Medical expert of the article
New publications
Focal epileptic seizures in children and adults
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Focal epilepsy is a type of brain disease known since ancient times, which manifests itself in specific convulsive attacks, called epileptic. For ignorant people in the modern world, contemplation of such attacks brings horror and numbness. Although in ancient times this disease was considered sacred due to the fact that the disease manifested itself in many great people of that time, who were considered saints and prophets.
What is focal epilepsy?
The human nervous system is a complex mechanism whose activity is based on the processes of excitation and inhibition due to irritation of neurons by external or internal factors. In this way, our body reacts to changes occurring inside it or in the surrounding space.
All sensory receptors on the human body, the network of nerve fibers, and the brain are supplied with neurons. It is thanks to these electrically excitable cells that we have the ability to feel, sense, perform purposeful actions and be aware of them.
Excitation is the process of energy transfer by a neuron through the nervous system, which transmits a signal (electrical impulse) to the brain or in the opposite direction (to the periphery). In a healthy person, the process of excitation of neurons occurs under the influence of irritating factors. Epilepsy is said to occur if foci of pathological excitation are detected in the brain, the neurons of which come to a state of combat readiness spontaneously without serious reasons with the formation of an excessively high charge.
Foci of increased excitability of the brain can have different shapes and sizes. Foci can be either single, clearly defined (localized form of the disease), or multiple, scattered across different parts of the brain (generalized form).
Epidemiology
In Ukraine, according to statistics, 1-2 people out of a hundred suffer from epilepsy. More than 70% of cases of epilepsy diagnosis are due to the congenital form of the pathology. This is a striking example of a generalized form of the disease, the causes of which are most likely hidden in a genetic anomaly. Nevertheless, there is a certain percentage of patients who are diagnosed with idiopathic focal epilepsy with a clearly defined focus of excitation in one specific part of the brain.
Causes focal epilepsy
Focal epilepsy is classified as a chronic neurological disease. It can be congenital without any anatomical defects in the brain structure. In this case, only disturbances are observed on the part of neurons that send incorrect signals to the periphery, which results in the appearance of pathological phenomena of various natures.
Symptoms of primary (idiopathic) epilepsy can be observed already in early childhood and adolescence. It responds well to drug therapy and over time the frequency of epileptic seizures decreases.
The processes of excitation in the brain constantly alternate with inhibition of the nervous system, thus, the control structures of the brain give it the opportunity to calm down and rest. If the control is not at the proper level, the brain is forced to constantly be in an excited state. This phenomenon is called increased convulsive readiness, which is characteristic of epilepsy.
The cause of genetic failures can be oxygen starvation at different stages of fetal development, intrauterine infections, intoxication, fetal hypoxia during childbirth. Incorrect genetic information can also be transmitted to subsequent generations that have not been exposed to the above factors.
But the disease can also occur later. This form of pathology is called acquired (secondary, symptomatic), and its symptoms can appear at any age.
The causes of the development of symptomatic focal epilepsy are rooted in organic brain damage caused by:
- traumatic brain injuries (moreover, manifestations of the disease may appear in the coming months after the injury, for example, a concussion, or be delayed in nature, reminding of themselves after several years),
- internal bacterial and viral infections (risk factors in this case are: untimely or incomplete treatment of the disease, ignoring bed rest in the acute stage of the pathology, ignoring the fact of the disease itself),
- previous meningitis or encephalitis (inflammation of the brain structures),
- acute cerebrovascular accidents, resulting in hypoxia of brain tissue, previous ischemic and hemorrhagic strokes,
- cervical osteochondrosis, which can provoke a circulatory disorder in the brain area,
- malignant and benign tumors in the brain, aneurysms,
- arterial hypertension,
- chronic alcoholism (focal epilepsy in alcoholism is caused by toxic damage to the brain and metabolic disorders in its tissues, which is a consequence of regular alcohol abuse).
But various defects (dysgenesis) of the nervous system are more characteristic of idiopathic focal epilepsy.
There is also an intermediate form of the disease called focal epilepsy associated with BEEP (benign epileptiform patterns of childhood). BEEP is diagnosed in 2-4% of children under 14 years of age. Every tenth such child is diagnosed with epilepsy.
Doctors believe that the cause of this form of focal epilepsy is birth trauma, i.e. organic brain damage received by the child during birth. Thus, a doctor's error can cause epileptic seizures in a child without congenital pathologies.
Pathogenesis
The basis of the pathogenesis of focal epilepsy is also uncontrolled spontaneous excitation of neurons in the brain, but in this form of the disease, such a pathological focus has limited dimensions and a clear localization. Thus, focal epilepsy should be understood as a localized form of the disease, the symptoms of which are less pronounced than in generalized seizures, when excitation occurs in different parts of the brain. Accordingly, the frequency of seizures in this case is less.
Many people associate an epileptic seizure with a convulsive attack, although in fact a whole complex of symptoms may be observed that precede unusual seizures. Excessive discharge of neurons in the brain provokes the occurrence of short-term pathological conditions characterized by disturbances in sensitivity, motor activity, mental processes, the appearance of vegetative symptoms and disturbances of consciousness.
The most unusual thing about this pathology is that patients most often cannot remember the details of the attack, since they do not even realize what happened to them. During a simple attack, the patient may remain conscious, but not control their reactions and actions. They realize that they have had an attack, but cannot describe the details. Such an attack usually lasts no more than 1 minute and is not accompanied by serious consequences for a person.
During a complex epileptic seizure, there is a short-term loss or confusion of consciousness. And when a person comes to, he cannot understand what happened to him if he suddenly finds himself in the wrong position or in the wrong place where the seizure caught him. The duration of such a seizure can vary from 1 to 3 minutes, after which the patient may have trouble orienting himself in the area for several more minutes, getting confused in events, spatial and temporal coordinates.
Symptoms focal epilepsy
When speaking about the clinical picture of focal epilepsy, it is important to remember that we are dealing with a small, limited epileptogenic focus in the brain, and depending on the location of this focus, the symptoms of the disease will change. However, a distinctive feature of any type of epilepsy is the presence of recurring epileptic seizures that develop progressively, but end within a short period of time.
As we have already mentioned, simple seizures occur without the patient losing consciousness, while complex seizures are characterized by disturbances and confusion of consciousness. Most often, complex epileptic seizures occur against the background of simple ones, and then a disturbance of consciousness is observed. Sometimes automatisms (multiple monotonous repetitions of words, movements, actions) occur. With secondary generalization, complex seizures occur against the background of a complete loss of consciousness. At first, symptoms of a simple seizure appear, and when excitation spreads to other parts of the cerebral cortex, a tonic-clonic (generalized) seizure occurs, which is stronger than a focal one. In the case of a disturbance or loss of consciousness, the patient feels some inhibition of reactions for another hour, and has poor judgment.
Simple epileptic paroxysms can occur with motor, sensory, autonomic, somatosensory disorders, occur with the appearance of visual and auditory hallucinations, changes in the sense of smell and taste, and even with mental disorders.
But these are all general phrases. What symptoms can manifest individual forms and types of focal epilepsy?
Idiopathic focal epilepsy is characterized by rare seizures with unilateral motor and/or sensory symptoms. Seizures most often begin with speech disorders, numbness of the tongue and mouth tissues, spasms of the pharynx, etc. Patients often experience weakened muscle tone, jerky movements of the body and limbs, impaired coordination of movement and orientation in space, and disruptions in the visual system.
Focal epilepsy in children is in most cases congenital and has symptoms of the idiopathic form. In infants, the disease may manifest itself in the form of trembling eyelids, a glassy, frozen gaze, freezing, throwing back the head, arching the body, spasms. Involuntary defecation and urination are not a reason to diagnose the disease if they are observed in children under 2 years old.
The first signs of an approaching attack in a child may be the following symptoms: the baby's sleep is disturbed, increased irritability appears, he begins to be capricious for no reason. In early childhood, attacks are often accompanied by loss of consciousness, whims, increased tearfulness of the baby.
Older children may experience sudden freezing with no reaction to the surroundings and stimuli, a gaze frozen at one point. With focal epilepsy, visual, gustatory and auditory disturbances often occur. After the seizure, the child continues to do his or her business as if nothing had happened.
Epileptic seizures in children do not necessarily have to be accompanied by convulsions. Seizures without convulsions (also known as absences), lasting less than 30 seconds, are often observed in girls between the ages of 5 and 8.
In adolescence, epileptic seizures are often accompanied by tongue biting and foaming at the mouth. After the seizures, the child may feel sleepy.
The symptomatic form of the disease has a clinical picture corresponding to the localization of the affected area in the brain, since different parts of the brain are responsible for different aspects of our life.
If the zone of increased neuronal excitability is located in the temple area ( temporal epilepsy ), the epileptic seizure has a short duration (half a minute to a minute). The seizure is preceded by a bright aura: the patient may complain of vague pain in the abdomen, semi-real illusions (pareidolia) and hallucinations, impaired sense of smell, spatial-temporal perception, awareness of one's location.
Attacks may occur with either loss of consciousness or preservation of consciousness, but awareness of what is happening remains blurred. Manifestations of the disease will depend on the location of the epileptogenic focus. If it is located in the medial zone, then partial loss of consciousness is observed, i.e. the person may freeze for a while.
After a sharp stop in motor and speech activity, adults experience predominantly motor automatisms. In other words, a person can repeatedly and unconsciously repeat some simple actions or gestures. In children, oral automatisms predominate (pushing of lips, imitation of sucking, clenching of jaws, etc.).
Temporary mental disorders may be observed: a feeling of unreality of what is happening with memory impairment, self-perception disorders, etc.
The lateral location of the lesion in the temporal zone of a person is tormented by nightmarish hallucinations (visual and auditory), increased anxiety, dizziness that is not systemic, temporary loss of consciousness and loss of balance without the appearance of convulsions (temporal syncope).
If the lesion is found in the dominant hemisphere of the brain, speech disorders ( aphasia ) may be observed for some time after the attack.
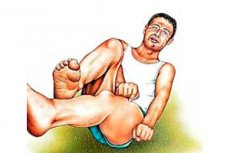
If the disease progresses, at a certain stage secondary generalized seizures may occur, which occurs in 50% of patients with focal temporal epilepsy. In this case, in addition to loss of consciousness, tonic-clonic seizures are observed, with which we usually associate the concept of epilepsy: numbness of the limbs in an extended state, throwing back the head, a loud violent scream (sometimes as if growling) with an active exhalation, then twitching of the limbs and body, spontaneous release of urine and feces, the patient may bite the tongue. At the end of the attack, speech and neurological disorders are observed.
At later stages of the disease, the patient's personality characteristics may change, and he or she may become more conflicted and irritable. Over time, thinking and memory are impaired, and slowness and a tendency to generalize appear.
Focal temporal lobe epilepsy is one of the most common types of symptomatic form of the disease, which is diagnosed in every fourth patient.
For focal frontal epilepsy, which is rightfully considered the most popular type of pathology, the appearance of an aura is not typical. The attack usually occurs against the background of preserved consciousness or in sleep, has a short duration, but tends to be serial (repeated attacks).
If an epileptic seizure begins during the daytime, one may notice uncontrolled movements of the eyes and head, the appearance of complex motor automatisms (the person begins to move their arms and legs, imitating walking, running, riding a bicycle, etc.) and psycho-emotional disorders (aggression, nervous excitement, throwing, shouting, etc.).
If the epileptogenic focus is located in the precentral gyrus, sudden motor disturbances of a tonic-clonic nature may occur, localized on one side of the body, usually occurring against the background of preserved consciousness, although sometimes the seizure generalizes. At first, the person freezes for a moment, and then almost immediately muscle twitching is noted. They always begin in the same place and spread to the half of the body where the seizure began.
The spread of convulsions can be prevented by clamping the limb where they began. However, the initial focus of the attack can be located not only on the limbs, but also on the face or body.
If seizures occur in a person during sleep, then such short-term disorders as sleepwalking, parasomnias (movement of limbs and involuntary muscle contractions in a sleeping person), and nocturnal enuresis may occur. This is a fairly mild form of the disease, in which increased excitability of neurons is observed in a limited area and does not spread to other areas.
Focal occipital epilepsy manifests itself mainly in visual disturbances. These can be involuntary eye movements as well as visual disturbances: its deterioration, temporary blindness, the appearance of visual hallucinations and illusions of various nature and complexity, narrowing of the visual field, formation of slopes (empty areas in the visual field), the appearance of flashing lights, flashes, patterns before the eyes.
As for visual motor disorders, here one may observe trembling of the eyelids, rapid oscillatory movements of the eyes up and down or from side to side (nystagmus), sharp narrowing of the pupils of the eyes (miosis), rolling of the eyeball, etc.
Most often, such an attack is observed against the background of a migraine-like headache, pale skin. In children and some adults, they can be accompanied by attacks of abdominal pain and vomiting. The duration of the attack can be quite long (10-13 minutes).
Focal epilepsy of the parietal zone is the rarest type of symptomatic form of the disease, usually caused by tumor and dysplastic processes in the brain. Patients complain of impaired sensitivity with characteristic symptoms: tingling, burning, acute short-term pain in the area of numbness. A person may feel that the numb limb is absent altogether or is in an uncomfortable position, dizziness and confusion may occur.
Most often, loss of sensitivity occurs in the face and hands. If the epileptogenic focus is located in the paracentral gyrus, numbness can also be felt in the groin, thighs, and buttocks. If the postcentral gyrus is affected, symptoms appear in a limited area and gradually spread to other areas.
If the posterior parietal zone is affected, then it is quite possible that visual hallucinations and illusory images will appear, as well as a disturbance in the visual assessment of the size of objects, the distance to them, etc.
When the parietal zone of the dominant hemisphere of the brain is damaged, speech and mental arithmetic disorders occur. Spatial orientation disorders are observed when the lesion is localized in the non-dominant hemisphere.
Attacks occur mainly during the day and last no more than 2 minutes. But their frequency of occurrence may be higher than in other localizations of the pathological focus.
Cryptogenic focal epilepsy of unclear genesis can occur against the background of alcoholism and drug addiction, and also be a consequence of head poisoning, viral pathologies, liver and kidney disorders. Usually, with epilepsy, seizures occur spontaneously, but with this form of pathology, they can be provoked by bright light, loud sounds, sudden temperature changes, sudden awakening, an event that caused a surge of emotions, etc.
It is believed that the disease is accompanied by a metabolic disorder. The fat content in the body remains at the same level, but the water level constantly increases and it begins to accumulate in tissues, including brain tissue, which provokes the onset of an attack.
Quite often, attacks of varying duration occur with loss of consciousness and neurological disorders. Their regular repetition can lead to mental disorders.
The harbingers of a severe and prolonged attack are considered to be: the appearance of insomnia, tachycardia, headaches, bright visual hallucinations with flashing lights.
Focal epilepsy with secondary generalization of seizures is characterized by the following manifestations:
- First, an aura occurs within a few seconds, the symptoms of which are unique, i.e. different people may experience different symptoms indicating the onset of a seizure,
- Then the person loses consciousness and balance, muscle tone decreases and he falls to the floor, making a specific cry caused by the difficult passage of air through the suddenly narrowed glottis with a sudden contraction of the chest muscles. Sometimes the muscle tone does not change and the fall does not occur.
- Now comes the phase of tonic convulsions, when the person's body freezes for 15-20 seconds in an unnatural pose with outstretched limbs and a head thrown back or turned to the side (it turns to the side opposite the lesion). Breathing stops for a while, the veins in the neck swell, the face becomes pale, which can gradually take on a bluish tint, and the jaws are tightly clenched.
- After the tonic phase, the clonic phase begins, lasting about 2-3 minutes. During this phase, twitching of muscles and limbs, rhythmic flexion and extension of arms and legs, oscillatory movements of the head, movements of the jaws and lips are observed. These same paroxysms are characteristic of a simple or complex attack.
Gradually, the strength and frequency of convulsions decrease, and the muscles relax completely. In the post-epileptic period, there may be a lack of response to stimuli, dilation of the pupils, lack of eye reaction to light, tendon and protective reactions.
Now some information for alcohol lovers. Cases of focal epilepsy development against the background of alcohol abuse are not uncommon. Usually seizures are caused by head injuries, which often happen in a state of alcohol intoxication, withdrawal syndrome, and sudden alcohol withdrawal.
Symptoms of alcoholic epilepsy include: fainting and loss of consciousness, cramps, burning pain, a feeling of squeezing or twisting of muscles in the limbs, hallucinations, vomiting. In some cases, a burning sensation in the muscles, hallucinations, and delirious states are observed even the next day. After attacks, sleep disorders may occur, irritability and aggression arise.
Further exposure of the brain to alcohol toxins leads to increased frequency of seizures and personality degradation.
Forms
Focal epilepsy is a generalized name for diseases with a clearly defined zone of excessive excitation of neurons, characterized by recurring epileptic seizures. Since this is a disease of the neurological sphere, specialists in this field distinguish 3 forms of focal epilepsy: idiopathic, symptomatic and cryptogenic.
Idiopathic focal epilepsy, which we have already mentioned, is a type of disease, the causes of which have not been fully studied. But scientists assume that everything comes down to disturbances in the maturation of the brain in the prenatal period, which have a genetic nature. At the same time, devices for instrumental diagnostics of the brain (MRI and EEG devices) do not show any changes.
The idiopathic form of the disease is also called benign focal epilepsy. This is the form that is referred to when a doctor makes a diagnosis:
- benign childhood (rolandic) epilepsy or epilepsy with central-temporal peaks,
- benign occipital epilepsy with early manifestations (Panayotopoulos syndrome, occurs before the age of 5 years),
- benign occipital epilepsy, which manifests itself at a later age (Gastaut-type epilepsy is diagnosed in children over 7 years old),
- primary epilepsy of reading (the rarest type of pathology with the localization of the epileptogenic focus in the parietal-temporal zone of the cerebral hemisphere, which is largely responsible for speech, is more common in the male population with alphabetic writing),
- autosomal dominant frontal lobe epilepsy with nocturnal paroxysms,
- familial temporal lobe epilepsy
- non-familial and familial benign epileptic seizures in infancy,
- familial temporal lobe epilepsy, etc.
Symptomatic focal epilepsy, on the contrary, has specific causes, consisting of all sorts of organic lesions of the brain and revealed during instrumental studies in the form of interconnected zones:
- zone of anatomical damage (direct focus of brain damage resulting from head injury, circulatory disorders, inflammatory processes, etc.),
- zone of formation of pathological impulses (area of localization of neurons with high excitability),
- symptomatic zone (area of excitation distribution, which determines the clinical picture of an epileptic seizure),
- irritant zone (a part of the brain in which increased electrical activity is detected by EEG outside of seizures),
- zone of functional deficit (the behavior of neurons in this area provokes neurological and neuropsychiatric disorders).
The symptomatic form of the disease includes:
- Permanent partial epilepsy (synonyms: cortical, continual, Kovzhevnikov epilepsy), characterized by constant twitching of the muscles of the upper body (mainly on the face and arms).
- Epileptic syndromes provoked by certain factors, for example, attacks of partial (focal) epilepsy that occur upon abrupt awakening or under the influence of strong psychoemotional factors.
- Focal temporal epilepsy, in which the temporal zone of the brain is affected, responsible for thinking, logic, hearing, behavior. Depending on the localization of the epipathological focus and the symptoms that appear, the disease can occur in the following forms:
- amygdala,
- hippocampal,
- lateral (posterior temporal),
- insular.
If both temporal lobes are affected, we can talk about bilateral (bitemporal) temporal epilepsy.
- Focal frontal epilepsy, which is characterized by damage to the frontal lobes of the brain with speech impairments and serious behavioral disorders (Jacksonian epilepsy, sleep epilepsy).
- Focal parietal epilepsy, characterized by decreased sensitivity on one half of the body.
- Focal occipital epilepsy, which occurs at different ages and is characterized by visual impairment. There may also be problems with coordination of movement and increased fatigue. Sometimes the process spreads to the frontal lobes, making diagnosis difficult.
A special type of the disease is multifocal epilepsy, when mirror-like epileptogenic foci are successively formed in opposite hemispheres of the brain. The first focus usually appears in infancy and affects the electrical excitability of neurons in the symmetrical area of the other hemisphere of the brain. The appearance of the second focus leads to disturbances in psychomotor development, the work and structure of internal organs and systems.
Sometimes, with obvious symptoms of epilepsy in adults, doctors are unable to establish the cause of the disease. Diagnostics do not reveal organic damage to the brain, but the symptoms indicate otherwise. In this case, the diagnosis is "cryptogenic focal epilepsy", i.e. epilepsy that occurs in a latent form.
Cryptogenic and symptomatic focal epilepsy may occur with secondary generalization, when both cerebral hemispheres are involved in the process. In this case, along with focal (partial) seizures, generalized complex seizures occur, which are characterized by complete loss of consciousness and the presence of vegetative manifestations. In this case, the presence of seizures is not necessary.
Some syndromes may occur with two types of seizures (focal and generalized):
- neonatal seizures in infants,
- severe myoclonic epilepsy developing in early childhood,
- sleep epilepsy, which occurs during the slow-wave sleep phase and is characterized by prolonged complexes of peaks and waves,
- Landau-Kleffner syndrome or secondary epileptic aphasia, which develops at the age of 3-7 years and is characterized by symptoms of aphasia (receptive speech disorder) and speech expressiveness disorders (speech underdevelopment), EEG reveals epileptic paroxysms, and the patient also experiences simple and complex epileptic seizures (in 7 out of 10 patients).
Complications and consequences
Despite the fact that focal epilepsy is considered a milder form of the disease than generalized, its symptoms not only look very unsightly, but also pose a certain danger to the patient. Of course, seizures do not occur as often and are less pronounced than in generalized ones, but even these infrequent seizures pose a high risk of injury with a sudden decrease in tone and falling to the floor, especially if there is no person nearby who can support in such a situation.
Another big danger is the high probability of asphyxia due to vomit entering the respiratory tract or blocking the air flow with the patient's tongue falling inside. This can happen if there is no person nearby to turn the patient's body on its side during the attack. Asphyxia in turn can lead to the death of the patient, regardless of the cause and type of epilepsy.
Vomiting into the respiratory tract during an attack can provoke the development of an acute inflammatory process in the lung tissue ( aspiration pneumonia ). If this happens regularly, the disease can have a complicated course, the mortality rate of which is about 20-22 percent.
In frontal focal epilepsy, paroxysms may occur serially over half an hour with a short interval between attacks. This condition is called epileptic status. The occurrence of serial seizures may also be a complication of other types of epilepsy.
The human body simply does not have time to recover during the intervals. If there is a delay in breathing, this can lead to hypoxia of the brain and related complications (with a total duration of attacks of more than half an hour, oligophrenia, mental retardation in children, death of the patient with a probability of 5-50%, behavioral disorders may develop). Convulsive epileptic status is especially dangerous.
If the disease is not treated, many patients develop mental instability. They are prone to outbursts of irritability, aggression, and they begin to conflict in a group. This affects a person's relationships with other people, creates obstacles in work and everyday life. In some cases, an advanced disease leads not only to emotional instability, but also to serious mental disorders.
Focal epilepsy is especially dangerous in children, since regular attacks can lead to delays in mental development, speech and behavioral disorders, which presents certain difficulties during learning and communication with peers, teachers, parents, and a decrease in academic performance at school.
Diagnostics focal epilepsy
Doctors diagnose focal epilepsy based on periodically recurring epileptic seizures. Single paroxysms are not considered a reason to suspect a serious illness. However, even such seizures are sufficient grounds for contacting a doctor, whose task is to identify the disease at an early stage of its development and prevent the progression of symptoms.
Even a single focal paroxysm may be a symptom of a severe cerebral disease, such as tumor processes in the brain, vascular malformation, dysplasia of the cortical zone, etc. And the earlier the disease is detected, the greater the chances of defeating it.
This problem should be addressed to a neurologist who will conduct a physical examination of the patient, listen carefully to the patient's complaints, paying attention to the nature of the symptoms, the frequency of their recurrence, the duration of the attack or attacks, the symptoms preceding the seizure. The sequence of the development of an epileptic seizure is very important.
It is important to understand that the patient himself often remembers little about the symptoms of the attack (especially a generalized one), so the help of relatives or eyewitnesses to the attack may be needed, who can provide details.
It is mandatory to study the patient's medical history and family history to identify episodes of epilepsy in the patient's family. The doctor will definitely ask the patient (or his relatives, if it is a small child), at what age the seizures or symptoms corresponding to absences appeared, as well as the events preceding the attack (this will help to understand what provoked the excitation of the brain neurons).
Laboratory tests in case of focal epilepsy are not important diagnostic criteria. General urine and blood tests, which the doctor may prescribe in this case, are needed rather to identify concomitant pathologies and determine the functionality of various organs, which is important for prescribing drug treatment and physical therapy.
But without instrumental diagnostics, an accurate diagnosis is impossible, because based on the above, the doctor can only guess in which area of the brain the epileptogenic focus is located. The most informative from the point of view of diagnosing epilepsy are:
- EEG (electroencephalogram). This simple test sometimes allows us to detect increased electrical activity in epi-foci even between attacks, when a person goes to the doctor (in the transcript it is shown as sharp peaks or waves of greater amplitude than the rest)
If the EEG does not show anything suspicious during the interictal period, provocative and other studies are carried out:
- EEG with hyperventilation (the patient needs to breathe quickly and deeply for 3 minutes, after which an increase in the electrical activity of neurons is observed,
- EEG with photostimulation (using flashes of light),
- Sleep deprivation (stimulation of neuronal activity by denying sleep for 1-2 days),
- EEG at the time of the attack,
- Subdural corticography (a method that allows determining the exact localization of the epileptogenic focus)
- MRI of the brain. The study allows to identify the causes of symptomatic epilepsy. The thickness of the slices in this case is minimal (1-2 mm). If structural and organic changes are not detected, the doctor makes a diagnosis of cryptogenic or idiopathic epilepsy based on the patient's history and complaints.
- Positron emission tomography (PET of the brain). It is used less often, but helps to identify metabolic disorders in the tissues of the epi-focus.
- X-ray of the skull. It is performed in case of injuries or impossibility of performing other examinations.
Additionally, a biochemical blood test, blood test for sugar and infections, tissue biopsy and subsequent histoscopic examination (if there is a suspicion of an oncological process) may be prescribed.
Differential diagnosis
Differential diagnostics helps to determine the form of the disease (focal or generalized), make an accurate diagnosis taking into account the localization of the lesion, differentiate between isolated epileptic seizures provoked by emotional states and epilepsy itself, as a chronic disease with recurring seizures.
Who to contact?
Treatment focal epilepsy
Treatment for the patient can be prescribed by a neurologist or epileptologist, if such a specialist is available at the medical institution. The basis of therapy for focal epilepsy is taking medications, while physiotherapy for this pathology is not prescribed at all, so as not to provoke an attack, or is carried out with special caution (usually these are special exercise therapy exercises that help balance the processes of excitation and inhibition in the brain). It is necessary to immediately adjust to the fact that taking medications will not be temporary, but constant throughout the patient's life.
The main antiepileptic drugs are considered to be anticonvulsants: "Carmazepine", "Clobazam", "Lacosamide", " Lamotrigine ", "Phenobarbital", valproic acid preparations, etc. The drugs are selected individually and, if there is no good effect, are replaced by others. The goal of such treatment is a significant reduction in the number of attacks and relief of symptoms.
If focal epilepsy is caused by other diseases, then in addition to stopping epileptic seizures, it is necessary to treat the underlying disease, otherwise the result will be insufficient.
Among the symptomatic types of epilepsy, the occipital and parietal forms respond well to drug treatment. But with temporal localization of the epileptic focus, resistance to the action of antiepileptic drugs may develop after a couple of years. In this case, surgical treatment is recommended.
Indications for surgical treatment may include deterioration of the patient's condition, an increase in the number and duration of attacks, a decrease in intellectual abilities, etc. Neurosurgeons perform brain surgery by removing either the epileptogenic focus itself or neoplasms (tumors, cysts, etc.) that provoke pathological excitability of neurons (focal or extended resection with removal of adjacent tissues where epiactivity extends). Such operations are possible only if the localization of the epileptogenic focus is clearly defined as a result of diagnostic studies (corticography).
The environment plays a major role in the successful treatment of epilepsy. The patient should never feel inferior or feel condemned or pitied by others. Attacks occur periodically and rarely affect a person's ability to communicate and learn. The child and adult should lead a full life. They are not prohibited from physical activity (there may only be some restrictions that prevent attacks).
The only thing that is recommended is to protect the patient from strong emotional shocks and heavy physical exertion.
Medicines for focal epilepsy
Since treatment of focal epilepsy attacks is impossible without the use of anticonvulsants, we will talk about them now.
"Karmazepine" is a popular anticonvulsant drug used to treat epilepsy, idiopathic neuralgia, acute manic states, affective disorders, alcohol withdrawal, diabetic neuropathies, etc. The drug is named after its active substance, which is a derivative of dibenzazepine and has normotonic, antimanic and antidiuretic effects. In the treatment of epilepsy, the anticonvulsant effect of the drug, which is available in the form of tablets and syrup, is valued. It can be used to treat children.
In case of monotherapy with the drug for children under 4 years of age, the dose is calculated based on the formula 20-60 mg per kilogram of weight per day, depending on the severity of symptoms. Every two days, the dose should be increased by 20-60 mg. The initial daily dose for children over 4 years of age will be 100 mg. Subsequently, it will have to be increased by 100 ml every week.
Children aged 4-5 years are prescribed 200-400 mg per day (if tablets are needed), children aged 5 to 10 years should take 400-600 mg per day. Teenagers are prescribed from 600 mg to 1 g of the drug. The daily dose should be divided into 2-3 doses.
Adults are prescribed the drug in a dosage of 100-200 mg once or twice a day. The dose is gradually increased to 1.2 g per day (maximum 2 g). The optimal dosage is determined by the attending physician.
The drug is not prescribed in case of hypersensitivity to its components, disorders of bone hematopoiesis, acute porphyria revealed during the study of the anamnesis. It is dangerous to prescribe the drug in case of AV block of the heart and parallel use of MAO inhibitors.
Caution should be exercised when prescribing the drug to patients with heart failure, hyponatremia, liver and kidney dysfunction, dysplastic processes in the prostate gland, increased intraocular pressure. This also includes elderly people and those who suffer from alcoholism.
Taking the drug may cause dizziness, drowsiness, ataxia, asthenic conditions, headaches, accommodation disorders, allergic reactions. Less common are hallucinations, anxiety, and loss of appetite.
"Phenobarbital" is a drug with a hypnotic effect, also used in anticonvulsant therapy for epilepsy to stop generalized and focal seizures in patients of different ages.
The dosage of the drug is determined individually by monitoring blood tests. The minimum effective dosage is prescribed.
Children are prescribed the medicine at a rate of 3-4 mg of the active substance per kilogram of weight, taking into account the increased metabolic rate in children and adolescents. For adults, the dosage is adjusted - 1-3 mg per kg of body weight, but not more than 500 mg per day. The medicine is taken 1 to 3 times a day.
The dosage may be lower when treating older people or patients with impaired renal function.
The drug is not prescribed in case of hypersensitivity to its components, porphyria, respiratory depression, severe liver and kidney pathologies, acute poisoning, including alcohol intoxication, during pregnancy and lactation. Prescribed to patients over 6 years of age.
Taking the medicine may be accompanied by dizziness, impaired coordination of movements, headaches, hand tremors, nausea, bowel and vision problems, decreased blood pressure, allergic and other reactions.
"Convulex" is a drug based on valproic acid, which is classified as an antiepileptic drug, since it has an anticonvulsant effect in various types and forms of epilepsy, as well as in febrile seizures in children not associated with the disease. It is available in the form of syrup, tablets, drops for oral administration and injection solution.
The dosage of the drug is determined depending on the age and body weight of the patient (from 150 to 2500 mg per day) with dose adjustment in elderly patients and those with kidney pathologies.
The drug should not be prescribed in case of hypersensitivity to its components, hepatitis, liver and pancreas dysfunction, porphyria, hemorrhagic diathesis, obvious thrombocytopenia, urea metabolism disorders, during breastfeeding. Do not use simultaneously with mefloquine, lamotrigine and St. John's wort preparations.
Caution should be exercised when treating with several drugs, during pregnancy, with organic brain damage, at the age of up to 3 years. It is advisable to abstain from pregnancy, since there is a risk of giving birth to children with CNS pathologies.
Like the previous drugs, "Convulex" is well tolerated by patients. But the following side effects are also possible: nausea, abdominal pain, appetite and stool disorders, dizziness, hand tremors, ataxia, visual impairment, changes in blood composition, changes in body weight, allergic reactions. Usually, such symptoms are observed if the level of the active substance in the blood plasma exceeds 100 mg per liter or therapy is carried out simultaneously with several drugs.
"Klobazam" is a tranquilizer with sedative and anticonvulsant action, prescribed as part of complex therapy for epilepsy. It is used to treat patients over 3 years of age.
Adults are prescribed the drug in tablet form in a daily dosage of 20 to 60 mg. The medicine can be taken once (at night) or twice a day. Elderly patients require a dose adjustment (no more than 20 mg per day). The pediatric dose is 2 times less than the adult dose and is determined by the doctor depending on the patient's condition and the medications taken.
The drug is not prescribed in case of hypersensitivity to the drug, respiratory disorders (depression of the respiratory center), serious liver pathologies, acute poisoning, in the 1st trimester of pregnancy, drug dependence (detected by studying the anamnesis). Do not prescribe to children under 6 months.
Caution should be exercised in cases of myasthenia, ataxia, bronchial asthma, liver and kidney pathologies.
During the drug intake, patients may feel tired, sleepy, dizzy, have tremors in the fingers, feel sick, and suffer from constipation. Sometimes allergic reactions occur. There is a possibility of bronchospasm. Severe reversible dysfunctions of various organs are possible with prolonged intake of large doses of the drug.
Along with anticonvulsants, you can take vitamins, phytonutrients, antioxidants - drugs that improve brain function and help increase the effectiveness of special treatment. Omega-3 fatty acids also reduce the number of attacks. But an epileptic can take any medications only after consulting a doctor.
Folk remedies
It should be said that folk medicine also succeeds in treating focal epilepsy, which is considered a milder form of the disease. Folk treatment not only does not interfere with drug therapy, but even enhances its effect and reduces the number of epileptic seizures. In this case, you can use recipes from various gifts of nature and herbal treatment together.
For example, apricot kernels can be used to treat epilepsy in children. You need to choose non-bitter specimens, peel them and give them to the child in an amount corresponding to the number of full years of the child's life. It is recommended to use the kernels in the morning before meals. Continue the treatment for a month, after which you need to take a break of the same duration, observing whether the attacks recur. If necessary, repeat the course of treatment.
If a patient suffers from night attacks, you can buy myrrh in a church and fumigate the room with it before going to bed for at least a month and a half. This helps the patient calm down and relax.
You can also take an infusion of valerian root three times a day, which must be crushed beforehand. Pour 1 tbsp of plant material into 200-250 ml of cool water and leave for 8 hours. Adults are recommended to take 1 tbsp of infusion, children - 1 tsp.
Herbal baths are recommended for epileptics. To fill them, you can prepare an infusion of forest hay or a composition of pine buds, aspen and willow branches, calamus roots (pour boiling water over the crushed raw materials and let it brew). The bath should be taken for no more than 20 minutes. The water temperature should not exceed 40 degrees.
For any type of epilepsy, it is useful to add dried herbs such as mint, thyme, hops (cones), sweet clover, lovage, and marigolds (flowers) to the pillow filling. The patient should sleep on such a pillow every night.
In case of alcoholic epilepsy, it is useful to take angelica powder (0.5 g) purchased at a pharmacy three times a day and drink coffee made from peeled grains of rye, barley, oats, acorns with the addition of dandelion roots and chicory. All components are poured with boiling water and infused.
To treat symptomatic focal epilepsy, in addition to the main treatment, you can try to stop the attacks using the following recipe: take 3 tablespoons of good black tea, dried chamomile flowers and dried wormwood, brew 1 liter of boiling water and leave for at least 4 hours. The prepared infusion should be drunk during the day after straining. Three monthly courses are required with an interval of 1 month between them.
Stone oil, which contains a huge amount of substances useful for the human body, also helps in treating the disease. It is recommended to dilute 3 g of stone oil in 2 liters of water and take this medicine for a month three times a day before meals. A single dose is 1 glass. The treatment should be carried out regularly once a year.
An alcohol tincture of peony petals is also suitable for treating epilepsy. For 0.5 liters of good vodka, take three tablespoons of plant material. The medicine is infused for 3-4 weeks. It should be taken three times a day, 1 teaspoon at a time.
When using various folk remedies, one should not forget about drug treatment. There are reports on the Internet that many people were helped to refuse drug treatment by using the Doman oxygen mask. This treatment option can also be considered, but if it does not bring the desired improvement, it is better to return to traditional treatment, supported by folk recipes.
 [ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ], [ 39 ], [ 40 ], [ 41 ]
[ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ], [ 39 ], [ 40 ], [ 41 ]
Homeopathy
Probably, adherents of folk medicine will have it easier than fans of homeopathy. The fact is that in our country few homeopaths undertake to treat patients diagnosed with generalized or focal epilepsy. And there are not so many drugs that help with this pathology.
To improve the condition and functioning of the brain, you can take the homeopathic drug Cerebrum compositum. But such treatment alone will not help get rid of attacks of the disease.
Epileptic seizures at night and during menstruation, as well as seizures that are aggravated by warmth, are part of the pathogenesis of the homeopathic remedy Bufa rana, made from toad venom.
Nux vomica can be used to treat nighttime seizures. Cuprum also has a beneficial effect on the nervous system, so it is also used to treat epilepsy accompanied by seizures preceded by screaming.
When using homeopathic medicines (and they should be prescribed by a homeopathic doctor) to treat epilepsy, you need to understand the principle of their action. Taking medicines initially worsens the condition of patients. BUT this is a temporary situation, followed by a decrease in the number of attacks and a decrease in their intensity.
Prevention
As for disease prevention, everything depends on the form of the disease. Timely treatment of the underlying disease causing attacks, proper nutrition, and a healthy and active lifestyle will help prevent the symptomatic form of the disease.
To prevent the idiopathic form of the disease in a child, the expectant mother should give up smoking, drinking alcohol and taking drugs during pregnancy and before conception. This does not give a 100% guarantee that the child will not develop such a deviation, but it will reduce the likelihood of such an outcome. It is also recommended to provide the baby with adequate nutrition and rest, protect the head from overheating and injury, promptly contact a pediatrician if any unusual symptoms appear and not panic if a seizure occurs, which does not always indicate the disease.
Forecast
The prognosis of such a disease as focal epilepsy depends entirely on the localization of the affected area and the etiology of the disease. Idiopathic forms of the disease are easily corrected with medication and do not cause difficulties in treatment. Intellectual and behavioral disorders are not observed in this case. In adolescence, attacks may simply disappear.
With appropriate treatment, attacks gradually come to zero in half of the patients, and another 35% note that the number of paroxysms has noticeably decreased. Serious mental disorders are observed in only 10% of patients, while 70% of patients have no intellectual disabilities. Surgical treatment guarantees almost 100% relief from attacks in the near future or in the distant future.
In symptomatic epilepsy, the prognosis depends on the pathology that causes the seizures. Frontal epilepsy, which has a milder course, is the easiest to treat. The prognosis for treating alcoholic epilepsy strongly depends on whether the person can give up drinking alcohol.
In general, treatment of any form of epilepsy requires abstinence from drinks that stimulate the nervous system (alcohol and caffeine-containing liquids), drinking large amounts of clean water and protein-rich foods: nuts, chicken, fish, vitamin products and dishes with a high content of polyunsaturated fatty acids. It is also undesirable for epileptics to work the night shift.
An established diagnosis of focal or generalized epilepsy entitles the patient to receive disability. Any epileptic with moderate-intensity seizures can apply for Group 3 disability, which does not limit his ability to work. If a person experiences simple and complex seizures with loss of consciousness (in pathology with secondary generalization) and decreased mental abilities, he can even be given Group 2, because employment opportunities in this case are limited.
Focal epilepsy is a milder disease than the generalized form of the disease, but nevertheless, epileptic seizures can somewhat reduce the patient's quality of life. The need to take medications, seizures that pose a risk of injury, possible complications and suspicious looks (and sometimes stupid, tactless questions) from people around who have witnessed the seizure can affect the patient's attitude towards themselves and life in general. Therefore, much depends on the relatives and friends of the epileptic, who can increase the person's self-confidence and motivate them to fight the disease. A person should not perceive the disease as a death sentence. It is rather a feature of a person and a test of his will and desire to live a healthy, fulfilling life.

