Medical expert of the article
New publications
Incomplete heart block
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Partial slowing or interruption of impulses from the upper chambers of the heart (atria) through the atrioventricular node (AV node) and/or the bundle of Hiss to the lower chambers (ventricles) with impaired synchronization between them is defined as incomplete heart block.
Epidemiology
Given the asymptomatic nature of mild partial AV blockade (approximately two thirds of cases), the clinical statistics of this cardiac conduction disorder is very approximate. The prevalence of incomplete right bundle branch block in the general population is estimated at 3-7%, it is a frequent finding during ECG at any age, especially in men and athletes.
The researchers found that in a significant proportion of cases of incomplete blockade, its causes are acute myocardial infarction and cardiac pathologies of structural nature, in particular, in elderly people - idiopathic degenerative fibrosis of the conduction system structures. [1]
Causes of the incomplete heart block
Partial heart block - atrial-ventricular or atrioventricular block i and II degree - is characterized by a slower or irregular heart rhythm due to disruption of the conduction system of the heart,
Among the most frequent causes of this condition, experts name: ischemic heart disease (with focal myocardial pathology and fibrosis); myocardial infarction (more precisely, postinfarction cardiosclerosis ); heart failure; degenerative fibrosis of the branches of the bundle of Hiss (Leva's disease or Lenegre syndrome); rheumatic heart disease (with diffuse myocardial changes); congenital heart disease (including valve disease); cardiomyopathies (dilated, hypertrophic, restrictive); pulmonary embolism.
In addition, incomplete atrial-ventricular block can be drug-induced and develops due to long-term use of foxglove drugs, β1-adrenoreceptor blockers, antiarrhythmic agents, etc. Read more in the publication - drug-induced arrhythmias
Also, this condition as an adaptation variant under constant increased physical loads can be observed in athletes: they may have heart enlargement and remodeling of the left ventricle with thickening of its free wall. For such cases in domestic cardiology there is a concept athletic heart, and foreign specialists use the term "athletic heart syndrome".
Incomplete heart block in a child is congenital and acquired. Congenital causes include congenital heart defects (e.g., atrial septal defect) and gene mutations brugada syndrome in children (with delayed conduction of impulses through the right atrium due to right bundle branch block). The cause of acquired atrial-ventricular conduction disturbance is most often myocarditis in children.
Risk factors
The risk of developing incomplete heart block is increased:
- In deterioration of coronary circulation associated with atherosclerosis of the arteries supplying the heart;
- With severe hypertension;
- In people with diabetes;
- For cardiac neoplasms;
- Due to electrolyte imbalance;
- After surgical interventions on the heart, catheterization of its departments and other procedures;
- When heart muscle is damaged due to chest trauma;
- In patients with autoimmune diseases (e.g., sarcoidosis or SLE), systemic amyloidosis, or systemic scleroderma;
- In the presence of vasovagal syndrome (increased activity of the autonomic vagus nerve).
Pathogenesis
Myocardial conductive myocytes, the cells of the heart's conductive system, are responsible for the execution of its contraction-relaxation cycle by conducting electrical signals (ion fluxes through intercellular gap junctions) from the atria to the ventricles. These specialized cardiomyocytes are located in the sinotrial (sinus-atrial) node, inter-nodal pathways, atrioventricular (atrial-ventricular) node, atrioventricular bundles (Gis bundles) and Purkinje fibers.
The basis of coordinated cardiac contraction is the orderly propagation of electrical signals between neighboring cardiomyocytes and throughout the heart.
In this case, the rhythm driver - sinus node (SA-node) - works as it should and generates normal impulses, i.e. Sinus rhythm of the heart and incomplete blockade are combined, which consists in violation of transmission of these impulses either between the SA-node and atria, or below the AV-node - along the legs of the bundle of Hiss.
And the pathogenesis of heart block is associated with disturbances in the propagation of these signals by the conducting cardiomyocytes of the Guis bundles.
When all impulses from the AV node pass to the ventricles along the legs of the bundle of Hiss, but with a significant slowdown, this is AV-blockade of the I degree. In cases of AV-blockade of ²² degree, not all the signals are conducted along the legs of the heart (bundle of Hiss) to the ventricles. Such incomplete blockade of the ventricles leads to pauses between their contractions with delayed activation of the ipsilateral ventricle.
Read more - heart rhythm and conduction disorders
Symptoms of the incomplete heart block
Dizziness and general weakness are the first signs of partial blockade of impulse conduction from the atria to the ventricles of the heart. Pre-syncope and cardiogenic syncope may occur.
Also, clinical symptoms are manifested by abnormalities and rhythm of the heart, interruptions in heart, in particular, in the form of bradycardia and bradysystolic form of atrial fibrillation. Dyspnea, chest pain and nausea may occur.
More information in the materials:
- Heart rhythm and conduction disorder: symptoms and diagnosis
- Hiss bundle branch blockade: causes, symptoms, diagnosis, treatment
The types of blockade - right bundle branch blockade of the left bundle branch of the Hiss bundle - do not differ much symptomatically.
Incomplete blockade of the left ventricle of the heart (where the great circle of blood circulation originates) is incomplete or incomplete blockade of the left leg of the bundle of Hiss. This blockade delays the response of the left ventricle (QRS complex duration of more than 120 ms on ECG), and the right ventricle is activated and contracts before the left ventricle.
In grade I blockade, the ECG shows atrial-ventricular slowing due to the movement of the impulse from the CA node to the ventricle. Most people do not experience symptoms because the blood supply to the brain is not affected, but weakness, dizziness, drowsiness, pulse irregularities, and shortness of breath may occur.
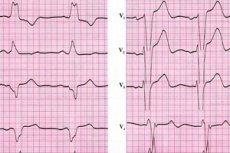
Right bundle branch block or incomplete right bundle branch block is an incomplete blockade of the right ventricle of the heart (where the small circle of blood circulation originates); the delay of electrical signals, leading to a violation of the regularity of the heartbeat, occurs in the right side of the heart. The electrocardiogram shows a widening of the QRS complex with a duration of more than 90-100 ms and an elevation of the R tooth, as well as the absence of the Q tooth and a shift of the ST and T tooth opposite to the main deviation of the ventricular complex. That is, the impulse does not pass simultaneously from the left and right sides, and the signal from the right side is delayed, giving an irregular heartbeat and causing an increase in pressure in the right ventricle. [2]
Complications and consequences
On its own, incomplete or partial heart block is usually not dangerous, although it can progress to complete heart block (with a prevalence in patients of 27-35%), and complete block is fraught with cardiac arrest.
Also complications of incomplete atrial-ventricular block are:
- Atrial fibrillation (atrial fibrillation);
- Aggravation of congestive heart failure, CHD and ventricular arrhythmias;
- Morgagni-Adams-Stokes syndrome, resulting from decreased cardiac output and impaired systemic blood supply;
- In the presence of acute myocardial infarction - development of arrhythmic cardiogenic shock.
Diagnostics of the incomplete heart block
The main role is played by instrumental diagnostics:
- Electrocardiography,
- Cardiac ultrasound - echocardiography,
- X-ray cardiac function study.
To find out the cause of partial blockage of conduction of impulses from the atria to the ventricles of the heart, laboratory tests are carried out - blood tests: general, for the level of glucose, cholesterol and triglycerides, C-reactive protein, troponin, AST and ALT enzymes, amylase, thyroid hormones.
Differential diagnosis is also performed, the task of which is to distinguish incomplete AV blockade and Hiss bundle branch blockade from other diseases and pathologies accompanied by a decrease in heart rate.
Who to contact?
Treatment of the incomplete heart block
A mild asymptomatic degree of incomplete atrial-ventricular block may not require any treatment.
Treatment of incomplete second-degree heart block depends on its cause and severity, and is most often directed at the disease or pathology that caused it.
When heart defects are the cause of Hiss bundle branch block, their surgical correction is required. Chronic arterial hypertension requires the prescription of adequate hypotensive drugs.
Ischemic heart disease and chronic heart failure are treated; myocarditis is treated with anti-inflammatory drugs, and rheumocarditis with corticosteroids and nonsteroidal anti-inflammatory drugs; in cardiosclerosis, combined cardiotonic drugs such as advocard are prescribed; in case of marked decrease in HR, beta-adrenomimetics.
In severe cases, it may be necessary to have surgery to place a pacemaker.
Prevention
There are no special preventive recommendations that could we prevent incomplete heart block, so one thing remains - to lead a healthy lifestyle.
Forecast
When predicting the outcome of incomplete heart block, cardiologists consider its causes, the absence or presence of symptoms (and their severity), and the fact that it will progress to complete heart block - with an increased risk of full cardiac arrest.
Can I enlist in the army if I have incomplete heart block? If it is a mild form that does not cause any symptoms, military service is possible.

