Medical expert of the article
New publications
Adenoids
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
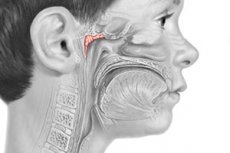
Adenoids (adenoid vegetations) - hypertrophy of the pharyngeal tonsil, which occurs under certain circumstances. Most often observed in children aged 2-10 years.
The pharyngeal tonsil, as part of the Waldeyer-Pirogov lymphoid pharyngeal ring, possessing all the properties of immunocompetent organs, performs an important protective and immunological function in the adaptation of the body to environmental factors.
Epidemiology
Adenoids are diagnosed in more than 90% of children of early and preschool age. In the absence of appropriate treatment of adenoiditis as a response to any inflammatory process of the upper respiratory tract, they increase in size relatively quickly, leading to a sharp disruption of nasal breathing and the development of concomitant diseases of the ENT organs, as well as other organs and systems of the body.
Chronic adenoiditis, accompanied by hypertrophy of the pharyngeal tonsil, mainly affects children from 3 to 10 years old (70-75%), the rest of the diseases occur at older ages. Hypertrophy of the pharyngeal tonsil can occur in mature, elderly and even old age, but these age categories account for an average of no more than 1% of cases.
Causes adenoids
In young children, hypertrophy of adenoid tissue up to a certain age can be attributed to a physiological phenomenon reflecting the formation of a protective system on the path of penetration of microorganisms with a stream of air into the upper respiratory tract.
Being part of a single barrier structure, adenoid tissue first responds to infectious effects by mobilizing compensatory capabilities. Over time, the process of physiological regeneration of lymphoid tissue is disrupted, and the number of atrophic reactive and then regenerating follicles gradually begins to increase.
The causes of adenoids are varied, but most often they are based on an infection that penetrates the parenchyma of the tonsil from the outside (for example, with mother's milk infected with staphylococcus) and causes its protective hypertrophy. Often, rapid growth of adenoids is provoked by childhood infections (measles, scarlet fever, whooping cough, diphtheria, rubella, etc.). In 2-3% of cases, adenoid vegetations can be infected with MBT in children with tuberculosis of various localizations. A certain role in the occurrence of adenoids can be played by syphilitic infection. Thus, A. Marfan out of 57 infants with a clinically established diagnosis of "adenoid vegetations" found congenital syphilis in 28, and in 11 children the presence of this disease was determined as highly probable. However, most often hypertrophy of the pharyngeal tonsil and developing chronic adenoiditis occur with lymphatic diathesis, which is characterized by systemic morphological and functional changes in the lymphatic organs, manifested by absolute and relative lymphocytosis in the blood, an increase in the lymph nodes and lymphoid formations of the nasopharynx. The latter circumstance favors the development of infection in the pharyngeal tonsil and its further hypertrophy. Often with lymphatic diathesis, an increase in the thymus gland is detected. As Yu.E. Veltishchev (1989) notes, children suffering from lymphatic diathesis are distinguished by a large body weight, but are pasty, with reduced resistance of the body to infections. They are pale, with delicate, easily injured skin, with cervical micropolyadenia, hypertrophied lymphoid formations of the pharynx, more and most often in the pharyngeal tonsils. They often develop acute respiratory diseases, tonsillitis, otitis, tracheobronchitis, pneumonia, and easily develop stridor. Often, adenoids in such children are combined with anemia and dysfunction of the thyroid gland. There are known cases of sudden death of children with lymphatic diathesis, which is associated with the insufficiency of the sympathetic-adrenal system and hypofunction of the adrenal cortex, characteristic of this type of diathesis. At the same time, adenoids, chronic tonsillitis and other signs of hyperplasia and insufficiency of the lymphatic system are found in close relatives.
Risk factors
Predisposing factors for hypertrophy of adenoid tissue may be age-related imperfection of immunological processes, inflammatory diseases of the pharynx, various childhood infectious diseases and increased allergization of the child's body due to frequent acute respiratory viral infections, endocrine disorders, hypovitaminosis, constitutional abnormalities, fungal invasion, unfavorable social and living conditions, radiation and other types of exposure that reduce the reactivity of the body. Enlargement of adenoids is one of the manifestations of the body's adaptation to changed conditions in response to significant functional stress as a result of frequent inflammatory processes. One of the causes of hypertrophy of the pharyngeal tonsil is considered to be disorders in the cytokine system, which serve as regulators of immunity, in particular the inflammatory process along with hypofunction of the cortical layer of the adrenal glands.
Pathogenesis
During nasal breathing, the first solitary lymphadenoid formation located in the path of inhaled air containing antigen-forming elements and a number of atmospheric harmful substances is the pharyngeal tonsil (BS Preobrazhensky and A.Kh Minkovsky considered it more correct to call this lymphadenoid formation the "nasopharyngeal tonsil") or adenoid vegetations (pharyngeal tonsil, or 3rd tonsil). A normal pharyngeal tonsil has a thickness of 5-7 mm, a width of 20 mm and a length of 25 mm. The third tonsil was first discovered in humans in vivo by J. Szermak in 1860, and the clinical picture of chronic hypertrophic adenoiditis was described by G. Luschka in 1869 and Mayer in 1870. It was Mayer who called the pathologically hypertrophied pharyngeal tonsil “adenoid vegetations”.
Macroscopically, it appears as ridges along its length, with grooves between them. The grooves end posteriorly, converging at one point, forming a kind of bag, which, according to G. Lushka, is a rudiment of the once existing pituitary canal. The pharyngeal tonsil is well developed only in childhood. At birth, the pharyngeal tonsil can present different aspects in appearance. Thus, L. Testut distinguished three types of pharyngeal tonsils in newborns - fan-shaped with small lymphoid ridges, the type of large lymphoid ridges (circum-valata) and the type with additional granules located on the surface of the lymphoid ridges.
In childhood, adenoid vegetations appear soft and elastic, but over time they become denser due to the fact that part of the lymphoid tissue is replaced by connective tissue, which is where the process of their involution begins. The pharyngeal tonsil is richly vascularized, the mucous glands located in them secrete a large amount of mucus containing leukocytes, lymphocytes and macrophages. From the age of 12, the pharyngeal tonsil begins to progressively decrease, and by the age of 16-20, only small remnants of adenoid tissue usually remain, and in adults, their complete atrophy often occurs. When pathological changes occur in the pharyngeal tonsil, it increases due to hyperplasia, i.e. true hypertrophy of lymphadenoid formations. Therefore, with hypertrophy of the pharyngeal tonsil, it retains the same morphological structure as a normal tonsil, but with certain features characteristic of chronic inflammation.
Morphologically, the pharyngeal tonsil appears as a pale pink formation located on a wide base in the area of the nasopharyngeal dome. In hyperplasia, it can reach the choanae and vomer anteriorly, the pharyngeal tubercle posteriorly, and the pharyngeal pockets and nasopharyngeal openings of the auditory tube laterally. Usually, the sizes of the hypertrophied pharyngeal tonsil are divided into degrees, determined visually during posterior rhinoscopy:
- I degree of hypertrophy (small size) - lymphadenoid tissue covers the upper third of the vomer;
- II degree (medium size) - lymphadenoid tissue covers the upper 2/3 of the vomer (level of the posterior end of the middle nasal concha);
- Grade III - completely covers the choanae (the level of the posterior ends of the inferior nasal conchae). In addition to the main, solitary lymphadenoid formation located in the dome of the nasopharynx, lateral formations arising as a result of hypertrophy of the follicular apparatus of the mucous membrane are of great clinical significance. They often fill the pharyngeal pockets and the openings of the auditory tube (tubal tonsils).

The surface of the pharyngeal tonsil is covered with the same mucous membrane as the other lymphadenoid formations. The crypts and the rest of the surface of the nasopharynx are covered with multilayered ciliated epithelium. With hypertrophy and inflammation of the mucous membrane covering the pharyngeal tonsil, it acquires a bright pink or red color, sometimes with a bluish tint, and can be covered with mucopurulent discharge, abundantly flowing down the back wall of the pharynx. The negative role of adenoids is usually not limited to the disruption of nasal breathing, but also consists in the fact that with hypertrophy of the pharyngeal tonsil, there is a disruption of blood circulation in the nasal cavity and nasopharynx, which can cause congestion not only in the nose and paranasal sinuses (as a rule), but also in the pituitary-sellar region, thereby disrupting the functions of one of the most important endocrine glands, closely associated with the hypothalamus and other endocrine systems of the body - the pituitary gland. Hence - various somatic and psycho-emotional disorders of the developing child's body.
Symptoms adenoids
The main symptoms are impaired nasal breathing and persistent runny nose. In most children, adenoids form a characteristic facial type (habitas adenoideus): an apathetic expression and pale skin, a half-open mouth, smoothed nasolabial folds, slight exophthalmos, and a drooping lower jaw. The formation of facial bones is disrupted: the dental system develops abnormally, especially the alveolar process of the upper jaw with its narrowing and wedge-shaped protrusion to the front; there is a pronounced narrowing and high position of the palate (Gothic palate - hypstaphilia); the upper incisors are abnormally developed, they protrude significantly forward and are randomly located; dental caries occurs early; the high-standing hard palate leads to a curvature of the nasal septum and a narrow nasal cavity.
Children experience slow growth, speech development, and physical and mental development. The voice loses its sonority, a nasal tone appears due to blockage of the nose from the choanae ("closed nasal tone"), and the sense of smell is reduced. Enlarged adenoids interfere with normal breathing and swallowing. Nasal functions are impaired, and sinusitis develops. Nasal discharge with constant runny nose irritates the skin of the nasal vestibule and nasolabial area, and frequent swallowing of discharge causes gastrointestinal disorders.
Prolonged shallow and frequent oral breathing causes abnormal development of the difficult cell ("chicken breast"), anemia. Restless sleep with an open mouth, accompanied by snoring. Absent-mindedness, weakening of memory and attention affect academic performance at school. Constant inhalation of unpurified cold air through the mouth leads to the development of tonsillitis, chronic tonsillitis, laryngotracheobronchitis, pneumonia, less often to dysfunction of the cardiovascular system. Congestive changes in the mucous membrane of the nasal cavity with impaired aeration of the paranasal sinuses and the outflow of secretion from them contribute to their purulent damage. Closure of the pharyngeal opening of the auditory tubes is accompanied by hearing loss of the cocductive type, the development of recurrent and chronic diseases of the middle ear.
At the same time, the general condition of children is disturbed. Irritability, tearfulness, apathy are noted. Malaise, pale skin, decreased nutrition, increased fatigue occur. A number of symptoms are caused not only by respiratory failure. They are based on a neuroreflex mechanism. These are psychoneurological and reflex disorders (neuroses), epileptiform seizures, bronchial asthma, nocturnal enuresis (enuresis), obsessive paroxysmal cough, a tendency to spasms of the vocal folds, visual impairment, chorea-like movements of the facial muscles.
The general immune reactivity decreases, and adenoids can also become a source of infection and allergy. Local and general disorders in the child's body depend on the duration and severity of the difficulty in nasal breathing.
With adenoids that fill the entire vault of the nasopharynx and prevent free nasal breathing, i.e., exclude the resonator and phonator functions of the nasal cavity, a violation of phonation is noted. Pronunciation of the consonants "M" and "N" is difficult, they sound like "B" and "D". Such pronunciation of "nasal" vowels is called closed nasality, in contrast to open nasality, which occurs with paralysis of the soft palate or its anatomical deficiency (scarring, cleft palate, etc.).
The impact of adenoids on the auditory tube - obstruction of the nasopharyngeal opening, hyperplasia of the tubal tonsil, infection of the mucous membrane of the auditory tube (chronic eustachitis, tubootitis) in the overwhelming majority of cases leads to periodic or permanent hearing loss, which causes a delay in the child's development, his absent-mindedness, and inattention. Young children, due to hearing loss of tubal genesis, have difficulty mastering speech, which is often distorted.
Constant thick, viscous nasal discharge causes irritation and maceration of the skin of the upper lip, its swelling and eczematous lesions of the skin of the nasal vestibule.
In "adenoid" children, constant breathing through the mouth causes various anomalies in the development of the facial skeleton. The shape of the upper jaw changes especially noticeably. It narrows and lengthens forward, giving it a wedge-shaped form. The alveolar process and teeth protrude forward and beyond the arch of the lower jaw, causing the upper teeth to cover the vestibular surface of the lower teeth (the so-called upper prognathia), which leads to malocclusion. The hard palate, continuing to develop, protrudes into the nasal cavity in the form of a deep depression resembling the vault of a Gothic cathedral ("Gothic" palate). At the same time, the lower jaw lags behind in development (microgenia), which further emphasizes the deformation of the facial skeleton and increases the malocclusion.
If adenoids are not sanitized in a timely manner, complications are inevitable, which manifest themselves in numerous disorders of the somatic and mental development of the child, as well as many disorders of the functions of the sense organs and internal organs. However, numerous clinical observations have established that there is no correlation between the size of adenoids and the frequency, variety and severity of complications. Often, small adenoids can provoke significant complications from various organs and systems. This phenomenon is explained by the fact that in the parenchyma of adenoid vegetations there are small but numerous abscessing follicles, which, due to the rich blood supply and lymph drainage, seed with pathogenic microorganisms not only nearby anatomical formations, but also organs and systems located far beyond the nasopharynx.
Adenoid hypertrophy is a reversible process. During puberty, they undergo reverse development, but the complications that arise remain and often lead to disability.
Where does it hurt?
Stages
There are three degrees of hypertrophy of the pharyngeal tonsil:
- I degree - adenoid tissue occupies the upper third of the nasopharynx and covers the upper third of the vomer;
- II degree - adenoid tissue occupies half of the nasopharynx and covers half of the vomer;
- Grade III - adenoid tissue occupies the entire nasopharynx, covers the vomer completely, reaches the level of the posterior end of the inferior nasal concha; much less often, enlarged adenoids protrude into the lumen of the oropharynx.
Complications and consequences
Among the complications, the most common are chronic, often aggravated adenoiditis, acute inflammation of the palatine tonsils, laryngotracheitis and pneumonia, catarrh of the auditory tube, tubootitis, acute purulent otitis media. Small children do not know how to cough up sputum that gets into the laryngeal part of the pharynx from the nasopharynx, so they swallow it. Often, due to swallowing infected mucus, they develop gastrointestinal dysfunction.
Eye complications such as blepharitis, conjunctivitis, and ulcerative keratitis are also common.
Often, adenoid growths lead to skeletal development disorders of a rickets-like nature: a narrow "chicken" chest, kyphosis and scoliosis of the spine, deformation of the lower limbs, etc. These changes are associated with frequent disruption of metabolic processes in adenoids associated with hypovitaminosis D.
Hyperplasia of the pharyngeal tonsil is usually accompanied by chronic inflammation of its parenchyma, but accumulations of pathogenic microorganisms in its grooves significantly aggravate the inflammatory process, turning the pharyngeal tonsil into a pus-soaked sponge. This sluggish inflammation is called chronic adenoiditis; it significantly complicates the course of adenoidism in children and most often leads to various purulent complications.
The inflammatory process from the nasopharynx easily spreads to the pharynx, larynx and bronchi, especially in acute catarrh and frequent and long-term inflammatory diseases of the upper respiratory tract. The flow of mucopurulent discharge into the larynx causes persistent coughing, especially at night. Regional lymph nodes (cervical, submandibular and occipital) are often significantly enlarged. Periodically occurring exacerbations of chronic adenoiditis are accompanied by an increase in body temperature, scraping local pain in the nasopharynx, an increase in mucopurulent discharge, irradiation of pain to the base of the skull, the back of the head, and the eye sockets. The pharyngeal tonsil, already hypertrophied, sharply enlarges, completely obstructing the choanae. The general condition of the child in such cases significantly worsens. The child becomes lethargic, irritable, often cries due to pain in the nasopharynx, loses appetite, and often vomits while eating.
Another complication associated with an infection nesting in the adenoids is acute adenoiditis, which is a retronasal or nasopharyngeal sore throat. In some cases, this complication occurs as a catarrhal inflammation, in rare cases - as a follicular sore throat. The disease usually occurs in young children and begins suddenly with a high body temperature (39-40 ° C). At the same time, there is complete obstruction of nasal breathing, ear pain and paroxysmal cough at night. Acute adenoiditis can occur spontaneously, in the absence of pathological hyperplasia of the pharyngeal tonsil, but most often it is the infection of the tonsil with this hyperplasia that causes the occurrence of an acute inflammatory process in it. The symptoms are usually the same as in the exacerbation of chronic adenoiditis, the difference is only in the severity of the inflammation and an even worse general condition, while the regional lymph nodes enlarge and become painful. The discharge from the nasopharynx becomes abundant and purulent. The child literally chokes on them and, unable to cough them up and spit them out, swallows them, which often causes acute inflammation of the gastric mucosa and dyspeptic disorders. The presence of a shorter and wider auditory tube in childhood contributes to the infection getting into the middle ear, especially if parents try to teach the child to blow his nose. Increased pressure in the nasopharynx during these attempts facilitates the entry of purulent discharge into the middle ear, and acute purulent otitis media occurs.
Acute adenoiditis, if no complications arise, ends, like ordinary tonsillitis, on the 3rd to 5th day with recovery with appropriate intensive treatment.
Another group of complications consists of reflex disorders, which, as A.G. Likhachev (1956) believed, may originate from the nerve receptors of the pharyngeal tonsil or arise as a result of concomitant changes in the nasal mucosa. Histological studies conducted by various authors in the mid-20th century established that the pharyngeal tonsil is supplied with numerous pulpy and non-pulpous nerve fibers, as well as receptor devices that end both in the stroma of the tonsil and in its parenchyma. These nerve formations, reacting to the air flow passing through the nasopharynx, play an important role in the morphological development of the entire anatomical region of the upper respiratory tract, since they are closely connected through vegetative structures with the hypothalamus, pituitary gland and other subcortical nerve centers that play an important role in the trophic provision of the body and the reflex regulation of its functions.
Reflex disorders may include nocturnal enuresis, headaches, asthma attacks, laryngospasm, choreiform contractions of the facial muscles reminiscent of voluntary childish grimaces, etc.
Neuropsychiatric disorders in "adenoid" children, such as memory loss, slow intellectual development, constant lethargy and drowsiness, and attention deficit disorder, are caused by the pathological influence of adenoid vegetations on the pituitary gland, which has close connections with the pharyngeal tonsil, not only mediated through nerve formations, but also direct ones due to the presence of an embryonic craniopharyngeal canal in children, originating in the so-called Lutka's bag and leading directly to the pituitary gland. Vascular connections with the anterior pituitary gland, responsible for the somatic development of the body, are carried out through this canal. Hypofunction of this lobe leads to a child's growth retardation and sexual maturation. Removal of the adenoids compensates for this deficiency and leads to the elimination of most niche-related reflex disorders.
Diagnostics adenoids
A child with a hypertrophied pharyngeal tonsil can be recognized by its characteristic appearance.
The anamnesis indicates frequent respiratory viral diseases with prolonged runny noses and subsequent subfebrile condition, progressive deterioration of the child’s general condition with damage to other ENT organs.
Physical examination
The size and consistency of adenoids are determined by posterior rhinoscopy and digital examination of the nasopharynx. The degree of adenoid growth is determined by lateral radiography of the nasal cavity and nasopharynx.
 [ 35 ], [ 36 ], [ 37 ], [ 38 ]
[ 35 ], [ 36 ], [ 37 ], [ 38 ]
Laboratory research
Clinical blood and urine tests, bacteriological examination of nasopharyngeal secretions for microflora and sensitivity to antibiotics, cytological examination of prints from the surface of adenoid tissue.
Instrumental research
Direct detailed examination of the nasopharynx is performed by the method of posterior rhinoscopy, in which adenoid vegetations are visualized as irregularly shaped formations with a wide base, located on the vault of the nasopharynx. They have 4-6 longitudinal clefts, of which the deepest is located in the middle. Less common are growths with a spherical surface, on which individual deep pockets are noted.
Adenoid vegetations in children are soft and pink. In adults, they are usually somewhat denser and paler. In rare cases, sclerotic, very dense formations are encountered. Mucous discharge filling the nasopharynx and nasal passages, swelling, or hypertrophy of the nasal conchae are visible. After anemia of the mucous membrane of the nasal cavity, during phonation, anterior rhinoscopy can show how adenoid growths move along the back wall of the pharynx. An indirect sign of the presence of adenoids is enlarged palatine tonsils and especially hypertrophied lymphoid follicles of the back wall of the pharynx. Limited mobility of the soft palate is characteristic.
Lateral radiography of the nasopharynx is an objective method for determining the degree of hypertrophy of the adenoid tissue, which also allows detecting the structural features of the nasopharynx, which is of certain importance during surgical intervention. When posterior rhinoscopy is difficult to perform in young children, digital examination of the nasopharynx is widely used.
Histological examination of adenoids shows that they consist of reticular connective tissue, the loops of which are filled with lymphocytes. Lymphocytes in different stages of karyokinetic division are visible in the germinal centers of follicles. The surface of adenoids is covered with multilayered cylindrical ciliated epithelium. In some areas, the epithelium is penetrated by emigrating lymphocytes.
What do need to examine?
How to examine?
Differential diagnosis
Differential diagnostics of adenoids is a very important stage in the examination of the patient, since the nasopharynx is the area in which numerous volumetric diseases can develop, fundamentally different from adenoids. The use of non-surgical or surgical methods used for adenoids for some of them can lead to irreparable consequences. Adenoids should be differentiated from all diseases of the nasal cavity, accompanied by difficulty in nasal breathing, mucopurulent discharge from the nose and nasopharynx, from volumetric benign and malignant tumors of the nasopharynx, specific granulomas, congenital anomalies of the nose and nasopharynx (for example, choanal atresia). Particular attention should be paid to recurrent adenoids, especially in adults. In these cases, the patient should be examined in the direction of excluding the tumor process (inverted papilloma, epithelioma, sarcoma), for which a biopsy is performed before the next surgical intervention.
Who to contact?
Treatment adenoids
Adenoids are treated with the aim of restoring free nasal breathing, preventing the development of concomitant diseases of the ENT organs, internal organs and body systems caused by frequent diseases of the upper respiratory tract and long-term impairment of nasal breathing.
Indications for hospitalization
The need for adenotomy surgery.
Non-drug treatment of adenoids
UF-tube on the back wall of the pharynx and endonasally, helium-neon laser treatment of adenoid tissue, diathermy and UHF on regional posterior cervical, postauricular and occipital lymph nodes, irrigation therapy (the so-called "nasal shower") to eliminate antigens from the mucous membrane of the nasal cavity and nasopharynx using mineral water, nasal sprays "Aqua Maris" and "Physiomer", ozone therapy, oxygen cocktails, mud therapy. Sanatorium and spa treatment (climatic and balneological mud resorts and warm seasons): vacuum hydrotherapy with undiluted sea water and iodine-bromine water, mud solution, inhalation therapy after rinsing the nasopharynx with carbon dioxide water, mud solution, phytoncides, vegetable oils, endonasal electrophoresis of mud solution, phototherapy (for example, laser radiation of the nasopharynx through a light guide or nasal cavity).
Drug treatment of adenoids
Homeopathic lymphotropic drugs: umckalor, tonsilgon, tonsilotren, yov-malysh in age-related dosages according to various schemes for 1-1.5 months. The effectiveness of lymphomyosot for adenoids has not been proven.
Surgical treatment of adenoids
Adenotomy, cryo-, laser- and ultrasound destruction of adenoid tissue.
Treatment of adenoids should be comprehensive, combining methods of local and general impact, especially in advanced cases, when an inflammatory process develops in the lymphadenoid tissue, and somatic and psychointellectual disorders are noted. Such children, according to indications, should be examined by a pediatrician, child psychotherapist, endocrinologist, internist, audiologist, phoniatrist and other specialists in accordance with the psychosomatic and functional disorders detected in him.
Treatment of adenoids is mainly surgical (adenotomy and adenectomy; the difference between these types of surgery is that with adenotomy only the hypertrophied pharyngeal tonsil itself is removed, while with adenectomy the remaining lymphoid tissue on the lateral walls of the nasopharynx that can be removed is removed), especially for grades II and III adenoids.
When is surgical treatment of adenoids indicated?
Adenotomy is performed at any age if there are appropriate indications.
In infants, surgical treatment of adenoids is mandatory in cases of nasal breathing disorders, noisy breathing during sleep (especially when stridor breathing occurs), and difficulty sucking (the child leaves the breast to "catch his breath" or refuses it altogether). Surgery is also indicated for recurrent adenoiditis, salpingootitis, tracheobronchitis, etc. In children of this age group who experience frequent otitis, long periods of subfebrile temperature not explained by other reasons, long periods of septicemia in the absence of other significant foci of infection (for example, chronic tonsillitis), neurotoxicosis (convulsions, meningismus, changes in somatic reflexes), adenotomy is allowed even during an exacerbation of chronic adenoiditis under the "cover" of appropriate antibacterial drugs.
Children aged 5-7 years are subject to surgical treatment in case of adenoid origin of difficulty in nasal breathing, phonation disorders, inflammatory diseases of the middle ear and their complications; adenotomy at this age is also performed in case of cervical adenitis, lymphatic fever or subfebrile temperature of unclear etiology, recurrent adenoamygdalitis, rhinitis, sinusitis, eye infections, laryngotracheobronchitis, gastrointestinal disorders, deformations of the facial skeleton and chest, reflex disorders (laryngeal spasms and nocturnal enuresis, paroxysmal convulsive cough, headaches, etc.).
Adenotomy in adults is performed even in cases where the lymphadenoid tissue of the nasopharynx is concentrated around the openings of the auditory tube and prevents recovery from catarrhal and purulent otitis, rhinosinusitis, and chronic bronchopneumonia.
Some foreign authors recommend that patients of all ages (with adenoids) who have undergone surgical treatment of adenoids undergo an antrocellulotomy or mastoidectomy for a more favorable course of the postoperative period of the main surgical intervention. This equally applies to surgical interventions on the paranasal sinuses.
Contraindications
Adenotomy is not performed in cases where the pharyngeal tonsil, even if enlarged, does not cause the adenoidism and complications described above. Surgical treatment of adenoids is not performed in the presence of local and general inflammatory processes of banal etiology (acute adenoiditis and tonsillitis, adenovirus infection of the upper respiratory tract, acute rhinitis, etc.). Surgery is performed 2-3 weeks after the end of these diseases. Surgery is not performed during epidemics of infectious diseases, such as influenza, as well as in the case of tuberculosis in the active phase, the presence of foci of infection in the dental and maxillary region, seropositive syphilis, decompensated conditions in diseases of the heart and kidneys, hemophilia. Surgical treatment of adenoids is postponed in the case of other diseases that can be effectively treated. Removal of adenoids in cases of congenital defects of the soft and hard palate (clefts), as well as in cases of severe atrophy of the mucous membrane of the pharynx, preosenosis and ozena lead to an aggravation of the functional and trophic disorders of the underlying disease.
 [ 39 ], [ 40 ], [ 41 ], [ 42 ]
[ 39 ], [ 40 ], [ 41 ], [ 42 ]
How is adenoid surgery performed?
Before surgical treatment of adenoids is performed, much attention must be paid to preoperative preparation, which, in accordance with generally accepted rules, includes a number of activities (unfortunately, these rules are often not fully observed and preparation for surgical treatment of adenoids is carried out according to an “abbreviated program”, which often leads to serious, sometimes fatal complications):
- They carefully collect anamnesis, find out whether the child has recently suffered from any infectious diseases, whether he has been in contact with sick children in recent weeks or whether he has been in an epidemically dangerous environment; whether the child suffers from increased bleeding, and find out hereditary characteristics;
- a series of examinations are carried out (chest X-ray, blood tests (general clinical and hemostatic indicators), urine tests, serological tests for tuberculosis and syphilis and, if indicated, other studies; throat swabs are examined for carriage of Cor. diphtheriac;
- the child is examined by a pediatrician to identify contraindications to surgery, a dentist and, if indicated, other specialists;
- If the operation is planned to be performed under general anesthesia, the child will be examined by an anesthesiologist-resuscitator the day before.
Before performing surgery, many ENT pediatricians recommend local prophylactic antiseptic treatment to prevent postoperative purulent-inflammatory complications. For this purpose, 3-4 days before the operation, the child is prescribed a 3% solution of protargol or 20-30% solution of sodium sulfacyl (albucid) in the form of nasal drops, and also 1 week before the surgery to improve hemostatic parameters - vitamin C, calcium gluconate, etc.
The operating room in which surgical treatment of adenoids is performed must be equipped with everything necessary to provide assistance in case of nasopharyngeal bleeding (posterior nasal packing, ligation of the external carotid artery), asphyxia (tongue-holder, intubation and tracheotomy kits), pain shock and collapse (a set of drugs that stimulate the activity of the cardiovascular and respiratory systems, the pituitary-adrenal cortex system, increasing blood pressure) in agreement with the resuscitator.
The following surgical instruments are required for adenotomy: a mouth gag, a tongue depressor, Beckman adenotomes of two sizes, selected according to V.I. Voyachek's rule (the volume of the nasopharynx, its width is equal to two folded lateral surfaces of the distal phalanges of the first fingers of the hands), Luke's nasal forceps, long curved scissors and Lube-Barbon nasopharyngeal forceps for infants.
To perform surgical intervention under general anesthesia, appropriate means for intubation anesthesia are required.
It is recommended to wrap the child tightly in a sheet before the operation to immobilize the limbs. The child is seated on the left thigh of the assistant, who grasps the child's legs with his shins, the child's chest with his right hand, holding his left hand, and fixing the right hand. The child's head is fixed with the left hand.
Anesthesia
In infants and children up to 2-3 years of age, surgical treatment of adenoids is performed without any anesthesia in an outpatient setting. After 2-3 years, some authors recommend short-term mask anesthesia with ether. Older children and adults are given application anesthesia by 3-4-fold lubrication of the posterior sections of the nasal mucosa and the vault of the nasopharynx with a 1-3% solution of dicaine or a 5-10% solution of cocaine. The posterior end of the vomer is anesthetized especially carefully. The posterior wall of the nasopharynx and the nasopharyngeal surface of the soft palate are also anesthetized. If for one reason or another the use of local anesthesia is impossible, then the operation is performed under intubation anesthesia.
 [ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ]
[ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ]
Adenotomy technique
Adenotomy consists of several stages:
- After pressing the tongue downwards with an angled spatula, the adenotome ring is inserted behind the soft palate, while the handle of the instrument is held so that the second finger fixes the rod of the adenotome; the adenotome ring is turned 90° relative to the surface of the tongue, moved along the spatula in the direction of the back wall of the pharynx and, having reached the soft palate, the ring is inserted behind it and turned in the opposite direction so that the blade takes a horizontal position and the arch of the ring is directed towards the mouth opening, i.e. with the cutting part towards the back wall of the pharynx.
- A complex movement of the adenotome (tilting the handle downwards, simultaneously moving the ring upwards to the vault of the nasopharynx, pressing the arch of the ring to the vomer without losing contact with the latter, raising the ring with an emphasis on the angle formed by the vomer and the vault of the nasopharynx, slightly tilting the child's head forward) provides a "starting position"
- With a quick movement along the vault of the nasopharynx, pressing the adenotome ring upward and backward, the adenoids are cut off and, together with the knife, they are taken out into the oral cavity and then into the kidney-shaped basin. During the cutting of the adenoids, the assistant or the surgeon himself tilts the child's head down, which ensures close contact of the blade with the object being removed and smooth sliding of the knife along the back wall of the nasopharynx. As soon as the adenoids are removed, the child's head is immediately tilted down so that the blood, in case of profuse but short-term bleeding, does not get into the respiratory tract, but flows out through the nose and mouth. Sometimes the removed adenoids remain on the flap of the mucous membrane of the back wall of the pharynx and hang down from behind the soft palate. They are grasped with a clamp and cut with scissors.
- After a pause determined by the surgeon, the entire procedure is repeated using a smaller adenotome to complete the "medial" adenotomy and remove the laterally located remnants of the adenoids covering the nasopharyngeal openings of the auditory tube; for this, the adenotome is inserted two more times. To prevent psychological trauma to the child, A.A. Gorlina (1983) recommends moving the adenotome from top to bottom in a zigzag pattern during the adenoid cutting stage, which achieves a more complete removal;
- Upon completion of the surgical intervention, the child is asked to blow his nose and the quality of nasal breathing is checked, while it should be borne in mind (which is established before the operation) that nasal breathing may not improve significantly due to rhinogenic causes (nasal polyps, hypertrophic rhinitis, curvature of the nasal septum, etc.). In addition, a digital examination of the nasopharynx is performed to control the thoroughness of the adenotomy. Next, an examination of the removed adenoids is performed and compared with the in vivo picture. The removed adenoids should be shown to the child's parents so that they can verify the quality of the operation, but they should also be warned that in rare cases, despite a well-done operation, relapses are possible.
 [ 48 ], [ 49 ], [ 50 ], [ 51 ], [ 52 ]
[ 48 ], [ 49 ], [ 50 ], [ 51 ], [ 52 ]
Complications after adenotomy
Complications during and after adenotomy, although rare, can cause life-threatening complications and be very difficult to manage.
The most common complication after adenotomy is bleeding, which occurs immediately after the operation or several hours after it. Under all other favorable conditions, the cause of such bleeding is incomplete removal of adenoid tissue, which may depend on the following circumstances: mismatch between the size of the adenotome and the size of the nasopharynx, insufficiently high position of the knife when cutting the adenoids, which can be determined by failure to press the arch of the ring to the vomer and insufficiently tight pressing of the blade to the upper posterior wall of the nasopharynx, and also if the patient rises during cutting the adenoids. In case of this type of bleeding, it is necessary to repeat the operation and carefully remove the remains of the adenoid tissue and all mucous membrane fragments on the back wall of the pharynx with a conchotome. If bleeding continues, it is necessary to perform posterior nasal tamponade or take other measures.
Complications of the middle ear (salpingootitis, catarrhal and acute purulent otitis media) are caused by tubal or hematogenous infection. Treatment is standard.
Postoperative increase in body temperature to 37.5-38°C without apparent cause is not uncommon and lasts no more than 2 days. If the temperature is higher and lasts longer, sepsis, diphtheria, pneumonia, or exacerbation of pulmonary tuberculosis should be suspected. The measures taken should be aimed at establishing the cause of hyperthermia and eliminating it.
Vomiting blood may occur shortly after surgery if it was swallowed during adenoid removal. The occurrence of this vomiting after a few hours indicates renewed bleeding. Such a child should be immediately taken to the hospital to determine the cause of this complication.
Sometimes the adenotome gets stuck in the nasopharynx, which makes it impossible to complete the operation and remove the knife into the oral cavity. The most common cause is excessive tilt of the head during adenoidectomy or abnormal protrusion of the anterior tubercle of the 1st cervical vertebra. In the first case, the head is returned to its initial position to remove the knife. In the second case, if the adenotome fails to be removed, the head is slightly tilted and the obstacle in the knife's path is cut off with a forced movement. There are also such incidents as a broken ring (knife) and its getting stuck in the nasopharynx. This happens when there is a material or design defect in the ring or the end of the adenotome rod to which the knife is welded. In such cases, without any haste, the metal object remaining there is felt with a finger or a Mikulich clamp, or Lube-Barbon forceps inserted into the nasopharynx, grasped and carefully removed. An unsuccessful adenotomy is immediately repeated or, if the nasopharynx was injured during the removal of a foreign body that arose during the operation, the repeat operation is postponed for 1 month.
Traumatic complications occur with rough surgical intervention. For example, with significant pressure of the adenotome on the back wall of the nasopharynx, the mucous membrane is deeply damaged and subsequently cicatricial stenosis of the nasopharynx may occur. Synechiae and cicatricial deformations of the soft palate after adenotomy occur in children with congenital syphilis. Torticollis and neck rigidity are rare and occur as a result of damage to the aponeurosis and prevertebral muscles by the adenotome with infection of the damaged tissues and the development of a post-inflammatory cicatricial process. This complication occurs in cases when during curettage the patient's head is not tilted forward and poorly fixed by an assistant, but on the contrary, the child sharply deviates it backwards, which significantly increases the natural cervical lordosis, the convexity of which falls under the blade of the adenotome. This complication gives itself away by the forced position of the child's head, which is characterized by immobility and extension of the head. Cases of atlas subluxation have also been described; the disease was called "nasopharyngeal torticollis" or Grisel's syndrome, named after the French physician P. Grisel who described it in 1930. The syndrome of nasopharyngeal torticollis is characterized by the displacement of the atlas into a position of luxation-rotation due to unilateral contracture of the prevertebral muscles. A child who had adenoid surgery the day before wakes up in the morning with his head turned and tilted to one side. Deep palpation at the angle of the lower jaw causes acute pain in the child. An X-ray of the upper cervical vertebrae reveals a sign of luxation-rotation of the atlas. The use of antibiotics, decongestants, hydrocortisone, and physiotherapy for several days leads to recovery.
Trauma to the mucous membrane of the nasopharynx can also result in atrophic epipharyngitis, which occurs after repeated adenotomies performed by different specialists for incorrect indications.
The results of the operation are positive in most children; nasal breathing is restored, existing inflammatory diseases of the upper respiratory tract are quickly eliminated, appetite returns, physical and mental activity increases, and the child's further physical and intellectual development is normalized. However, as statistics show, adenoid relapses occur in 2-3% of cases, primarily in children suffering from allergies manifested by atonic asthma, Quincke's edema, urticaria, seasonal bronchitis, etc. As a rule, adenoid relapse occurs with incomplete removal and not earlier than 3 months after the operation, and is manifested by a gradual increase in difficulty in nasal breathing and all other signs of adenoidism that were observed before the surgery. Conducting adenotomy under visual control under general anesthesia and using modern video surgical methods dramatically reduces the number of relapses.
It should be borne in mind that children after adenotomy, even with absolutely free nasal breathing, still have the habit of keeping their mouth open, especially at night. To eliminate this habit, such children undergo special breathing exercises, certain educational activities, and sometimes the lower jaw is tied with a scarf.
If a child's adenoids are treated on an outpatient basis, the child is left in the hospital for an hour (lying on a couch), during which time the child is periodically examined by a doctor or an experienced nurse to ensure that there is no bleeding, and then sent home. At home, bed rest is prescribed for 2-3 days, hot food and drinks are excluded for 7-10 days. In the following days, the child's physical activity is limited for 2 weeks, schoolchildren are exempted from classes for 2 weeks, from physical education classes for 1 month. Older children and adults after adenoid removal are kept in the hospital for 3 days with bed rest and, if indicated, appropriate symptomatic agents. To facilitate nasal breathing and remove bloody crusts that form in the postoperative period, oil drops in the nose are prescribed 3-4 times a day.
Non-surgical treatment of adenoids
This treatment of adenoids is only an auxiliary method, complementing surgical treatment. Its effectiveness in case of developed adenoids is limited to reducing inflammatory phenomena and preparing the ground for a more favorable course of the postoperative period. At the earliest stages of adenoid growths (stage I), this treatment can give positive results only with a comprehensive approach to it and, first of all, with the elimination of the cause of the disease. For this purpose, antiallergic and desensitizing treatment of adenoids is carried out, the immune functions of the body are strengthened, systematic hardening is carried out, foci of infection are sanitized, the body is saturate with vitamins A and D and microelements necessary for the harmonious development of the body. Heliotherapy, UV therapy, and, in recent years, laser therapy play a significant role in non-surgical treatment.
Further management
Observation by an otolaryngologist, breathing exercises and health-improving measures.
More information of the treatment
Prevention
Timely administration of preventive vaccinations against the most common childhood infectious diseases, hardening of the body, early diagnosis and rational treatment of inflammatory diseases of the upper respiratory tract and adenoiditis, increasing the body's immunological resistance.
Forecast
The prognosis depends on the general condition of the child, against which adenoidism developed. If the cause of adenoids was a vulgar infection, then with its elimination and removal of the adenoids the disease stops. If the cause of hyperplasia of the pharyngeal tonsil was lymphatic diathesis, then with the removal of the adenoids the systemic disease does not disappear, but may manifest itself with similar changes in another place. The prognosis for facial deformations that have arisen during the long course of the disease is determined by the age of the patient. If the removal of the adenoids is performed during the period of ongoing skeletal development, then some correction of the face shape is possible, however, this correction never reaches the ultimate effect, and the pathomorphological changes that have arisen as a result of the influence of the adenoids remain for life.
With timely diagnosis and adequate therapy, the prognosis is good in terms of stable restoration of nasal breathing and prevention of the development of concomitant diseases of internal organs and ENT organs.
 [ 63 ]
[ 63 ]

