Medical expert of the article
New publications
Myocardial dystrophy: acute, fatty, ischemic, focal, in athletes
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Myocardial dystrophy is considered a pathological process based on damage to the heart muscle, which occurs as a result of metabolic and biochemical disorders.
Some sources suggest that myocardial dystrophy should not be singled out as a separate pathology, but considered a clinical manifestation of some disease. However, this pathology, in comparison with, for example, cardiomyopathy, clearly outlines the processes occurring in the heart muscle.
Myocardial dystrophy is distinguished only in cases where metabolic disorders have been proven, resulting in muscle damage.
Causes myocardial degeneration
For a hundred years now, there has been a classification that distinguishes two groups of causes of cardiac muscle dystrophy. It is based on various diseases that directly or indirectly affect metabolic processes in the myocardium.
Causes of myocardial dystrophy of the first group include heart diseases, in particular, myocarditis, ischemic heart disease and cardiomyopathy.
The second group indicates extracardiac pathology, which through hormones, blood elements or nervous regulation can have a negative effect on the muscular layer.
This group should include anemia, when the level of red blood cells and hemoglobin is below acceptable standards, chronic tonsillitis, intoxication, both internal and external, in particular, occupational poisoning.
In addition, the causes of this pathology imply the negative effect of drugs, the dose and duration of which exceeded the permissible limits. This applies to hormonal agents, cytostatics and antibacterial drugs.
Diseases of endocrine organs, such as the adrenal glands or thyroid gland, affecting hormonal levels, also contribute to degenerative processes in the heart muscle. Chronic kidney and respiratory diseases should not be forgotten.
Separately, it is necessary to highlight sports dystrophy, when excessive physical exertion, which the heart muscle cannot cope with, leads to its damage.
Due to the impact of the above reasons, the muscular layer begins to experience a lack of energy. In addition, toxic substances formed as a result of metabolic processes accumulate in cardiomyocytes, which causes additional damage (endogenous intoxication).
Thus, the functional cells of the heart muscle die, in place of which connective tissue foci are formed. It is worth noting that such areas are not able to perform the functions of cardiomyocytes, as a result of which "dead" zones arise.
The compensatory mechanism is an increase in the heart cavity, which causes a weak contractile process. In this case, the organs do not receive a full volume of nutrients and oxygen, hypoxia increases. As the pathological process progresses, heart failure occurs.
Symptoms myocardial degeneration
The clinical manifestations of the pathology can vary significantly, ranging from a complete absence of symptoms to signs of heart failure with severe shortness of breath, edema and hypotensive syndrome.
Symptoms of myocardial dystrophy are initially absent, but sometimes painful sensations in the heart area are possible. They appear as a result of intense physical exertion or after a psycho-emotional outburst, while at rest the pain subsides.
At this stage, few people seek help from a doctor. Later, shortness of breath, swelling of the shins and feet gradually appear, which increases towards evening, attacks of pain in the heart become more frequent, tachycardia, heart rhythm disturbances and severe weakness appear.
All these symptoms already indicate the onset of heart failure, which worsens the prognosis for recovery.
In some cases, for example, with climacteric myocardial dystrophy, pain is observed in the heart area, especially above the apex, which spreads to the entire left side of the chest. Their nature can be stabbing, pressing or aching, and the intensity does not change after taking nitroglycerin.
Quite often, all these symptoms can be combined with other vegetative manifestations of menopause, such as facial flushing, a feeling of heat and increased sweating.
Alcoholic muscular dystrophy is characterized by the appearance of tachycardia, a feeling of lack of air and cough. Extrasystole and atrial fibrillation can often be observed on the ECG.
Myocardial dystrophy in athletes
First, we need to understand how the muscle layer cells work at rest and under load. Thus, cardiomyocytes work at full capacity even at rest, but the heart contracts and relaxes from 60 to 90 times per minute.
When doing physical exercise, especially when running, the heart rate increases by 2 or more times. When the pulse reaches 200 per minute, the heart does not have time to relax completely, that is, there is practically no diastole.
That is why myocardial dystrophy in athletes is caused by an increase in internal tension in the heart, as a result of which blood circulates poorly and hypoxia develops.
When there is a lack of oxygen, anaerobic glycolysis is activated, lactic acid is formed, and some organelles, including mitochondria, are destroyed. If the loads exceed the norm, cardiomyocytes are in almost constant hypoxia, which leads to their necrosis.
Myocardial dystrophy in athletes develops through the replacement of cardiac muscle cells with connective tissue that is incapable of stretching. In athletes who died suddenly, microinfarctions in the heart were found during autopsy, which confirms poor blood circulation in the myocardium.
In addition, connective tissue conducts nerve impulses poorly, which can manifest itself as arrhythmia and even cardiac arrest. Most often, death occurs at night after intense training, the cause of which is microinfarctions as a result of improperly selected physical activity.
Forms
Ischemic myocardial dystrophy
As a result of short periods of insufficient oxygen supply to the heart muscle, ischemic myocardial dystrophy may develop. However, it should be taken into account that at the time of ischemia, characteristic changes are recorded on the ECG, but at the same time, markers of muscle damage are absent (transaminases, lactate dehydrogenases).
Pathogenetically, the muscular layer looks flabby, pale with areas of insufficient oxygen supply and edema. Sometimes a thrombus can be found in the arteries that feed the heart muscle.
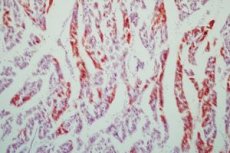
Microscopic examination is characterized by vascular paresis, in particular capillary dilation, erythrocyte stasis, and interstitial tissue edema. In some cases, hemorrhages and leukocyte diapedesis are observed, as well as groups of neutrophils in the peripheral area of myocardial ischemia.
In addition, muscle fibers lose striation and glycogen reserves. Staining reveals necrotic changes in cardiomyocytes.
Among the clinical symptoms, it is worth highlighting angina pectoris - pain in the heart area, a feeling of shortness of breath, a feeling of fear and increased blood pressure.
A complication may be acute heart failure, which in some cases is the cause of death.
 [ 10 ]
[ 10 ]
Focal myocardial dystrophy
One of the forms of ischemic heart disease is focal myocardial dystrophy. Morphologically, it is the formation of small pathological foci of the heart muscle and is considered an intermediate form between angina and infarction.
The cause of the development of pathological foci is a violation of blood circulation in the arteries that feed the heart muscle. Most often, people over 50 suffer from this pathology. Pain in the heart area initially occurs during intense physical activity, but as it progresses, it bothers even at rest.
In addition to pain, a person may experience a feeling of insufficient inhalation and dizziness. Also, a dangerous condition is a disturbance of the rhythm and an increase in the heart rate of more than 300 per minute. Such tachycardias can lead to death.
There is also asymptomatic focal myocardial dystrophy, when a person does not experience any symptoms of pathology. In such people, even a heart attack can be painless.
To avoid worsening symptoms, it is necessary to see a doctor and undergo instrumental examinations, such as ECG and ultrasound of the heart. In this way, it is possible to visualize the areas of damage to the muscle layer and begin timely treatment.
 [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ]
[ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ]
Fatty myocardial degeneration
In some cases, among normal cardiomyocytes, there appear those in which small droplets of fat accumulate. Over time, the size of the fat inclusions gradually increases and eventually replaces the cytoplasm. This is how fatty myocardial dystrophy is formed.
In the cells of the heart muscle, mitochondria are destroyed, and upon autopsy, one can observe varying degrees of fatty heart disease.
A minor degree of pathology activity can be visualized only with a microscope, but a more pronounced lesion causes an increase in the size of the heart. In this case, the cavities are stretched, the muscle layer is flabby, dull and clay-yellow in color.
Fatty myocardial degeneration is a sign of a decompensated condition. As a result of gradual accumulation of fatty inclusions in cardiomyocytes, a violation of cellular metabolism processes and destruction of lipoproteins of cardiac cell structures occurs.
The main factors in the occurrence of fatty muscle damage are insufficient oxygen supply to the myocardium, metabolic pathology as a result of an infectious disease, as well as an unbalanced diet with low levels of vitamins and proteins.
 [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ]
[ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ]
Left ventricular myocardial dystrophy
Left ventricular damage is not an independent pathology, but is a manifestation or consequence of some disease.
Left ventricular myocardial dystrophy is characterized by a decrease in the thickness of the muscular layer, which causes the appearance of some clinical symptoms. These include weakness, a feeling of exhaustion, heart rhythm disturbances, which are felt as interruptions, as well as pain syndrome of varying intensity.
In addition, a person may experience shortness of breath when walking or during intense physical activity, which reduces performance and increases fatigue.
As the dystrophy progresses further, swelling of the legs and feet, increased heart palpitations and a drop in blood pressure may occur.
Laboratory tests may reveal insufficient levels of hemoglobin in the blood, which contributes to the development of anemia.
Left ventricular myocardial dystrophy contributes to dysfunction of other organs and systems. Without timely effective treatment, the pathological condition can lead to heart failure in the near future, which significantly worsens the general condition of a person.
As a result of severe physical overexertion, hemorrhages, necrotic processes and toxic damage to cardiomyocytes can be observed in the myocardium. Clinically, this can be manifested by a decrease in heart rate and a decrease in pressure.
Myocardial dystrophy with insufficient nutrition can provoke atrophy of muscle fibers, which is a consequence of pathological metabolism. Nitrogenous bases, bile acids and ammonium are found in the blood.
Manifestations of acidosis can be observed when this pathology is combined with diabetes mellitus. As for hyperthyroidism, it contributes to weakening and decreasing the thickness of the muscle layer. In parallel, pressure and cardiac output increase.
Complications include atrial fibrillation, murmur during systole, and the appearance of dilatation of the heart cavities. The pathological process then progresses, and circulatory failure is added.
Dyshormonal myocardial dystrophy
Damage to the heart muscle as a result of hormonal imbalance is observed with thyroid dysfunction or as a result of secondary hormonal imbalance.
Dyshormonal myocardial dystrophy is more common after 45-55 years. In men, the pathology is associated with impaired testosterone secretion, and in women - estrogens during menopause or with gynecological diseases.
Hormones affect the exchange of proteins and electrolytes in the cells of the heart muscle. With their help, the content of copper, iron, and glucose in the bloodstream increases. Estrogens activate the process of fatty acid synthesis and contribute to the deposition of energy reserves for cardiomyocytes.
Since this pathology can arise and progress quite quickly, women during menopause are recommended to regularly undergo heart function tests for early detection of the pathological process.
As for the thyroid gland, its function can be reduced or increased, which affects metabolic processes in the muscle layer and the development of dystrophic processes.
Treatment of this type of pathology consists of eliminating the cause of its development, namely normalizing hormone levels and restoring the normal functioning of the endocrine organs.
With the help of medications, a person can get rid of such clinical manifestations as stabbing pain in the heart area spreading to the left arm, heart problems (increased heart rate, decreased heart rate and arrhythmia), as well as changes in the psycho-emotional state.
In addition, a person may experience irritability, increased nervousness, dizziness, sleep disturbances, and weight loss. Most often, these symptoms are characteristic of thyrotoxicosis.
Myocardial damage due to insufficient thyroid function can manifest itself as aching pain in the heart spreading to the left arm, dull tones, swelling and decreased pressure.
Diagnostics myocardial degeneration
Changes in cardiomyocytes and the muscular layer as a whole are a consequence of the progression of any disease. When contacting a doctor, his main task is to detect the main pathology and prescribe the correct therapy for its treatment.
In the process of communication with the patient, the first information about his complaints, the time of their occurrence and progression appears. In addition, the doctor during an objective examination can detect visible clinical manifestations of the disease, especially during auscultation of the heart. It is especially necessary to ask about past illnesses and sports activities, to exclude or suspect myocardial dystrophy in athletes.
Diagnosis of myocardial dystrophy also involves the use of instrumental methods. Thus, thyroid ultrasound can show its structure, and laboratory tests can determine the level of its hormones and assess its functionality. Also, a clinical blood test can indicate the presence of anemia if the hemoglobin level is low.
Particular importance is given to ECG when rhythm disturbances are visualized, and clinically the pathology does not manifest itself in any way. Ultrasound helps to detect changes in cardiac contractility and assess the ejection fraction. However, significant pathological foci can be seen only in severe heart failure. Ultrasound also indicates an increase in the cavities of the heart and changes in the thickness of the myocardium.
Confirmation can be obtained after a biopsy, when a piece of muscle tissue is taken and carefully examined. This manipulation is very dangerous, so it cannot be used with every suspicion of dystrophic processes.
A new method is nuclear MRI, when radioactive phosphorus is introduced into the body and its accumulation in the cells of the muscle layer is assessed. The result can be used to judge the level of pathology. Thus, a reduced amount of phosphorus indicates insufficient energy reserves of the heart.
What do need to examine?
Who to contact?
Treatment myocardial degeneration
In mild cases of pathology and in the absence of heart failure, patients can undergo treatment for myocardial dystrophy in a clinic or in a day hospital, but always under the supervision of a physician.
The main task is to identify and eliminate the cause that caused metabolic disorders in cardiomyocytes. Successful treatment of the underlying disease ensures complete regression of dystrophic processes or significant improvement of the clinical and morphological picture.
In case of thyroid dysfunction, it is necessary to consult an endocrinologist, who should adjust the treatment and prescribe hormonal agents.
In the presence of anemia, iron preparations, vitamin complexes or erythropoietin should be used. Therapy for chronic tonsillitis consists of the use of antibacterial and anti-inflammatory drugs. If the effect is insufficient, tonsillectomy is recommended - a surgical operation to remove the tonsils.
Treatment also involves influencing the trophism of the muscle layer. For this purpose, cardiotropic drugs can be used that will nourish the heart muscle. They normalize metabolic processes and thereby improve heart function. These include magnesium, potassium in the form of panangin and magnerot, vitamins B, C and folic acid. Such drugs as riboxin, retabolil and mildronate have proven their effect.
If the cause of pain in the heart is psycho-emotional stress, it is recommended to use sedatives, such as Corvalol, valerian, motherwort, barboval or Novo-Passit.
In the presence of arrhythmias, calcium channel blockers such as verapamil, beta blockers (metoprolol) or cordarone should be used. During treatment, it is imperative to monitor heart activity using an ECG. Heavy physical activity should be excluded during the therapeutic course. After the disappearance of clinical manifestations of the pathological process, cardiotropic drugs should be taken for another month. This course should be repeated 2-3 times a year for the next 3-5 years.
Prevention
Based on the already known causes of the pathology, prevention of myocardial dystrophy should include measures to eliminate the underlying disease that negatively affects cardiomyocytes.
For preventive purposes, it is necessary to regularly take vitamin and mineral complexes. However, do not forget about proper nutrition and rest. It is also necessary to avoid stressful situations in order to avoid disruption of the psycho-emotional state and to engage in physical activity in a measured manner.
Athletes' training should be designed taking into account gender, age and the presence of concomitant pathology in a person. A mandatory condition is the sanitation of all chronic foci and control over the activity of existing diseases.
Prevention involves the use of a minimum amount of medications in strictly selected dosages. Failure to comply with the regimen of taking medications threatens intoxication and damage to the muscular middle layer.
During periods of intense exercise, during menopause and in old age, it is necessary to undergo regular examinations to determine the functioning of the heart, at least by performing an ECG and ultrasound.
Forecast
The prognosis of myocardial dystrophy depends on each person, since timely consultation with a doctor and rapid initiation of treatment can ensure complete regression of the pathological process and elimination of clinical manifestations.
However, if complications such as heart failure occur, the prognosis depends on the severity of the pathology and may have an unfavorable outcome. Due to the lack of treatment, the general condition and quality of life of a person significantly worsens.
In advanced stages, sometimes even a heart transplant is required, since medications cannot independently cope with degenerative processes and their consequences.
Myocardial dystrophy is not registered very often due to the absence of clinical symptoms at the initial stage. With the help of regular examinations and performing ECG and ultrasound of the heart, it is possible to avoid further progression of the pathology and activate the processes of restoration of the normal structure of cardiomyocytes.

