Medical expert of the article
New publications
Hyperplastic gastritis: symptoms, treatment, diet, prognosis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
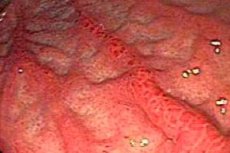
Hyperplastic gastritis is a morphological type of chronic gastric disease, in which pathological changes in the gastric mucosa are caused by increased proliferative activity of its cells. This can lead to certain structural and functional disorders and is often accompanied by inflammation of the gastric mucosa.
Epidemiology
In clinical gastroenterology, hyperplastic gastritis is considered a relatively rarely detected pathology of the stomach, which – among chronic gastric diseases – accounts for approximately 3.7-4.8% of diagnosed cases.
For example, according to the Journal of Clinical Investigation, giant hypertrophic gastritis affects both children and adults; in adults, this rare form of gastric mucosal pathology develops between the ages of 30 and 60, and this condition is detected three to four times more often in men than in women.
But polypous hyperplastic gastritis, for reasons that are still unclear, much more often affects the gastric mucosa of 40-45 year old women.
Causes hyperplastic gastritis
If, as a result of an endoscopic examination of the stomach, areas of increased mitosis of the cells of the mucous membrane lining its cavity are detected, gastroenterologists can make a diagnosis of hyperplastic gastritis.
The key morphological feature of this type of stomach lesion is the proliferation (hypertrophy) of the mucous membrane – due to an increase in glandular epithelial cells and a change in their arrangement, as well as a disruption of the normal folded structure of the mucous membrane (allowing the internal surface of a healthy stomach to increase after eating). In this case, the appearance of thicker, less mobile (rigid) folds is observed, preventing normal peristalsis of the stomach. And in the loose submucous (submucous) layer of the surface of various parts of the stomach, containing elastin fibers, hypertrophic nodes of various sizes (single or multiple) or polypoid formations are often found.
The digestion process and physiological functions of the stomach are extremely complex, and the specific causes of hyperplastic gastritis continue to be studied. The etiology of hyperplastic processes that occur in the stomach over a long period of time is associated with a number of factors:
- disorders of general metabolism that negatively affect the process of regeneration of the gastric mucosa;
- the presence of autoimmune pathologies (pernicious anemia);
- infection with cytomegalovirus and activation of the Helicobacter pylori bacteria;
- disruption of neurohumoral and paracrine regulation of the production of mucoid secretion by mucocytes of the mucous membrane and fundic glands of the stomach;
- peripheral blood eosinophilia (due to parasitic diseases, such as ascariasis, anisakiasis or lymphatic filariasis);
- genetically determined predisposition to polyposis of the fundic glands of the stomach and adenomatous polyposis (which is caused by mutations in the β-catenin and APC genes);
- autosomal dominant Zollinger-Ellison syndrome, which involves mutations in the MEN1 tumor suppressor gene;
- various congenital anomalies of the stomach and differentiation of its tissues (for example, Cronkhide-Canada syndrome ).
Risk factors
Experts name such risk factors for the development of hyperplastic gastritis as eating disorders; allergies to certain foods; deficiency of essential vitamins; toxic effects of alcohol and carcinogenic compounds, severe renal failure and hyperglycemia. And when treating hyperacid gastritis and gastroesophageal reflux disease with potent drugs that inhibit acid secretion (Omeprazole, Pantoprazole, Rabeprazole, etc.), the risk of activating the growth of polyps that appear in the areas of the main glands and foveoli (gastric pits into which the ducts of the glands exit) increases. Probably, such localization of the pathological process is associated with the fact that the regeneration of the gastric mucosa when it is damaged occurs precisely due to the cells of the mucosa covering the areas of the gastric pits.
Pathogenesis
Experts also associate the pathogenesis of atrophic-hyperplastic gastritis of the body and antrum of the stomach in cases of prolonged use of the above-mentioned proton pump inhibitors with the possibility of developing nodular hyperplasia of neuroendocrine enterochromaffin-like cells (ECLS).
In almost 40% of cases, hyperplastic gastritis in a child has the form of lymphocytic gastritis with erosion and the presence of T-lymphocyte infiltrates (CD4 and CD8 T-cells) in the upper layer of the gastric mucosa. This pathology is found with greater frequency in children with gluten intolerance (celiac disease) or malabsorption syndrome.
The pathogenesis of hyperplastic gastritis is seen in the excessive number of epithelial cells of the gastric mucosa secreting gastric mucus. Apparently, this occurs due to increased production of the mitogenic polypeptide TGF-α (transforming growth factor alpha), the molecules of which bind to epidermal growth factor receptors (EGFR), stimulating the division of cells of the gastric mucosa and the production of mucin, while simultaneously inhibiting the synthesis of acid by parietal cells.
Symptoms hyperplastic gastritis
The symptoms of hyperplastic gastritis are non-specific and vary greatly, but gastroenterologists include the following in the list of possible clinical manifestations of this pathology: heartburn, belching with a rotten taste, plaque on the back of the tongue, nausea, increased gas formation, pain in the epigastric region (aching, pressing or spasmodic), vomiting.
However, the disease often proceeds latently, and the first signs of almost all types of hyperplastic gastritis are an unpleasant feeling of heaviness in the stomach that occurs shortly after eating (especially if the food is fatty and spicy, and the level of acidity of gastric juice is increased).
Thus, with erosive-hyperplastic gastritis, patients complain of stomach pains, which can become stronger when walking or bending the body. Some have exacerbations of the disease in the spring with the appearance of blood in the stool (melena). Blood can also be in the vomit.
In most cases of giant hypertrophic gastritis, there are no symptoms. However, some patients may experience pain in the pit of the stomach, nausea with vomiting, and diarrhea. Also noted are loss of appetite and body weight, hypoalbuminemia (low albumin content in blood plasma) and associated swelling of the stomach tissue. Gastric bleeding is also possible.
Forms
There is currently no unified classification of hyperplastic gastritis, but gastroenterologists use the so-called Sydney classification system for gastritis (which was adopted by the participants of the 9th World Congress of Gastroenterology).
Experts emphasize that – regardless of localization, severity and stage (exacerbation or remission) – this is chronic hyperplastic gastritis. In domestic gastroenterology, the following types of this pathology are distinguished:
- Focal hyperplastic gastritis or nodular endocrine cell hyperplasia is the development of a basally located benign gastric carcinoid tumor (<1-1.5 cm in size) that occurs as a result of hyperplasia of endocrine enterochromaffin cells, the proliferation of which is stimulated by hypergastrinemia (excess of the hormone gastrin). Most often, this pathology is observed in patients with chronic atrophic gastritis, vitamin B12 deficiency (pernicious anemia), and also with mutations of the MEN1 tumor suppressor gene (leading to multiple endocrine neoplasia).
- Diffuse hyperplastic gastritis is diagnosed in cases where hypertrophic changes in the gastric mucosa of any etiology are multiple in nature.
- Superficial hyperplastic gastritis is characterized by the involvement in the pathological process of only the upper single-layer prismatic epithelium of the gastric mucosa.
- Polypous hyperplastic gastritis, which many specialists define as atrophic-hyperplastic, and officially it is called multifocal atrophic gastritis with focal hyperplasia. The appearance of multiple polyps consisting of glandular tissue cells on the mucous membrane of the walls of the stomach is associated with Helicobacter pylori infection, as well as with hypochlorhydria and hypergastrinemia of autoimmune etiology. As a rule, the pathology begins to manifest itself in adulthood; it has both focal and diffuse forms.
- Erosive-hyperplastic gastritis or lymphocytic-erosive gastritis (which has already been mentioned above) is characterized not only by leukocyte infiltrates in the gastric mucosa and hypertrophy of its folds. Nodular formations and areas of chronic erosion of the mucosa (especially in the area of the foveolae of the cardiac, fundic and pyloric glands) can also be observed. In this case, the level of acidity of the gastric juice can be different.
- Hyperplastic granular gastritis (or granular) is classified as focal hypertrophy of the mucosa, when multiple 1-3 mm hemispherical growths are formed on it, causing the mucosa to swell and become lumpy. At the same time, rigidity of its muscular plate, submucosa, as well as folds of the mucous and muscular membrane of the stomach is noted. The typical localization is the antral section, the mucosa of which has a large number of additional secretory cells with granular cytoplasm and inclusion of mucous granules that produce mucous secretion. According to clinical observations, this pathology is more often detected in middle-aged men.
- Hyperplastic reflux gastritis is accompanied by the reflux of the contents of the duodenum into the stomach, which causes the mucous epithelium of the stomach to be damaged by components that are part of the duodenal secretion (in particular, bile acids).
- Antral hyperplastic gastritis or rigid antral gastritis manifests itself in the disruption of the physiologically normal relief of the mucous membrane, up to a change in the direction of the folds, as well as in the presence of polypous formations on their surface. Because of this, the main and parietal cells of the fundic glands can atrophy, which leads to achlorhydria (cessation of hydrochloric acid production). In addition, the pyloric part of the stomach is deformed and becomes narrower and gastric peristalsis decreases.
Among the rare hereditary pathologies, giant hypertrophic gastritis is noted - chronic hypertrophic polyadenomatous gastritis or Menetrier's disease. It is characterized by hypertrophy of the mucous membrane in the gastric pits and a significant increase in gastric folds, insufficient secretion of HCl and excessive production of protective gastric mucin. Low levels of hydrochloric acid lead to the inability to digest proteins and absorb nutrients, causing diarrhea, weight loss, peripheral edema of soft tissues. However, since inflammation is minimal or absent, Menetrier's disease is classified in medical literature as a form of hyperplastic gastropathy.
Finally, there is active hyperplastic gastritis, which has three degrees of leukocyte (neutrophilic) infiltration of mucosal hyperplasia foci. In essence, this is chronic hyperplastic gastritis, in which the severity of the inflammatory process, determined by histological examination of tissue samples, is ranked depending on the scale of penetration of polynuclear T-cells into the structures of the gastric mucosa.
Complications and consequences
The most common consequences and complications of hyperplastic gastritis:
- changes in the structure of the gastric mucosa with atrophy of varying degrees of severity;
- damage and reduction in the number of parietal cells, decreased acid synthesis and deterioration of the digestive functions of the stomach;
- atony and impaired gastric motility, leading to persistent dyspepsia and partial gastroparesis;
- hypoproteinemia (decrease in serum protein levels);
- anemia;
- weight loss.
Advanced hyperplastic granular gastritis threatens the development of gastric ulcer and even cancer. Giant hypertrophic gastritis leads to hypochlorhydria; experts note the ability of this form of pathology to degenerate into a cancerous tumor of the stomach.
Focal hyperplasia of enterochromaffin-like cells of the mucosa can also lead to gastric carcinoma. Polypous hyperplastic gastritis, according to some data, becomes malignant in almost 20 cases out of a hundred.
Diagnostics hyperplastic gastritis
The main method on which the diagnosis of hyperplastic gastritis is based is endogastroscopy (endogastroduodenoscopy). Endoscopic instrumental diagnostics allows not only to visualize pathologically altered areas of the gastric mucosa, but also to perform a biopsy: to take tissue particles for subsequent histochemical examination. Radiography, ultrasound of the stomach, and electrogastrography are also used.
Laboratory tests are carried out, for which the following analyses are taken:
- clinical and biochemical blood analysis;
- blood test for eosinophils;
- IF blood test for the presence of Helicobacter pylori;
- gastric juice to determine pH level;
- blood test for gastric cancer tumor marker CA72-4;
- stool analysis.
What do need to examine?
How to examine?
What tests are needed?
Differential diagnosis
Differential diagnostics are carried out in order to distinguish all the mentioned types of gastric mucosal hyperplasia from other gastritis, gastroduodenal diseases and gastric oncopathologies.
Who to contact?
Treatment hyperplastic gastritis
Today, symptomatic treatment of hyperplastic gastritis is carried out, which takes into account the etiology of the disease, its type and main manifestations. And, of course, the level of acidity of gastric juice.
If the test for H. pylori is positive, a course of eradication of the bacteria is prescribed, including the azalide antibiotic Azithromycin (Sumamed) - three days, two capsules (1 g), as well as the antibacterial drug of the macrolide group Clarithromycin (Aziclar, Claricin) - for 14 days, 500 mg twice a day. Side effects of these drugs include problems with the stomach, gallbladder and intestines, headache, tachycardia, paresthesia, etc.
If pH <5-6, medications are needed to reduce acid secretion: Ranitidine tablets (0.3 g once a day); Quamatel (20 mg twice a day); Misoprostol (Cytotec) - one tablet three times a day.
Products containing bismuth subcitrate (Ventrisol, Bismofal, De-Nol Sucralf, etc.), as well as aluminum compounds (Gelusil, Compensan, Gastal, etc.) protect the damaged mucous membrane from the effects of gastric acid. Bruscopan and Pirenzepin (Gastrocepin, Gastril, Riabal) help relieve pain. For more information on the dosage, contraindications, and side effects of these drugs, see the article Tablets for stomach ulcers and the article Tablets for abdominal pain.
In case of mucosal atrophy, doctors recommend taking vitamin P and B vitamins, especially cyanocobalamin (B12). Methionine can be used to correct the condition associated with hypoproteinemia (0.5-1.5 g three times a day for two to three weeks).
For this pathology, homeopathy offers a multi-component remedy for parenteral and internal use (daily or every other day) - a solution in ampoules of Mucosa compositum.
Surgical treatment can be performed in cases of severe focal and polypous hyperplastic gastritis, as well as in cases of periodic gastric bleeding.
And how physiotherapy treatment is carried out is described in detail in the publication - Physiotherapy for chronic gastritis
A diet for hyperplastic gastritis of the stomach has great therapeutic potential – as with most diseases of the digestive system, read the article – Diet for gastritis
Folk remedies
Traditional treatment for hyperplastic gastritis involves herbal treatment in the form of decoctions and water infusions, which are prepared at the rate of a tablespoon of plant material per 200-250 ml of water.
Most often, herbal medicine recommends using: chamomile (flowers), plantain (leaves), calendula (flowers), cinquefoil and thyme (herb).
A decoction of the roots of Orchis bifolia and loosestrife acts as an enveloping agent (taken 50-60 ml three times a day). And an infusion of Ivan-tea (fireweed), taken a tablespoon 4 times a day, helps relieve inflammation of the gastric mucosa.
More information of the treatment
Prevention
For now, prevention concerns only the order and regularity of nutrition, which should be five times a day and include slightly more protein products. It is important to have a sufficient amount of vitamins (but in vegetables and fruits without coarse fiber) and water (at least five glasses a day).


 [
[