for the vaginal part of the cervix). From the area of the fundus of the uterus, the peritoneum continues onto the vesical (anterior) surface and reaches the cervix, then passes onto the urinary bladder. This deep pocket, which does not reach the anterior part of the vaginal vault and is formed by the peritoneum, which also covers the posterior surface of the urinary bladder, is called the vesicouterine pouch (excavatio vesicouterina). The peritoneum covering the rectal (posterior) surface of the uterus reaches the posterior wall of the vagina, from where it rises upward onto the anterior wall of the rectum. When passing from the uterus to the rectum, the peritoneum forms the rectouterine pouch (excavatio rectouterina), the Douglas pouch. On the right and left, this pouch is limited by the rectouterine folds of the peritoneum, which extend from the cervix to the rectum. The recto-uterine pouch descends (protrudes) into the pelvic cavity deeper than the vesico-uterine pouch. It reaches the posterior part of the vaginal vault. At the base of the recto-uterine folds of the peritoneum lies the recto-uterine muscle (m. rectouterinus) with bundles of fibrous fibers. This muscle begins on the posterior surface of the cervix in the form of flat bundles, passes through the thickness of the peritoneal folds, bypassing the rectum from the side, and is attached to the periosteum of the sacrum.
Ligaments of the uterus
At the edges of the uterus, the peritoneal layers covering its vesical and rectal surfaces come together to form the right and left broad ligaments of the uterus. The broad ligament of the uterus (lig. latum uteri) consists of two layers of the peritoneum - anterior and posterior. In its structure and purpose, it is the mesentery of the uterus (mesometrium). The right and left broad ligaments of the uterus are directed to the lateral walls of the small pelvis, where they pass into the parietal layer of the peritoneum. In the free upper edge of the broad ligament of the uterus, between its layers, is the fallopian tube. The section of the broad ligament adjacent to the fallopian tube is called the mesentery of the tube (mesosalpinx). Between the layers of the mesentery are the ovarian appendages. Slightly below the attachment of the ovarian ligament to the uterus, the round ligament of the uterus (lig.teres uteri) originates from the anterolateral surface of the uterus. This ligament is a rounded, dense fibrous cord 3-5 mm thick containing muscle bundles. The round ligament of the uterus is located between the leaves of the broad ligament of the uterus, directed downwards and forwards to the deep opening of the inguinal canal, passes through it and is woven into the pubic tissue in the form of separate fibrous bundles. The ovary is attached to the posterior leaf of the broad ligament of the uterus by its mesenteric edge. The section of the broad ligament of the uterus adjacent to the ovary is called the mesentery of the ovary (mesovarium). At the base of the broad ligaments of the uterus between the cervix and the pelvic walls lie bundles of fibrous fibers and smooth muscle cells that form the cardinal ligaments (ligg. cardinalia). With their lower edges, these ligaments are connected to the fascia of the urogenital diaphragm and prevent lateral displacement of the uterus.
Vessels and nerves of the uterus
The blood supply to the uterus is provided by aa. et w. uterinae et ovaricae. Each a. uterinae usually originates from the anterior branch of the internal iliac artery, most often together with the umbilical artery. The beginning of the uterine artery is usually projected onto the lateral edge of the pelvis, at a level of 14-16 cm below the innominate line. Then the uterine artery is directed medially and forward under the peritoneum above the fascia-covered muscle that lifts the anus, to the base of the broad ligament of the uterus, where branches usually originate from it to the urinary bladder (rami vesicales). They participate in the blood supply not only to the corresponding parts of the urinary bladder wall, but also to the area of the vesicouterine fold. Then the uterine artery crosses the ureter, located above it and giving it a small branch, and then comes close to the lateral wall of the uterus, most often at the level of the isthmus. Here a. uterinae gives off a descending, or vaginal (one or more), artery (a. vaginalis). Continuing further upward along the lateral wall of the uterus to its angle, the uterine artery along its entire length gives off from 2 to 14 branches to the anterior and posterior walls of the uterus. In the area of origin of the proper ligament of the ovary, a. uterina sometimes gives off a large branch to the fundus of the uterus (from which the tubal branch often departs) and branches to the round uterine ligament, after which the uterine artery changes its direction from vertical to horizontal and goes to the hilum of the ovary, where it divides into ovarian branches that anastomose with the ovarian artery.
The veins of the uterus have thin walls and form the uterine venous plexus, located mainly in the area of the lateral walls of the cervix and parauterine tissue. It widely anastomoses with the veins of the vagina, external genitalia, vesical and rectal venous plexuses, and the pampiniform plexus of the ovary. The uterine venous plexus collects blood mainly from the uterus, vagina, fallopian tubes, and broad ligament of the uterus. Through the veins of the round ligament, the uterine venous plexus communicates with the veins of the anterior abdominal wall. Blood flows from the uterus through the uterine vein into the internal iliac vein. The uterine veins in their lower sections most often consist of two trunks. It is important to note that of the two uterine veins, one (the smaller one) is usually located in front of the ureter, the other - behind it. Blood from the bottom and upper part of the uterus flows out, in addition, through the veins of the round and broad ligaments of the uterus into the pampiniform plexus of the ovary and further - through v. ovarica into the inferior vena cava (on the right) and renal (on the left); from the lower part of the body of the uterus and the upper part of the cervix, blood flows out directly into v. iliaca interna; from the lower part of the cervix and vagina - into the v. iliaca interna system through the internal vena cava.
The uterus is innervated by the lower hypogastric plexuses (sympathetic) and by the pelvic visceral nerves (parasympathetic).
The lymphatic system of the uterus is conventionally divided into intraorgan and extraorgan, with the former gradually transitioning into the latter.
The lymphatic vessels of the first group, which drain lymph from approximately the upper two thirds of the vagina and the lower third of the uterus (mainly the cervix), are located at the base of the broad ligament of the uterus and flow into the internal iliac, external and common iliac, lumbar sacral and anorectal lymph nodes.
The lymphatic vessels of the second (upper) group drain lymph from the body of the uterus, ovaries and fallopian tubes; they originate mainly from the large subserous lymphatic sinuses and pass mainly in the upper part of the broad ligament of the uterus, heading to the lumbar and sacral lymph nodes, and partly (mainly from the fundus of the uterus) - along the round ligament of the uterus to the inguinal lymph nodes. Regional lymph nodes of the uterus are located in various parts of the pelvic cavity and abdominal cavity: from the iliac arteries (common, external, internal) and their branches to the place where the mesenteric artery departs from the aorta.
X-ray anatomy of the uterus
For X-ray examination of the uterus, a contrast agent is introduced into its cavity (metrosalpingography). On the X-ray, the shadow of the uterine cavity has the form of a triangle with slightly concave sides. The base of the triangle is facing upwards, and the apex is facing downwards. The upper angles of the uterine cavity correspond to the openings of the fallopian tubes, the lower angle corresponds to the internal opening of the cervical canal. The uterine cavity contains from 4 to 6 ml of contrast fluid.

