Medical expert of the article
New publications
Myocardial akinesia
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
When diagnosing cardiac diseases, myocardial akinesia may be detected, that is, its immobility or the inability of certain areas of the heart muscle tissue to contract.
Thus, myocardial akinesia is not a disease, but a pathological condition, a disorder of the normal motor function of the heart muscle, which is determined by ultrasound diagnostics of the heart and is one of the structural and functional signs of a number of diseases of the cardiovascular system.
Causes myocardial akinesia
Why does the heart muscle stop contracting, that is, what are the causes of myocardial akinesia?
In cardiology practice, the pathogenesis of the loss of normal contractile function of the myocardium (which, as is known, is performed automatically by a healthy heart) is most often associated with myocardial infarction and the resulting necrosis of part of the working cardiomyocytes. Post-infarction reparative changes (remodeling) of the myocardium first lead to an increase in the infarction zone, and then the shape of the ventricle is distorted and expanded, with the cardiomyocyte necrosis zone turning into a scar and forming a region of myocardial akinesia. Fibrous changes can also affect the septum separating the ventricles, and then ultrasound examination shows akinesia in the area of the interventricular septum.
Myocardial infarction is an acute condition of cardiac ischemia or ischemic heart disease (IHD), which develops when blood circulation in the coronary artery system is disrupted, which leads to myocardial hypoxia and the death of its cells.
In case of post-infarction thinning of the area of the muscular membrane of the heart and its protrusion – aneurysm – ultrasound cardiography reveals akinesia of the left ventricle. In almost two thirds of patients, aneurysm formation occurs in the left ventricle – on its anterior wall or at the apex, and here akinesia of the apex of the heart is also noted.
In addition, there is a correlation between echocardiographic results visualizing myocardial akinesia and post-infarction myocardial syndrome – focal or diffuse post-infarction cardiosclerosis with characteristic replacement of damaged cardiomyocytes with fibrous tissue, as well as with damage to the cardiac conduction system (impaired conduction of bioelectrical impulses by cells of the sinoatrial or atrioventricular nodes).
In cases of myocardial degeneration or dystrophy, which has a histomorphological picture similar to cardiosclerosis, changes in the structure of the cardiac muscle tissue also demonstrate focal myocardial akinesia.
Often there are damages to the cells of the sinoatrial node with a decrease in the amplitude of movement of the muscular wall and the absence of its contraction, i.e. a combination of hypokinesia and akinesia in patients with infectious myocarditis. This disease can be accompanied by the formation of inflammatory infiltrates in the interstitium and localized myocytolysis due to inflammation caused by viruses (adeno and enterovirus, Picornaviridae, Coxsackie virus, Parvovirus B, Rubella virus, HSV-6), bacteria (Corynebacterium diphtheriae, Haemophilus influenzae, Borrelia burgdorferi, Mycoplasma pneumoniae), as well as protozoa (Trypanosoma cruzi, Toxoplasma gondii), fungi (Aspergillus) or parasites (Ascaris, Echinococcus granulosus, Paragonimus westermani, etc.). As clinical statistics show, the most cases of infectious myocarditis are caused by diphtheria, influenza, enteroviruses and toxoplasma.
And with myocarditis of autoimmune etiology (associated with systemic lupus erythematosus, scleroderma, rheumatoid arthritis, Whipple's disease, etc.), akinesia of the left ventricle and its dysfunction may occur, fraught with life-threatening arrhythmias.
Separately, cardiologists distinguish stress cardiomyopathy (Takotsubo cardiomyopathy), which domestic specialists call broken heart syndrome. This sudden transient systolic dysfunction of the mid-apical segments of the left ventricle often occurs in stressful situations in elderly women who do not have a history of coronary heart disease. In particular, a hyperkinesis zone is detected at the base of the left ventricle, and above it, akinesia of the apex of the heart. Also, on ultrasound of the heart, diagnosticians can detect a lack of movement in the area of the interventricular septum.
Risk factors
The main risk factors for disorders of normal motor function of cardiac muscle areas in the form of myocardial akinesia are the development of ischemic heart disease. And the risk factors for its development, in turn, are considered to be:
- age over 45 years for men and over 55 years for women;
- family history of early heart disease;
- reduced levels of cholesterol-carrying HDL (high-density lipoproteins) in the blood and increased levels of low-density lipoproteins (LDL), which contribute to the deposition of cholesterol on the walls of blood vessels – atherosclerosis;
- high levels of triglycerides in the blood (related to diet);
- high blood pressure;
- metabolic disorder (metabolic syndrome) that contributes to increased blood pressure and cholesterol deposition in the coronary vessels;
- smoking (including passive smoking), obesity, lack of physical activity, psychological stress and depression.
Viral and bacterial infections affecting the myocardium, as well as autoimmune pathologies, trigger such a risk factor for myocardial ischemia as an increase in the level of C-reactive protein (CRP) in the blood. And the normal state of the heart vessels is disrupted by an imbalance of tissue plasminogen activators (tPA) and their inhibitors (PAI), which poses a threat of thrombosis of the coronary veins with their complete occlusion.
Pathogenesis
It is suggested that the pathogenesis of this cardiomyopathy lies in the inadequate response of the heart vessels (coronary arteries and/or arterioles and capillaries) to the release of catecholamine neurotransmitters into the blood, and that short-term abnormalities in myocardial contraction arise due to the vasospasm they provoke.
Symptoms myocardial akinesia
In case of myocardial akinesia – an echocardiographic sign of cardiovascular diseases – the clinical picture is determined by the symptoms of these pathologies. Among them are: shortness of breath, pain of varying intensity in the heart area, arrhythmia (atrial or ventricular), ventricular flutter, fainting.
Thus, with takotsubo cardiomyopathy, patients most often complain of pain behind the sternum (of a squeezing nature) radiating to the left shoulder blade and a feeling of lack of air when inhaling.
And pains with myocarditis can be both acute and prolonged (with no effect when using nitroglycerin), and muffled (squeezing). In addition, cardiac symptoms in this disease of infectious origin include shortness of breath, fever, increased heart rate, heart flutter; lightning-fast hemodynamic disturbances (a drop in blood flow volume velocity), loss of consciousness and sudden cardiac death are possible.
Complications and consequences
Certainly, myocardial akinesia, compared to dyskinesia of the post-infarction scar area, represents a more serious danger to the life of patients with myocardial infarction. Studies have shown that in approximately 40% of cases of infarction with coronary vessel obstruction, with timely restoration of blood flow in the ischemic segment (reperfusion), myocardial contractility will be restored within two to six weeks after the infarction. However, its consequences and complications include sudden cardiac tamponade, electromechanical dissociation, and death.
The consequences and complications of dystrophic changes in the myocardium with its partial akinesia lead to the almost inevitable atrophy of muscle fibers, which can manifest itself not only as arrhythmia and a decrease in systolic ejection, but also as an expansion of the heart chambers with chronic circulatory failure.
Left ventricular akinesia with its systolic dysfunction and heart failure are among the strongest predictors of the risk of sudden cardiac death.
 [ 23 ]
[ 23 ]
Diagnostics myocardial akinesia
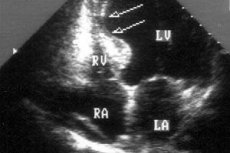
Only instrumental diagnostics of the myocardium using ultrasound examination of the heart – echocardiography – makes it possible to identify areas of its akinesia.
A special method of automatic segmental analysis of heart contractions allows tracking and recording all movements of the heart wall.
What do need to examine?
Differential diagnosis
Differential diagnosis of chest pain – in patients with an atypical clinical picture or diagnostically indeterminate electrocardiogram results – also involves the use of echocardiography.
In patients without myocardial motion disorder, echocardiography can be used to detect other life-threatening conditions with a similar clinical picture: massive pulmonary embolism or aortic dissection.
In addition, diagnostics of the myocardium, including in cases of its contractile function disorders, includes blood tests for ESR, C-reactive protein levels, antibodies (serological analysis of serum for IgM levels), electrolyte levels, and determination of myocardial damage markers (troponin I and T isoenzymes, creatine kinase).
Patients undergo an electrocardiogram (ECG), X-ray contrast coronary angiography, tomographic scintigraphy (with radioisotope substances), color tissue Doppler, and MRI. Diagnosis of cardiac aneurysms requires the use of X-ray contrast ventriculography.
In some cases, differential diagnosis of the myocardium is possible only with the help of endomyocardial biopsy followed by histology of the obtained sample.
Who to contact?
Treatment myocardial akinesia
Treatment of the myocardium is aimed at restoring the blood supply to its damaged areas (perfusion) and their conduction function, limiting the area of localized cardiomyocyte necrosis, and activating cellular metabolism.
In clinical practice, drugs of several pharmacological groups are used. In acute coronary syndromes and occlusive thrombosis of the epicardial coronary artery, reperfusion therapy is performed with thrombolytic drugs (Streptokinase, Prourokinase, Alteplase) and antiplatelet agents (Ticlopidine, Clopidogrel sulfate or Plavix).
In chronic heart failure, drugs are used that inhibit the angiotensin-converting enzyme (ACE) that regulates blood pressure: Captopril, Enalapril, Ramipril, Fosinopril. Their dosage is determined by a cardiologist depending on the specific disease and ECG readings. For example, Captopril (Capril, Alopresin, Tensiomin) can be prescribed at 12.5-25 mg - three times a day before meals (orally or under the tongue). Side effects of this drug and most drugs in this group include tachycardia, a drop in blood pressure, kidney dysfunction, liver failure, nausea and vomiting, diarrhea, urticaria, increased anxiety, insomnia, paresthesia and tremor, changes in the biochemical composition of the blood (including leukopenia). It should be borne in mind that ACE inhibitors are not used in cases of idiopathic myocardial pathologies, high blood pressure, stenosis of the aorta and renal vessels, hyperplastic changes in the adrenal cortex, ascites, pregnancy and childhood.
In case of coronary heart disease and cardiomyopathy, anti-ischemic drugs of the peripheral vasodilator group may be prescribed, for example, Molsidomine (Motazomine, Corvaton, Sidnofarm) or Advocard. Molsidomine is taken orally - one tablet (2 mg) three times a day; contraindicated in case of low blood pressure and cardiogenic shock; side effect - headache.
The antiarrhythmic and hypotensive drug Verapamil (Veracard, Lekoptin) is used for coronary heart disease with tachycardia and angina: one tablet (80 mg) three times a day. There may be side effects in the form of nausea, dry mouth, intestinal problems, headaches and muscle pain, insomnia, urticaria, and heart rate disturbances. This drug is contraindicated in severe heart failure, atrial fibrillation and bradycardia, and low blood pressure.
The drug Mildronate (Meldonium, Angiocardil, Vasonate, Cardionate and other trade names) has a cardiotonic and antihypoxic effect. It is recommended to take one capsule (250 mg) twice a day. This drug can only be used by adult patients and is contraindicated in cases of cerebral circulation disorders and structural pathologies of the brain. When using Mildronate, side effects such as headaches, dizziness, cardiac arrhythmia, shortness of breath, dry mouth and cough, nausea, and intestinal disorders are possible.
Drugs of the β1-adrenoblocker group for coronary heart disease (Metoprolol, Propranolol, Atenolol, Acebutolol, etc.) primarily reduce blood pressure, and by reducing sympathetic stimulation of receptors on myocardial cell membranes, they reduce heart rate, reduce cardiac output, increasing oxygen consumption by cardiomyocytes and relieving pain. For example, Metoprolol is prescribed one tablet twice a day, Atenolol is enough to take one tablet per day. However, drugs of this group increase the risk of acute heart failure and atrial and ventricular block, and their use is contraindicated in the presence of congestive and decompensated heart failure, bradycardia, and circulatory disorders. Therefore, many experts currently question the antiarrhythmic effect of these drugs.
Relieving heart pain is of primary importance, as sympathetic activation during pain causes constriction of blood vessels and increases the load on the heart. Nitroglycerin is commonly used to relieve pain. Detailed information in the article - Effective Pills That Relieve Heart Pain
Doctors recommend taking vitamins B6, B9, E, and to support the cardiac conduction system – medications containing potassium and manganese (Panangin, Asparkam, etc.).
Surgical treatment
In cases of infarctions with damage to the coronary arteries (leading to the formation of an area of myocardial ischemia and its akinesia with expansion of the heart chambers), surgical treatment is indicated to restore blood flow to the heart - aortocoronary bypass.
In case of ischemic heart disease, coronary dilation (expansion of the lumen) is used – stenting.
Surgical treatment is most often used for dyskinetic aneurysm: either by aneurysmectomy (resection), or by suturing the aneurysmal cavity (aneurysmoplasty), or by strengthening its wall.
A method of dynamic cardiomyoplasty has been developed, which involves the restoration or enhancement of myocardial contractility using electrically stimulated skeletal muscle (usually a flap from the edge of the latissimus dorsi muscle) wrapped around part of the heart (with partial resection of the second rib). The muscle flap is sutured around the ventricles, and its synchronous stimulation with cardiac contractions is carried out using intramuscular electrodes of an implantable cardiac pacemaker.
Prevention
Return to the Risk Factors section, and the methods by which cardiovascular pathologies can be prevented will become obvious. The main thing is not to gain weight, move more and not let cholesterol settle in the form of plaques on the walls of blood vessels, and for this it is useful after 40 years (and the presence of heart pathologies in blood relatives) to follow the Diet for Atherosclerosis
And, of course, cardiologists consider quitting smoking to be the most important condition for preventing ischemic damage to the myocardium. The fact is that when smoking, the hemoglobin proteins of the red blood cells combine with the gases of inhaled tobacco smoke, forming a compound that is very harmful to the heart - carboxyhemoglobin. This substance prevents blood cells from carrying oxygen, which leads to hypoxia of the cardiomyocytes of the heart muscle and the development of myocardial ischemia.
Also read – Prevention of post-infarction cardiosclerosis
Forecast
Cardiologists are reluctant to provide prognostic information: it is difficult to make an accurate prognosis of post-infarction dyskinesia, hypokinesia, and akinesia.
To assess the prognosis for mortality after acute myocardial infarction, experts from the American Society of Echocardiography introduced the Wall Motion Index (WMI). However, it does not have a full-fledged long-term prognostic value.
As for myocarditis, according to statistics, almost 30% of cases end in recovery, and in the rest, chronic dysfunction of the left ventricle becomes a complication. In addition, about 10% of cases of viral and microbial myocarditis lead to the death of patients. Total akinesia of the myocardium leads to cardiac arrest.

