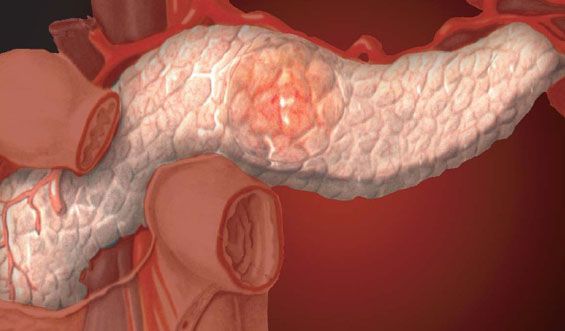
Chronic pancreatitis
Last reviewed: 17.06.2018

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Chronic pancreatitis is a persistent inflammation of the pancreas, which leads to permanent structural damage with fibrosis and stricture of the duct, accompanied by a decrease in exocrine and endocrine functions. The disease of chronic pancreatitis can be caused by chronic alcohol abuse, but it can also be idiopathic.
Read also: Acute pancreatitis in adults
The initial symptoms of chronic pancreatitis are manifested by relapsing bouts of pain. Later, some patients developed intolerance to glucose and malabsorption. The diagnosis is usually established with instrumental examination - ERCPG, echosonography and studies of the secretory function of the pancreas. Treatment of chronic pancreatitis is symptomatic and includes a corresponding diet, analgesics and the use of enzymes. In some cases, surgical treatment is indicated.
ICD-10 code
- K86.0 Chronic pancreatitis of alcoholic etiology
- K86.1 Other chronic pancreatitis.
What causes chronic pancreatitis?
In the US, 70-80% of cases are caused by alcoholism and 15-25% are idiopathic. Rare causes of chronic pancreatitis include hereditary pancreatitis, hyperparathyroidism and obstruction of the common pancreatic duct caused by stenosis, stones or cancer. In India, Indonesia and Nigeria, idiopathic calcific pancreatitis is observed among children and young people ("tropical pancreatitis").
Similarly to acute pancreatitis, the mechanism of the development of the disease may be associated with obstruction of the duct by protein stoppers. Protein plugs may be the result of an excess of glycoprotein-2 secretion or a deficiency of lithostatin, a protein of pancreatic juice that inhibits Ca precipitation. If the obstruction is chronic, persistent inflammation leads to fibrosis, dilatation and fragmentary strictures of the duct, followed by calcification. Neuronal envelope hypertrophy and perineuronal inflammation develop, which can contribute to the development of chronic pain. After several years, progressive fibrosis leads to loss of exocrine and endocrine functions. Diabetes develops in 20-30% of patients within 10-15 years after the onset of the disease.
Symptoms of Chronic Pancreatitis
Most patients experience episodic abdominal pain. Approximately 10-15% of the pain in the left side is absent and malabsorption develops. The pain is severe, localized in the epigastrium and can last several hours or days. Episodes of pain usually disappear spontaneously in 6-10 years due to the progressive destruction of acinar cells secreting pancreatic digestive enzymes. When the secretion of lipases and proteases decreases to less than 10% of the norm, the patient develops steatorrhea, manifested by a fat stool or even with fatty drops and creator. At this time, there may be signs of glucose intolerance.
What's bothering you?
Diagnosis of chronic pancreatitis
The diagnosis may be difficult because the levels of amylase and lipase are often within normal limits because of a significant decrease in pancreatic function. In patients with a typical anamnesis of alcohol abuse and recurrent episodes of acute pancreatitis, the detection of pancreatic calcification in routine abdominal radiography may be sufficient for diagnosis. However, such calcification usually occurs late during the course of the disease and these signs are only detected in about 30% of cases. Patients without a typical anamnesis should be excluded from the pancreatic malignancy as a cause of pain: CT of the abdominal cavity is recommended . CT can visualize calcification and other changes in the gland (eg, pseudocyst or dilated ducts), but in the early stages of the disease these symptoms may be absent.
The initial stages of the examination of patients with normal CT data include ERCP, endoscopic echosonography and studies of the secretory function of the pancreas. These tests are very sensitive, but ERCP can cause acute pancreatitis in approximately 5% of patients. MP cholangiopancreatography (MRCP) may be an acceptable alternative.
In the late stages of the course of the disease, the parameters of exocrine pancreatic function become changed. The study of stools on fat for 72 hours allows you to diagnose steatori, but the study is not specific. The secretin test involves taking a pancreatic secretion through the duodenal probe for analysis, but it is performed only in several centers. The levels of serum trypsinogen and chymotrypsin and elastase in the stool can be reduced. In tests with bentiromide and pancreolauril, substances are taken orally and urine is analyzed for the breakdown products caused by pancreatic enzymes. But all these exocrine tests are less sensitive than ERCPH or endoscopic ultrasonography in the early diagnosis of the disease.
What do need to examine?
How to examine?
Who to contact?
Treatment of chronic pancreatitis
Relapse of the disease requires treatment similar to acute pancreatitis, including hunger, intravenous fluid transfusion and analgesics. After resumption of nutrition, the patient should exclude alcohol and consume only low-fat food (<25 g / day) (to reduce the secretion of pancreatic enzymes). H 2 -blockers or inhibitors of proton pump can reduce the acid-stimulated secretion secretion, and thus reduce pancreatic secretion. However, often these measures do not allow to reduce the pain, which requires an increase in the dose of opiates with the threat of addiction. Treatment of chronic pancreatic pain is often unsatisfactory.
Oral administration of pancreatic enzymes can reduce chronic pain by inhibiting the output of cholecystokinin and thus reducing the secretion of pancreatic enzymes. This approach is likely to be more successful in the case of moderate idiopathic pancreatitis than with alcoholic pancreatitis. Enzymes are also used to treat steatorrhea. Different drugs are effective and a dose providing at least 30 000 units of lipase should be used. Tablets covered with an acid-resistant coating should be used, and they should be taken with food. It is necessary to appoint H2-blockers or proton pump inhibitors to prevent acid destruction of enzymes.
A favorable clinical effect includes weight gain, reduction in stool frequency, disappearance or decrease in steatorrhea, and improvement in general condition. The clinical effect of the treatment can be documented by studies indicating a decrease in fat content in the stool after enzyme therapy. If, despite the treatment of chronic pancreatitis, severe steatorrhea persists, the fat source can provide medium chain triglycerides (they are absorbed without pancreatic enzymes), decreasing proportionally the other edible fats. In addition to treatment, fat-soluble vitamins (A, D, K), including vitamin E, should be prescribed, which helps to reduce inflammation.
Surgical treatment of chronic pancreatitis can be effective in pain. The pseudocyst of the pancreas that causes chronic pain can be drained to the neighboring organ to which it belongs (eg, the stomach), or to the disconnected loop of the jejunum (by cystojunostomy along Roux). If the main pancreatic duct is enlarged by more than 5-8 mm, approximately 70-80% of patients have effective lateral pancreaticunostomy (Operation Puestowe). If the duct is not enlarged, partial resection is effective; Distal pancreatectomy is also used (with significant pancreatic tail damage) or Whipple's operation (if the pancreatic head is affected). Surgical interventions should be used in patients who have refused to drink alcohol, and in those who are able to control secondary diabetes, the development of which can be associated with resection of the pancreas.
Some pseudocysts can be drained endoscopically. Endoscopically, under the control of ultrasound, it is possible to perform a denervation of the solar plexus with alcohol and bupivacaine and thereby reduce the pain syndrome. In the case of pronounced stricture of the papilla or distal part of the pancreatic duct, ERCP can be effective with sphincterotomy, stenting, or dilatation.
Oral administration of hypoglycemic drugs is rarely effective in the treatment of diabetes caused by chronic pancreatitis. Insulin should be administered cautiously, as prolonged hypoglycemia may develop due to deficiency of glucagon secretion by a-cells and the lack of the effect of its secretion on hypoglycemia caused by insulin.
Patients who have chronic pancreatitis are at increased risk of pancreatic cancer. The increase in symptoms of chronic pancreatitis, especially associated with the development of stricture of the pancreatic duct, requires examination for malignancy. It may include a cytological analysis of scrapings from stricture or the determination of blood serum markers (eg CA 19-9 carcinoembryonic antigen).
