Medical expert of the article
New publications
Sports heart
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
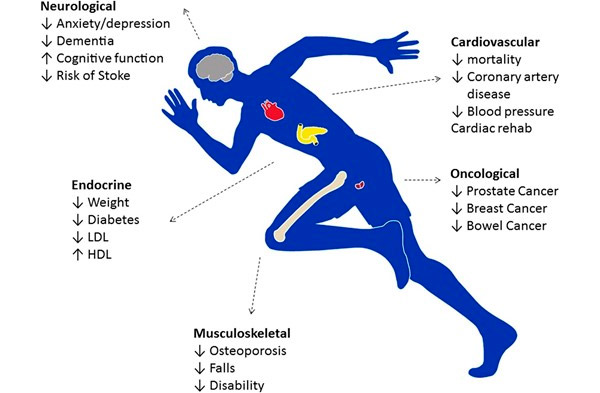
It has long been known that regular moderate exercise has many benefits. Exercise reduces the risk of heart disease, hypertension, [ 1 ] heart failure, depression, improves blood lipid profiles, [ 2 ] and increases insulin sensitivity. [ 3 ] Those who exercise regularly live longer and are more functional throughout their lives.
In addition to cardiovascular benefits, exercise reduces the risk of prostate and breast cancer, [ 4 ] prevents osteoporosis, and may slow the onset of dementia. [ 5 ] Exercise also increases stamina, boosts self-confidence, and is considered by many to be an antidepressant. [ 6 ] In terms of life expectancy, people who exercise regularly live at least 3 years longer than sedentary people, making exercise the most effective, accessible, and affordable therapy a doctor can prescribe.
Current European guidelines [ 7 ] and American guidelines [ 8 ] recommend that adults do at least 150 minutes of moderate-intensity exercise per week. Competitive athletes (and some recreational athletes) perform significantly higher than these recommendations and regularly perform more than 20 hours of intense exercise (15 METs) per week. Such intense levels of exercise require sustained 5-6-fold increases in cardiac output over long periods of time, accompanied by a host of unique electrical, structural, and functional adaptations of the heart, collectively referred to as the “athlete’s heart”. [ 9 ]
Athlete's heart is a set of structural and functional changes that occur in the heart of people who exercise for more than 1 hour almost every day. The condition does not cause subjective complaints. Manifestations include bradycardia and/or systolic murmur. Changes in ECG data are common. Diagnosis is clinical or by echocardiography. No treatment is necessary. Athlete's heart is important because it must be distinguished from serious heart diseases.
Pathogenesis
Intensive, long-term endurance and resistance training results in physiological adaptations of the body and the heart in particular. Left ventricular (LV) volume and pressure increase, which over time leads to increases in left ventricular muscle mass, wall thickness, and size. Maximal stroke volume and cardiac output increase, contributing to a lower resting heart rate and a longer diastolic filling time. The lower heart rate is primarily due to increased vagal tone, but other factors that decrease sinus node activity may be involved. Bradycardia reduces myocardial oxygen demand; at the same time, total hemoglobin content and the blood's ability to transport larger volumes of oxygen increase. Despite these changes, systolic and diastolic function remain normal. Structural changes are usually less pronounced in women than in men of the same age, body weight, and training status.
Heart structure: key points
- Predominantly eccentric left ventricular hypertrophy is observed in sports with high dynamic and low static loads (for example, running).
- Sports with high static loads (e.g. weight lifting) lead to predominantly concentric hypertrophy.
- In sports with high dynamic and high static loads (for example, cycling), hypertrophy is mixed and balanced. [ 10 ]
Symptoms of the athletic heart
There are no subjective complaints. Manifestations are variable, but may include the following:
- bradycardia;
- the LV impulse, which is shifted to the left, increases and grows in amplitude;
- systolic ejection murmur on the left at the lower border of the sternum;
- III heart sound (S 3 ), arising as a result of early, rapid diastolic filling of the ventricles;
- IV heart sound (S 4 ), which is heard best at rest against the background of bradycardia, since the diastolic filling time of the ventricles is increased;
- hyperdynamic pulse in the carotid arteries.
These symptoms reflect structural changes in the heart that occur as a result of adaptation to intense physical activity.
Where does it hurt?
Diagnostics of the athletic heart
Cardiovascular examination of an athlete
Cardiac examination should be performed in a stable condition, not during recovery from a prolonged period of exercise or competition, in a quiet, comfortable environment with privacy and room temperature. The examination should be performed in a sitting and supine position, with the addition of maneuvers such as the Valsalva maneuver, standing, and squatting if a significant murmur is detected.
Signs are usually discovered during routine screening or testing for other reasons. Most athletes do not require extensive testing, although an ECG is necessary. If symptoms suggest heart disease, an ECG, echocardiogram, and stress test are performed.
Athlete's heart is a diagnosis of exclusion and must be distinguished from disorders that cause similar manifestations but are life-threatening (eg, hypertrophic or dilated cardiomyopathies, ischemic heart disease, arrhythmogenic right ventricular dysplasia).
ECG reveals sinus bradycardia, sometimes with a heart rate of less than 40 beats per minute. Sinus arrhythmia often accompanies a low heart rate. Bradycardia at rest may predispose to an increase in the frequency of atrial or ventricular arrhythmias, including pacemaker migration through the atria and (rarely) atrial fibrillation, but pauses after ectopic impulses do not exceed 4 s. First-degree atrioventricular (AV) block is found in approximately one third of athletes. Second-degree AV block (mainly type 1), which occurs at rest but disappears with exertion, is less common. Third-degree AV block is a pathological condition and an indication for further examination. ECG abnormalities include high QRS voltage with abnormal waves or wave ratios reflecting left ventricular hypertrophy and abnormal early depolarization with biphasic waves in the anterior leads reflecting nonuniform repolarization with decreased sympathetic tone at rest. Both abnormalities resolve with exercise. Deep wave inversion in the anterolateral leads and incomplete right bundle branch block are also possible. ECG abnormalities correlate poorly with training status and cardiovascular function.
The athlete's heart may be associated with rhythm and conduction changes, morphological changes in the QRS complex, and repolarization abnormalities.[ 11 ] Factors that play a role in one or more of these changes include decreased intrinsic heart rate, increased parasympathetic or vagal tone, decreased sympathetic tone, structural cardiac adaptations, and inhomogeneous ventricular repolarization. The changes are most often observed in athletes engaged in high-intensity dynamic endurance events. It is important to recognize that some ECG changes that may accompany athletic training resemble abnormal ECG features and may mimic structural heart disease.
Electrocardiographic changes
Rhythm disturbances
- Sinus bradycardia
- Sinus arrhythmia, primarily associated with breathing.
- Sinus arrest with ectopic escape beats or rhythm or resumption of sinus rhythm.
- Wandering atrial pacemaker
- Other rhythms such as junctional rhythm, coronary sinus rhythm.
Atrioventricular block
- First degree atrioventricular block
- Second-degree atrioventricular (AV) block, Moebitz type I or Wenckebach type.
- Atrioventricular dissociation.
Higher-degree AV blocks have been observed rarely in athletes; they may indicate underlying cardiac disease and are an indication for further investigation.
Morphological changes
- Increased amplitude of P wave and notch
- Increased QRS voltage
- signs of LVH - for example, an increase in the Sokolov and Lyon index (SV1 + RV5)
- signs of PG - for example, an increase in RV1 + SV5
- incomplete right bundle branch block
- The frontal QRS axis is usually between 0–90° and is, on average, normal.
Repolarization disorders
ST segment
- Height of point J
- ST segment elevation
- ST segment depression
T wave
- Tall and pointed T waves
- T waves with teeth
- low amplitude or isoelectric T waves
- biphasic T waves
- biphasic T waves with terminal negativity
- inverted T waves.
Echocardiography helps differentiate athlete's heart from cardiomyopathy, but there is no clear boundary between physiological and pathological cardiac enlargement. In general, echocardiographic changes correlate poorly with the level of training and cardiovascular function. Mild mitral and tricuspid regurgitation are often detected.
During the exercise test, the heart rate remains below normal at submaximal exercise, increases accordingly and is comparable to that of nonathletes at maximal exercise. The heart rate recovers rapidly after exercise. The blood pressure response is normal: systolic blood pressure increases, diastolic blood pressure falls, and mean blood pressure remains relatively constant. Many of the resting ECG changes diminish or disappear during exercise; this finding is unique and pathognomonic of athlete's heart syndrome as opposed to pathological conditions. However, pseudonormalization of the inverted T wave may reflect myocardial ischemia, so further evaluation of older athletes is necessary.
Features that distinguish athlete's heart syndrome from cardiomyopathy
Indicator |
Sports heart |
Cardiomyopathy |
LV hypertrophy* |
< 13 mm |
> 15mm |
LV end-diastolic diameter |
< 60mm |
>70mm |
Diastolic function |
Normal (E:A ratio>1) |
Abnormal (E:A ratio<1) |
Hypertrophy of the septum |
Symmetrical |
Asymmetric (in hypertrophic cardiomyopathy) |
Family history |
Not burdened |
May be burdened |
BP response to exercise |
Normal |
Normal or decreased systolic BP response |
Deterioration of physical condition |
Regression of LV hypertrophy |
LV hypertrophy does not regress |
* Range A from 13 to 15 mm is undefined. Range A from 60 to 70 mm is undefined. Ratio E:A is the ratio of early and late flow velocities through the mitral valve.
Normal results
Physiological and morphological adaptations of the heart of aerobically trained athletes include a slowing of the heart rate, a systolic ejection murmur at the upper, left edge of the sternum, a third heart sound, a lateral shift in the point of maximum impulse, and a hyperdynamic pulse in the carotid arteries. Athletes who primarily engage in isometric training (weightlifters) will not experience these changes.
Even at rest, systolic flow murmurs may be heard in athletes, but they are soft, occur early in systole, and radiate superiorly rather than laterally to the apex. Although fixed splitting may be noted in the supine position in nonathletes, this splitting is especially noticeable in athletes. Thus, the finding of fixed splitting should be considered abnormal only if it is heard in the sitting or standing position.
What do need to examine?
How to examine?
Differential diagnosis
Pathological conditions in which echocardiographic (or cardiac magnetic resonance) reference values overlap with the physiological indices of an athlete's heart include HCM, dilated cardiomyopathy, and arrhythmogenic right ventricular cardiomyopathy (ARVC) (Figure), all of which are known to be important causes of sudden death in young people and athletes, and for which disqualification from intense sports is justified to create a safer athletic field.[ 12 ] Such differential diagnoses can present a serious clinical dilemma, given that an athlete's heart is considered benign without the development of cardiac symptoms or arrhythmic risk and would not in itself warrant disqualification from participation in athletic competition. However, overdiagnosis of cardiovascular disease in athletes may have the paradoxical effect of unnecessary exclusion from competitive sport, resulting in significant loss of psychological investment in (and enjoyment of) competition, reduced quality of life, and even loss of economic opportunity.
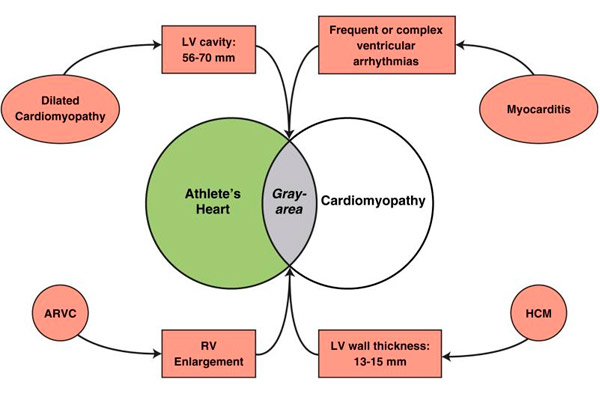
Differential diagnosis between athlete's heart and cardiovascular diseases.
The overlap between physiological LV hypertrophy and pathological conditions is shown in gray. ARVC = arrhythmogenic right ventricular cardiomyopathy; HCM = hypertrophic cardiomyopathy; LV = left ventricle; RV = right ventricle.
In the case of HCM, the differential diagnosis with athlete's heart most often occurs when the LV wall thickness is in the ambiguous "gray zone" of overlap between the extremes of athlete's heart and the mild HCM phenotype, being 13–15 mm (12–13 mm in women). [ 13 ], [ 14 ]
In such cases, the diagnosis can often be made by using noninvasive markers. HCM is preferred in the presence of LV end-diastolic cavity <45 mm, identification of a pathogenic sarcomere mutation or a family history of HCM, unusual LV wall thickness including non-contiguous segmental hypertrophy, abnormal LV filling/relaxation, particularly marked left atrial enlargement or late gadolinium enhancement on cardiac magnetic resonance. Athlete's heart is more likely when the LV cavity is enlarged (≥55 mm), [ 15 ] peak VO2 is >110% of predicted, or when LV thickness or mass decreases with short periods of strain. [ 16 ], [ 17 ]
Who to contact?
Treatment of the athletic heart
There is no need to treat athlete's heart, although a 3-month inactivity interval may be required to detect regression of left ventricular hypertrophy to differentiate this syndrome from cardiomyopathy.[ 18 ] Such an inactivity interval may significantly interfere with the athlete's life plans and cause resistance.
Forecast
Although the structural changes in the heart are pronounced and resemble those seen in some heart diseases, no adverse effects develop. In most cases, the structural changes and bradycardia regress after training is stopped, although up to 20% of elite athletes have residual chamber dilation, which is debatable because there is a lack of long-term data on whether athlete's heart is truly a benign condition.

