Medical expert of the article
New publications
Adenotomy
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
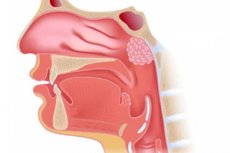
Removal of hypertrophied nasopharyngeal lymphoid tissue - adenotomy or adenoidectomy - belongs to the common operations in ENT surgery and is one of the most frequent surgical interventions performed in children.
Anatomy
Adenoid is an overgrowth of lymphoid tissue lining the posterior wall of the nasopharynx, forming the upper part of the lymphatic ring of Waldeyer. [1] Identified from the 6th week of pregnancy, blood supply is from branches of the facial and maxillary arteries, as well as the thyroid-neck trunk. Adenoids rapidly increase in size in early childhood and reach their maximum size by age seven and then regress. [2] The relative mismatch between an enlarged adenoid pad and a small nasopharynx in the pediatric population can lead to choanal obstruction, resulting in chronic mouth breathing, sleep disordered breathing, and obstructive sleep apnea. Untreated, chronic mouth breathing is thought to affect midface growth and tooth occlusion, leading to adenoid facies. This is manifested by a chronically open mouth, protruding teeth, a high arched palate, an upturned upper lip, and loss of nasolabial fold. [3] Obstruction of the eustachian tube opening combined with the presence of increased bacterial load in the adenoid is thought to lead to biofilm formation involved in the pathogenesis of otitis media with effusion. [4], [5]
Indications for the procedure
Nasopharyngeal (nasopharyngeal) adenoid hypertrophy - adenoids - is typical in young children (with a prevalence of up to 3% of the general population), when adenoid vegetations play an important role in fighting infections. But as children grow, the lymphatic tissue of the nasopharynx becomes less important: the body forms other immune defenses.
But tissue overgrowth or hypertrophy of the pharyngeal (adenoid) tonsil has negative consequences for children: from chronic inflammation of the paranasal sinuses and nasal congestion to hearing loss and deformation of the maxillofacial bones - with the formation of malocclusion. In addition, hypertrophy of this gland is not always amenable to conservative treatment.
And indications for adenoid removal surgery include:
Adenotomy in children at adenoids 1 degree is indicated in cases of no effect of drug treatment and physical therapy - in the presence of frequent respiratory diseases with progressive obstruction of the nasal airways, inflammation of the middle ear and/or paranasal sinuses (indicating that the adenoids have become a reservoir of pathogenic bacteria causing ear infections).
Due to involution, adenoid vegetations are usually undetectable after the age of 30, but removal of adenoids in adults may be performed in case of persistent (not related to acute respiratory viral infections) nasal congestion, chronic sinusitis or otitis media, and to get rid of snoring and night apnea caused by narrowing of the upper airway due to adenoid hypertrophy. [6]
Less frequent indications for adenoidectomy include complex treatment of rhinosinusitis, hyposmia or anosmia, and suspected malignancy.
Preparation
Before the planned operation, a standard anterior rhinoscopy, an X-ray of the nasopharynx, nasal cavity and paranasal sinuses is performed. If surgery under general anesthesia is planned, an ECG is required.
The list of tests for adenotomy includes: general and biochemical blood tests; coagulogram; blood tests for RW, hepatitis and HIV; nasopharyngeal swab.
Since anesthesia is required for adenotomy, based on all the data and the age of the patient, the anesthesiologist decides on the method of anesthesia (local application anesthesia, mask or intubation general anesthesia). More details in the material - removal of adenoids in children: which anesthesia is better?
Food intake before adenoid removal is stopped 10-12 hours before the procedure.
Technique of the adenotomies
There is a wide range of adenoidectomy techniques including laser ablation, coblation, endoscopic excision, and mechanical (microdebrider) excision. Ultimately, the decision rests with the operating surgeon, as similar successful outcomes have been well documented with all of these techniques. [7]
An ENT surgeon chooses the best method (type) of this surgical intervention for each specific case. Different methods have different techniques of carrying out, and how long the adenotomy operation lasts depends on the method of their removal.
Thus, in classical adenotomy, local anesthesia is performed and traditional adenotomy instruments are used (rotary dilator, Beckman loop adenotome, nasal and nasopharyngeal forceps, adenoid curette).
Adenoid resection under visual control of an endoscope - endoscopic adenotomy (with transnasal or transpharyngeal insertion of an endoscope) - is performed under general anesthesia. The procedure can be performed with a ring knife, electrosurgical coagulator (electron knife) or a special instrument such as a rhinoscopic shaver or microdebrider. The cutting nozzle of the rhinoscopic shaver (a tip located in a hollow tube) during rotation pulverizes hypertrophic tissues, which are suctioned from the nasopharynx through the internal outlet of the tip. And this is a shaver adenotomy.
Adenoids are removed using high-frequency waves (3.5-4.0 MHz) with a radio wave scalpel (adenotome electrode) of the Surgitron surgical device (Surgitron). This is a method of radiofrequency coagulation - radiofrequency adenotomy.
Under general anesthesia through endoscopic access, cold plasma coblation of adenoids is also performed - cold plasma adenotomy or coblation adenotomy using a radiofrequency plasma generator. The electric current generated by it in the radiofrequency range, passing through the physiological solution, creates a plasma field (with a temperature not higher than +45-60˚C) around the coblator electrodes. In this case, the destruction of hypertrophic tissue occurs due to the breakage of molecular bonds by hydrogen cations (H+) and hydroxide anions (OH-). The advantages of this method include bloodlessness and painlessness, while the main disadvantages include scarring.
How adenotomy is performed by laser (by laser coagulation or valorization of hypertrophic lymphoid tissue), read in the publication - surgery for removal of adenoids by laser
Contraindications to the procedure
Although there are no absolute contraindications to adenoidectomy, palatine insufficiency must be carefully considered. Individuals with known cleft palate or concealed submucosal cleft palate are at significantly increased risk of developing palatopharyngeal insufficiency after adenoidectomy, which may result in persistent hypernasal speech and nasal regurgitation. In such individuals, partial adenoidectomy limited to the lower third of the choanae has been proposed. [8] Other relative contraindications to adenoidectomy include significant hemorrhagic diathesis and active infection. [9]
Contraindications to this surgery are:
- Age of a child under two years (in the absence of urgent indications for nasal airway obstruction);
- Acute infectious diseases (including fever and cough) and exacerbation of any chronic diseases;
- Congenital anomalies of the facial bones, as well as the presence of cleft palate;
- Hemorrhagic diseases with insufficient blood clotting;
- Severe cardiac pathologies;
- The presence of cancer.
Consequences after the procedure
After adenotomy/adenoidectomy, there is always a sore throat (primarily when swallowing) and pain in the nasopharyngeal area of varying intensity. Many people have a headache after adenotomy and the child may experience otalgia (pain in the ears) that increases at night; these are referred pains that usually resolve spontaneously. The pain resolves on its own and a short course of simple analgesics such as paracetamol and non-steroidal anti-inflammatory drugs is usually sufficient.
In addition, there may be consequences such as:
- Nasal discharge (clear, yellow or green) - runny nose after adenotomy (for several days). This discharge may run down the back of the throat and cause coughing;
- Voice change within two to six weeks - due to the disappearance of pre-existing hyponasal speech;
- Bad breath after adenotomy because of the scab;
- Nasal congestion, nasal breathing becomes difficult, and the child snores after the adenotomy.
According to otolaryngologists, runny nose, stuffy nose, bad breath and snoring after adenotomy can last about two weeks. In principle, this is normal and these effects are temporary and will pass during the healing process.
Exudative otitis media after adenotomy with subfebrile temperature may be the result of exacerbation of chronic inflammation of the middle ear in the presence of an effusion or in the case of secondary infection. And when inflammation develops, a higher temperature after adenotomy is noted.
See also - consequences after adenoid removal in children
As with any type of surgical intervention, complications are possible after the adenoid removal procedure:
- Bleeding after adenotomy, as well as bleeding that occurs during the procedure, which may require postnasal tamponade and even vascular embolization with diathermy or electrocoagulation under direct or endoscopic visualization; Postoperative bleeding is rare, and with the widespread use of diathermy and direct visualization techniques, its incidence has decreased to 0.07%. [10]
- Vomiting blood and dehydration;
- Swelling of soft tissues of the nasopharynx (including allergic);
- Postoperative scarring stenosis of the pharynx;
- Atlantoaxial subluxation (of cervical vertebrae C1-C2);
- Damage to the eustachian (ear) tube.
Atlantoaxial subluxation (Grisell syndrome) is a rare but serious complication after adenoidectomy. Preexisting weakness of the anterior spinal ligament (associated with Down syndrome) and excessive use of diathermy are recognized risk factors. Treatment includes analgesia, immobilization, and neurosurgical intervention in refractory cases. [11]
Prolonged palatopharyngeal insufficiency is rare, occurring in 1 in 1,500 to 1 in 10,000 cases. It results in hypernasal speech and nasal regurgitation. Risk factors include known cleft palate or hidden submucous cleft palate. In these cases, partial adenoidectomy with tissue preservation at the palato-pharyngeal junction should be considered to minimize the risk. In rare cases, reconstructive surgery is required to improve severe speech and swallowing disorders. [12]
In some cases, re-growth of adenoids with the need for revision adenoidectomy is noted. [13] Hypertrophy of other lymphoid tissues of the Waldeyer's ring (of which the nasopharyngeal tonsil is a part) is also possible.
Care after the procedure
The success and speed of rehabilitation after adenotomy depends largely on proper care.
Most parents of operated children are interested in whether it is necessary to take antibiotics after adenotomy? In individual cases - with high fever and thicker nasal discharge - the doctor may prescribe antibacterial drugs. Protargol drops after adenotomy are used topically; they contain silver proteinate, which has antiseptic, antibacterial, anti-inflammatory and astringent effects.
However, not all topical agents in the form of drops or sprays with antimicrobial action are suitable. In particular, Polydex nasal spray after adenotomy (containing the corticosteroid Dexamethasone, the vasoconstrictor Phenylephrine and the antibiotics Neomycin and Polymyxin B) can only be used in children over 15 to prevent inflammation and reduce nasal congestion.
Also can reduce nasal congestion anti-inflammatory nasal spray Mometasone or Nazonex after adenotomy, and it is allowed to take children over three years old. But this drug refers to corticosteroids, and they can slow healing after ENT surgery.
The main recommendations after adenotomy are to prevent nosebleeds by using anti-edema and sudorific drops after adenotomy for three to five days: naftisin or sanorin, as well as drops and nasal congestion sprays with oxymetazoline, for example nazivin, Nazol or Rinazolin.
Answering the question whether you can walk after adenotomy, doctors do not recommend going for a walk with your child in the first 7-8 days after surgery. The child needs to rest at home (mom or dad for 10-12 days is given a sick leave after adenotomy in a child), and during the week should be excluded physical activity, bathing in hot water and staying in the sun.
In addition, it is necessary to monitor the body temperature and provide the child with a gentle diet, that is, it is necessary diet after adenotomy, more information - what to eat after removal of adenoids in children?
Parents often ask doctors: "Will the child be sick with acute respiratory viruses after adenotomy?" It should be taken into account that the removal of adenoids is not associated with a decrease in the likelihood of infection with respiratory viruses, but it solves more important problems associated with pathological hypertrophy of adenoid vegetations.
Useful information in the article - adenoids in a child: treat or remove?

