Medical expert of the article
New publications
Complications of meningitis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Inflammation of the meninges, especially in severe forms, can have long-term consequences and be life-threatening, and many complications of meningitis are irreversible and lead to disability. [ 1 ]
Epidemiology
According to WHO data based on research, the majority of patients (70%) with bacterial meningitis experience hydrocephalus, and the resulting serious disorders occur in almost 90% of patients.
It is also noted that the development of neurological complications occurs more often with meningitis of bacterial etiology. With damage to the meninges by Streptococcus pneumonia bacteria and the development of pneumococcal meningitis, mortality reaches 20%, and complications such as brain damage, paralysis, and learning disabilities are observed in 25-50% of surviving patients.
In children, hearing loss is a complication after pneumococcal meningitis in 14-32% of cases. This complication is observed, on average, in 13.5% of patients with meningococcal inflammation of the meninges and in 20% of cases of meningitis caused by Haemophilus influenzae.
Causes complications of meningitis
Infectious disease specialists and neurologists associate the causes of the development of meningitis complications with dysfunction of cells (including neurons) when they are damaged by toxins and antibodies circulating in the blood of meningococci (Neisseria meningitidis), pneumococci (Streptococcus pneumoniae), streptococci Streptococcus agalactiae group B, Listeria monocytogenes, Haemophilus influenzae, Escherichia coli, enteroviruses of the Picornaviridae family, Coxsackie and ECHO viruses, Paramyxoviridae, Herpes simplex, Varicella zoster. [ 2 ]
By overcoming the blood-brain barrier, they can penetrate not only the membranes of the brain and the subarachnoid space, but also its parenchyma.
In addition, a more aggressive reaction of the immune cells of the microglia and the dura mater plays a certain role in the alteration of neurons during the invasion of infection and the inflammatory process it induces: antibodies (IgG and IgM) produced to destroy bacteria or viruses can enhance the humoral intrathecal (subthecal) immune response, leading to cell damage and the development of various psychoneurological consequences. [ 3 ]
Risk factors
The following key risk factors for the development of serious complications of meningitis are noted:
- old age and childhood (especially the first year of life);
- immunodeficiency states;
- severe form of meningitis, in particular purulent;
- rapid clinical course of the disease;
- long prodromal period of the inflammatory process;
- impaired consciousness at the first manifestations of the disease;
- late detection of the disease due to delays in seeking medical help;
- untimely or inadequate treatment of febrile intoxication syndrome and meningitis itself – with delayed initiation of antibiotic therapy.
Pathogenesis
The mechanism of damage to cerebral structures and the central nervous system, that is, the pathogenesis of the development of complications in inflammation of the soft membranes of the brain of bacterial and viral origin, is considered in the publications:
- Acute bacterial meningitis
- Tuberculosis of the meninges (tuberculous meningitis)
- Viral meningitis
- Enterovirus meningitis
- Serous meningitis
- Purulent meningitis
For example, the mechanism of accumulation of cerebrospinal fluid (CSF) in the ventricles of the brain (hydrocephalus) in bacterial – including tuberculous – meningitis is explained by the fact that the outflow of CSF after its exit from the fourth ventricle of the brain is impeded by the blockage of the villi of the arachnoid (arachnoid) membrane of the brain by exudate in the median and lateral openings (openings of Magendie and Luschka) of the subarachnoid space.
And hydrocephalus, edema and focal purulent infiltrates of brain tissue lead to their necrosis and cause headaches, problems with vision and memory, convulsions, impaired coordination, etc.
Symptoms complications of meningitis
In case of complications of meningitis, symptoms appear that are caused by the nature, localization and degree of damage to the cells of the membranes and brain matter – after the disappearance of acute inflammation and symptoms of meningeal syndrome. Although the first signs that the disease will cause complications and long-term consequences may appear during the acute phase. This is heaviness in the head and poorly relieved cephalgia, as well as increased intracranial pressure (intracranial hypertension), which manifests itself as nausea and vomiting, sweating attacks, general weakness, diplopia (double vision), clouding of consciousness and can lead to the formation of a brain hernia. [ 4 ]
One of the clinical manifestations of bacterial meningitis is seizures, and when they occur within the first three days and are difficult to suppress, the patient is likely to experience persistent neurological complications.
In addition to hydrocephalus, numerous systemic and neurological complications of bacterial meningitis, including complications of meningococcal meningitis and pneumococcal meningitis, can manifest as:
- cerebral edema; [ 5 ]
- impaired coordination of movements and balance - vestibulo-ataxic syndrome; [ 6 ]
- convulsions and epileptic seizures; [ 7 ]
- partial or complete sensorineural hearing loss associated with paralysis of the VIII pair of cranial nerves (n. vestibulocochlearis); [ 8 ]
- deterioration or loss of vision due to inflammation of the optic nerve (II pair of cranial nerves – n. opticus); [ 9 ]
- speech disorders - bulbar dysarthria; [ 10 ]
- problems with memory and concentration, indicating cognitive impairment; [ 11 ]
- the formation of effusion between the arachnoid and dura mater - subdural empyema, [ 12 ] which can lead to a brain abscess, [ 13 ] and in fungal cryptococcal meningitis - to cryptococcoma; [ 14 ]
- the spread of inflammation to brain tissue, leading to meningoencephalitis, which often causes irreversible cerebral damage;
- meningeal cerebral coma.
Complications of tuberculous meningitis include basal adhesive or optic-chiasmatic arachnoiditis with seizures and visual impairment due to damage to the optic nerve and its membranes; formation of a tumor-like granulomatous formation in the brain – meningeal tuberculoma; arteritis (inflammation of the walls) of small or large vessels. [ 15 ] As doctors explain, extensive vascular complications in patients with meningeal damage by Mycobacterium tuberculosis occur as a result of cerebral infarction (such as ischemic stroke) in the area of the middle cerebral and basilar arteries, brainstem and cerebellum. Their consequences are manifested by neurological disorders, which may decrease over time.
Although the development of cerebral hypertension with inflammation of the meninges of viral origin is less common than with a bacterial infection, complications of viral meningitis in the form of hydrocephalus and cerebral edema may occur during the acute phase of the disease. But as the condition improves, the risks of long-term consequences also decrease, but they still develop. And this is meningoencephalitis, brainstem encephalitis, inflammation of the myocardium (heart muscle), flaccid paralysis and muscle weakness, paroxysmal headaches, sleep and memory disorders, mild cognitive impairment.
Complications and consequences
The main complications of purulent meningitis [ 16 ], [ 17 ] include:
- hydrocephalus and cerebral edema;
- damage to the cranial nerves with partial paralysis (paresis) of the limbs, speech disorder, decreased perception of visual signals;
- development of inflammation of the walls of the ventricles of the brain – ventriculitis; [ 18 ]
- cerebral vascular thrombosis and cerebral infarction;
- empyema and abscesses of the brain;
- cerebral atrophy;
- septicemia and sepsis with rapid development of septic shock and DIC syndrome in children (disseminated intravascular coagulation).
In addition to increased intracranial pressure, the development of hydrocephalic and convulsive syndromes, complications of serous meningitis include optic neuritis.
Characterizing the complications of meningitis in children, practicing doctors and researchers note that in newborns it leads to severe consequences in approximately 20-50% of cases. The most common complications are hydrocephalus, hearing and vision loss, prolonged seizures, epilepsy, inhibition of psychomotor development, and dysfunction of brain structures.
In older children, against the background of cerebral edema and hydracephaly (which can develop at the onset of the disease or several weeks after the diagnosis of bacterial meningitis), speech apparatus dysfunctions are possible due to damage to the cranial nerves and focal neurological deficit; hemiparesis, mental changes and decreased cognitive functions. [ 19 ]
Diagnostics complications of meningitis
Doctors of various specializations take part in the diagnosis of complications of meningitis, but a study of the neuropsychiatric sphere of each patient is mandatory. [ 20 ]
Basic tests include blood tests – general, biochemical, antibody levels; analysis of cerebrospinal fluid.
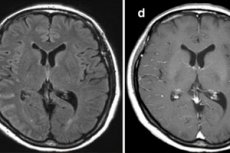
With the help of computer and/or magnetic resonance imaging (MRI) of the brain, instrumental diagnostics of complications of meningitis of any etiology is carried out. Ultrasound echoencephalography and electroencephalography are also used; in case of hearing problems, tympanometry and electrocochleography are used, etc.
Differential diagnosis
Differential diagnostics may be required, in particular to identify other pathogenetic factors of the existing symptoms, for example, cerebral tumors.
Who to contact?
Treatment complications of meningitis
Despite the high mortality rate, adequate treatment of systemic and neurological complications and aggressive antimicrobial therapy in the treatment of meningitis are essential to improve therapeutic outcomes.
Thus, in the treatment of cerebral edema it is necessary to: monitor respiratory function and intracranial pressure, control hyperventilation of the lungs, and administer a solution
Osmotic diuretic (Mannitol) and intravenous corticosteroid injections. Extensive cerebral edema can also be treated surgically by draining the cerebral ventricles (decompressive craniotomy).
Treatment of mild hydrocephalus may include drug therapy with diuretics and steroids, but in its obstructive form, drainage of cerebrospinal fluid is used, which can be done by temporary or permanent placement of a ventricular (ventriculoperitoneal) shunt or by endoscopic ventriculostomy of the third ventricle.
If the brain abscess cavity is surgically accessible, then it is drained.
For persistent seizures, anticonvulsants are used - antiepileptic drugs (Carbamazepine, Phenytoin, Gabapentin, etc.).
Speech disorders are treated by speech therapists; in addition, nootropics are used to treat bulbar dysarthria – drugs that are neurometabolic stimulants: Piracetam, Ceriton, Finlepsin, etc.
Cochlear implants are used to improve hearing, which are inserted into the ears. [ 21 ]
Prevention
To prevent neurological complications of bacterial meningitis, the most effective is primary prevention of infections: epidemic surveillance and vaccination of children against meningococci of serogroups A and C, Haemophilus influenzae, vaccination against pneumococcal infection, vaccination against meningococcal infection.
Forecast
It is difficult to predict the outcome of systemic and neurological complications of meningitis of any etiology, given the fairly high mortality rate of this disease - up to 30%.

